- Department of Neurosurgery, Sylhet MAG Osmani Medical College Hospital, Kajolshah, Sylhet, Bangladesh,
- Department of Neurosurgery, Kathmandu University, Kathmandu Medical College and Teaching Hospital, Kathmandu, Nepal,
- Department of Neurosurgery, Salford Royal NHS Trust, Salford, Manchester, United Kingdom.
- Department of Neurosurgery, Salford Royal Foundation Trust, Salford, Manchester, United Kingdom.
DOI:10.25259/SNI_213_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Anindya Bhowmik1, Sneha Bisht2, Ko Ko Zayar Toe3, K Joshi George4. Giant posterior mediastinal schwannoma requiring a thoracoabdominal approach for excision: Case report and literature review. 25-May-2021;12:241
How to cite this URL: Anindya Bhowmik1, Sneha Bisht2, Ko Ko Zayar Toe3, K Joshi George4. Giant posterior mediastinal schwannoma requiring a thoracoabdominal approach for excision: Case report and literature review. 25-May-2021;12:241. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10820
Abstract
Background: A schwannoma is a tumor of the peripheral nerve sheath. They are the most common benign tumor; presenting at any age, and at any site of the body and also one of the most common posterior mediastinal tumors. Posterior mediastinal schwannoma is usually identified incidentally in chest radiographs and with follow-up imaging such as CT scan. Large posterior mediastinal schwannoma usually presents with local symptoms. To confirm diagnosis and obtain local control, surgical excision is the usual approach.
Case Description: Here, we present a case of a 56-year-old female who presented with chronic low back pain. The lesion was picked up on an ultrasound scan to look at her kidneys. She was not experiencing any neurological symptoms. Excision of the tumor was made through a right thoracoabdominal approach. A WHO Grade 1 tumor was diagnosed on histology. There were no signs of recurrence in the follow-up scans.
Conclusion: Giant posterior mediastinal schwanommas are very rare with only one other reported case requiring a thoracoabdominal approach for excision. Though giant schwanommas raise concern for malignancy due to their large size, they generally turn out to be benign
Keywords: Excision, Posterior mediastinal, Schwannoma, Thoracoabdominal
INTRODUCTION
Schwannomas are one of the most common benign tumors arising from the peripheral nerve coverings. Posterior mediastinal tumors are mostly benign and most common type is neurogenic tumors accounting for 75% of the posterior mediastinal tumors.[
CASE REPORT
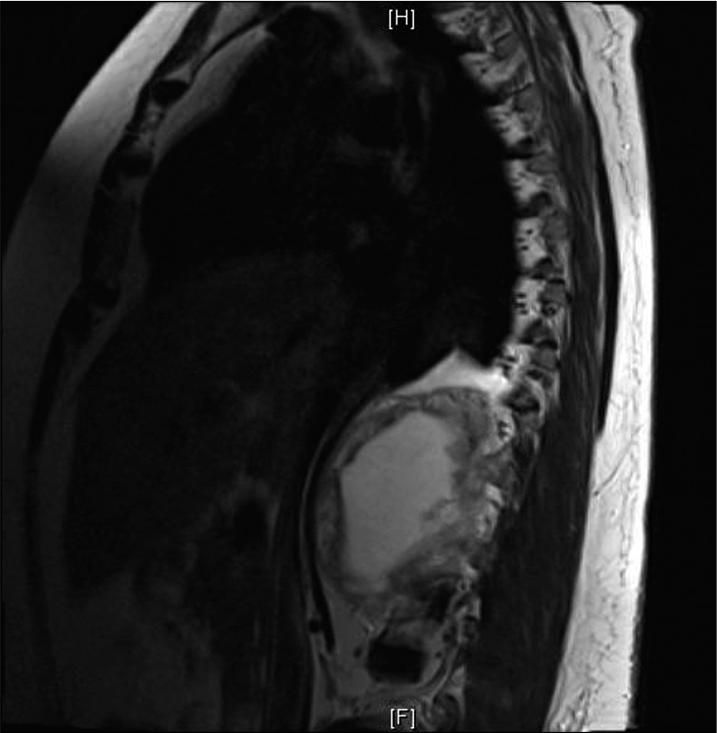
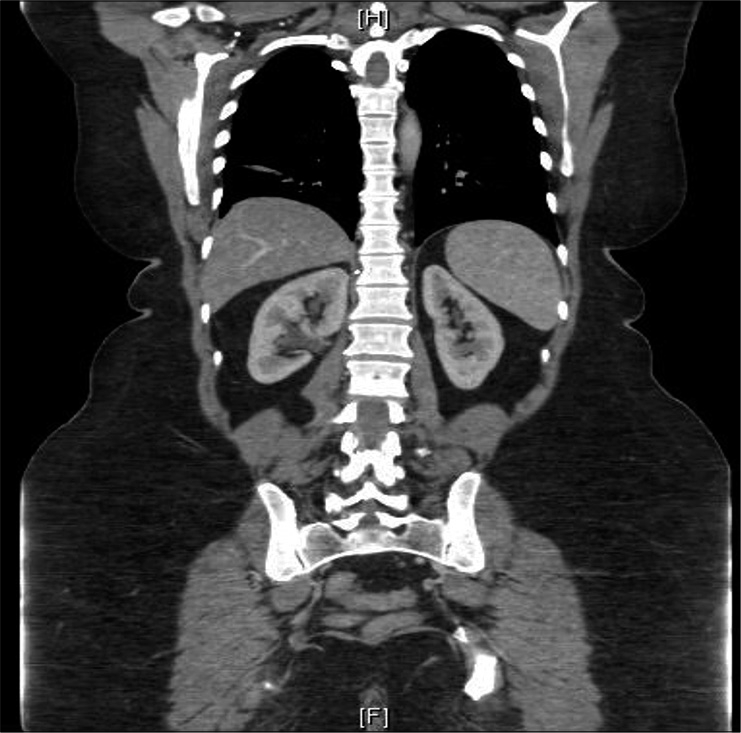
A 56-year-old lady who worked as a nursing sister presented with the chronic low back pain. She had attended in August 2016 with left-sided renal colic and this had picked up as a lesion in the right upper quadrant which was 8–9 cm in size and mainly cystic. MRI revealed thick enhancing cystic wall lesion occupying the right retroocular space [
She described the pain as aching sensation coming from her spine around the thoracolumbar region and the right side had more discomfort than the left side. She had no neurological symptoms or signs related to this although she was a bit overweight (BMI 36) and lower lumbar spine facet joint tenderness. She had no breathing difficulty and no problems with hiccups or coughing episodes.
