- Department of Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
- Department of Anesthesiology, Sarkari Karmachari Hospital, Dhaka, Bangladesh
- Department of Neurosurgery, Ibn Sina Diagnostic and Consultation Centre, Dhaka, Bangladesh,
- Department of Translational Research and of New Surgical and Medical Technologies, University of Pisa, Pisa, Italy,
- Department of Neurosurgery, Neurosurgery Clinic, Birgunj, Nepal.
Correspondence Address:
Md. Kamrul Ahsan
Department of Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
DOI:10.25259/SNI_540_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Md. Kamrul Ahsan1, Md. Rashedul Hossain1, Md. Shahidul Islam Khan1, Naznin Zaman2, Nazmin Ahmed3, Nicola Montemurro4, Bipin Chaurasia5. Lumbar revision microdiscectomy in patients with recurrent lumbar disc herniation: A single-center prospective series. 25-Nov-2020;11:404
How to cite this URL: Md. Kamrul Ahsan1, Md. Rashedul Hossain1, Md. Shahidul Islam Khan1, Naznin Zaman2, Nazmin Ahmed3, Nicola Montemurro4, Bipin Chaurasia5. Lumbar revision microdiscectomy in patients with recurrent lumbar disc herniation: A single-center prospective series. 25-Nov-2020;11:404. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10409
Abstract
Background: Recurrent lumbar disc herniation (RLDH) is a common complication following primary microdiscectomy. Notably, revision surgery for recurrent disc herniation typically warrants “aggressive discectomy (AD)” rather than microdiscectomy due to the marked changes in anatomy, including postoperative scar. Here, we prospectively evaluated clinical outcomes of 22 RLDH patients following secondary aggressive discectomy (AD).
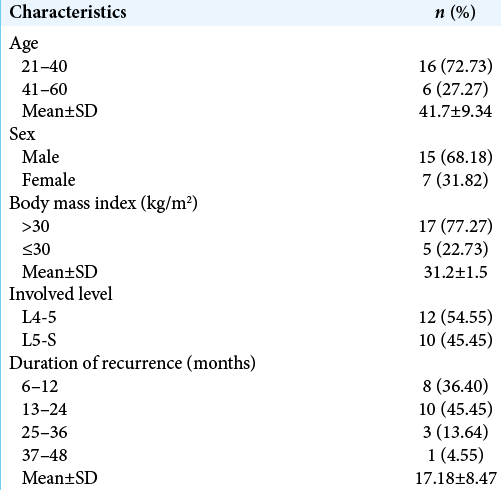
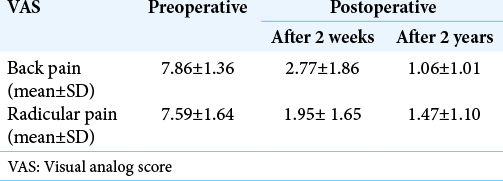
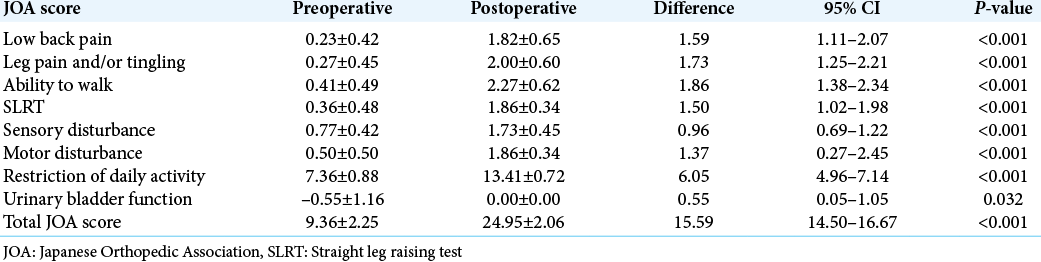
Methods: Records of 15 males and seven females averaging 41.7 years of age (range 21–60) who developed RLDH following primary microdiscectomy at the L4-5 (n = 12) and L5-S1 (n = 10) levels were studied. All patients underwent secondary AD for recurrent lesions (2014–2019). Multiple clinical parameters were assessed for these 22 patients. Outcomes were evaluated an average of 28.8 months postoperatively and included assessment of visual analog scales (VASs) and Japanese Orthopedic Association (JOA) Scores.
Results: The VAS scores for back and radicular pain significantly improved, as did the JOA scores following surgery in all 22 patients after secondary AD.
Conclusion: The authors concluded that secondary conventional revision discectomy (e.g., AD) effectively and safely managed RLDH.
Keywords: Lumbar disc herniation, Recurrent herniation, Revision discectomy
INTRODUCTION
Recurrent lumbar disc herniation (RLDH) following initial microdiscectomy is the most common cause for reoperations.[
MATERIALS AND METHODS
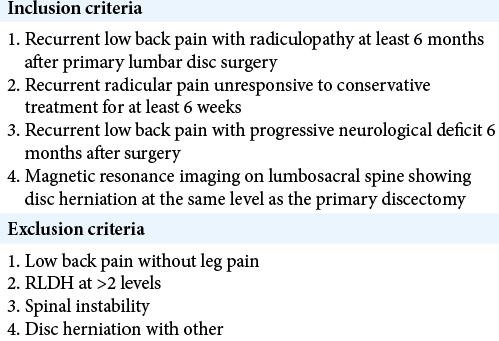
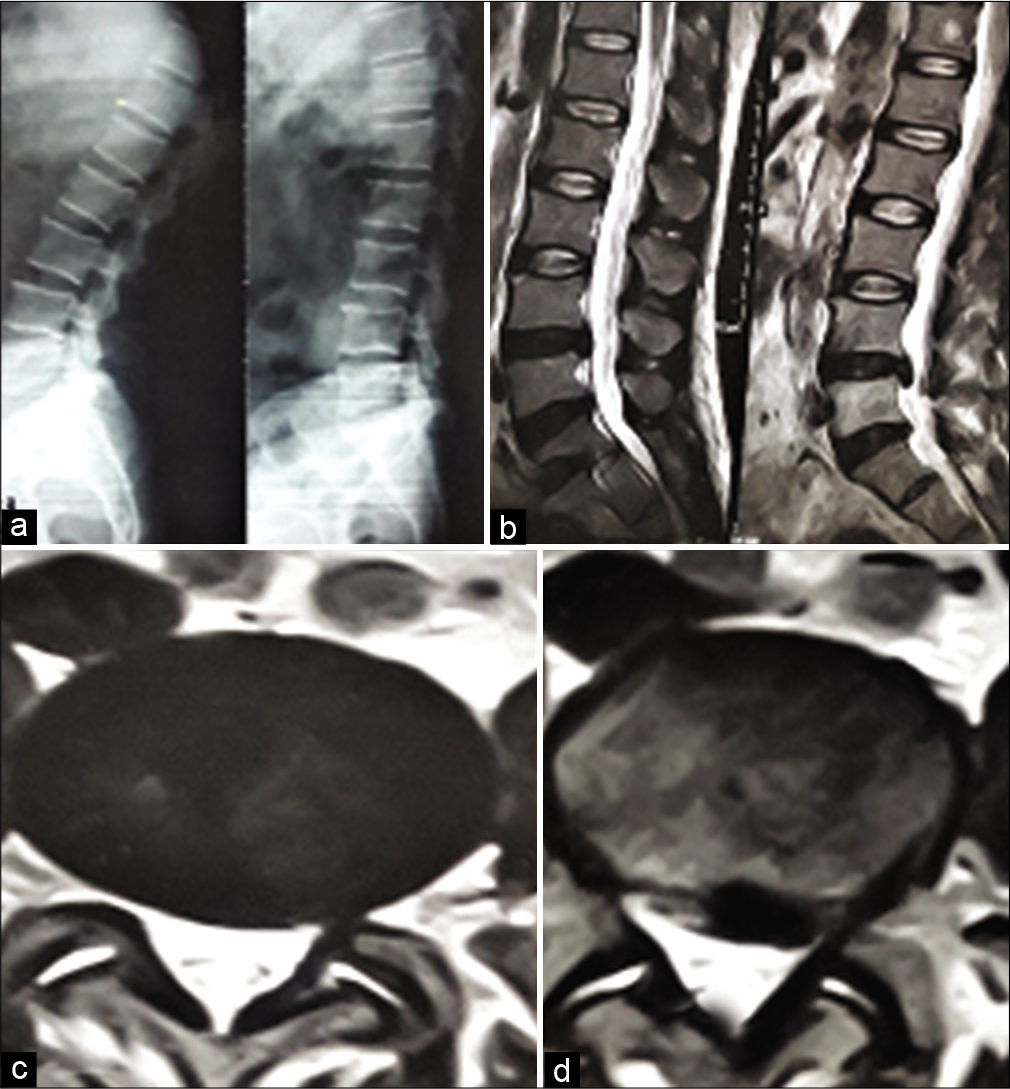
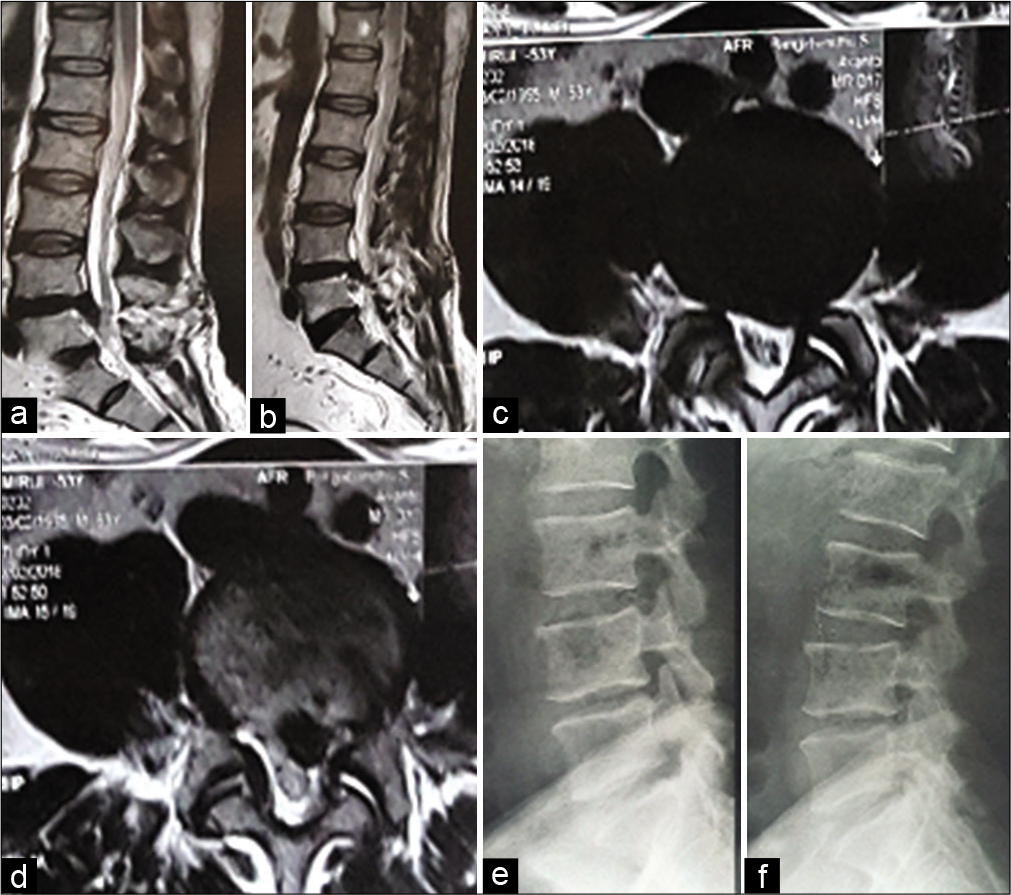
With IRB approval, we prospectively studied outcomes for 22 patients who originally underwent microdiscectomies, but secondarily whose RLDH were managed with 19 AD versus 2 simple excisions of extruded fragments (2014 and 2019) [
Statistical analysis
The quantitative data were analyzed statistically using Statistical Package for the Social Science, version 25, Armonk, NY, IBM Corp.
RESULTS
The operative time for secondary AD was 95.0 ± 9.0 min (range 65–125 min), the mean blood loss 85 ml (range, 70–150 ml), and average postoperative hospital stay was 5 days (range, 4–8 day). The mean VASs and JOA scores were significantly improved postoperatively [
DISCUSSION
Surgical options for RLDH
The main two surgical options for RLDH include revision lumbar discectomy (e.g., repeat microdiscectomy vs. AD) [
Timing of redo surgery
The typical pain-free interval between the index microdiscectomy and the RLDH is typically 6 months.[
CONCLUSION
The management of the RLDH requires following original microdiscectomy that warrants AD for better visualization and safer operative dissection (e.g., to more readily deal with postoperative scar formation).
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Dai LY, Zhou Q, Yao WF, Shen L. Recurrent lumbar disc herniation after discectomy: Outcome of repeat discectomy. Surg Neurol. 2005. 64: 226-31
2. El Shazly AA, El Wardany MA, Morsi AM. Recurrent lumbar disc herniation: A prospective comparative study of three surgical management procedures. Asian J Neurosurg. 2013. 8: 139-46
3. Kara B, Tulum Z, Acar U. Functional results and the risk factors of reoperations after lumbar disc surgery. Eur Spine J. 2005. 14: 43-8
4. Mashhadinezhad H, Sarabi E, Mashhadinezhad S, Ganjeifar B. Clinical outcomes after microdiscectomy for recurrent lumbar disk herniation: A single-center study. Arch Bone Jt Surg. 2018. 6: 397-401
5. Meredith DS, Huang RC, Nguyen J, Lymas S. Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J. 2010. 10: 575-80
6. Miwa S, Yokogawa A, Kobayashi T, Nishimura T, Igarashi K, Inatani H. Risk factors of recurrent lumbar disk herniation: A single center study and review of the literature. J Spinal Disord Tech. 2015. 28: E265-9
7. Suk KS, Lee HM, Moon SH, Kim NH. Recurrent lumbar disc herniation: Results of operative management. Spine (Phila Pa 1976). 2001. 26: 672-6