She had underlying medical problems of the previous BCC in face and uterine fibroid.
On review, she had been suffering from on-going aching sensation in right side of the thoracolumbar region. Recent MRI showed an increase in size of the lesion [
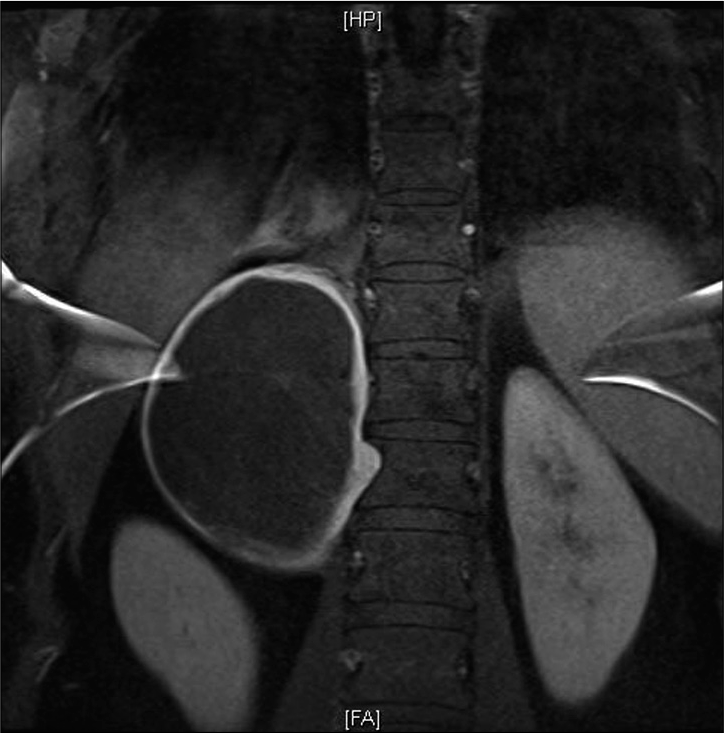
Figure 2:
Coronal sect. Large right-sided paraspinal mass lesion extending above the right kidney and displacing it. Entirely in the paraspinal tissues. It shows prominent peripheral enhancement no real central enhancement compared to surrounding muscle tissues. The adrenal is seen separate to this lesion. Scalloping of the lateral margin of T12. There is no widening of the neural exit foramen of the adjacent vertebrae. The remainder of the spine appears unremarkable.
Although initially the lesion was thought to be under the diaphragm, carefully study of the CT and MRI revealed that this was in fact above the diaphragm and arising from the right T11 nerve root [
Considering her symptoms and the large size, removing this lesion was discussed. Various operative approaches were explored. Considering that the lesion was low in the mediastinum behind the liver and kidneys, it was decided that a thoracoabdominal approach would be the optimal.
Operative procedure
She underwent a right thoracoabdominal approach for giant t11/12 nerve sheath tumor excision under GA. The procedure was performed via reverse L shaped incision over chest and mid upper abdomen. Abdomen and chest were entered and diaphragm was incised. After mobilizing the liver, adrenal and kidneys, and gross total excision of the tumor which lay above the diaphragm was done.
In the postoperative period, unfortunately, she experienced wound gaping at the epigastric area over 10 cm length without obvious sign of infection. The wound was closed back after washout on 14th postoperative and she went home 2 days after that was her 16th postoperative day.
Follow-up
Postoperative imaging showed good excision of the tumor with no residuum found [
Histology showed WHO Grade 1 Schwannoma.
DISCUSSION
Posterior mediastinal tumors are most commonly neurogenic schwannomas. They present equally in all genders and in all ages but commonly people over 40 years old have shown the most presentation.[
Symptoms
As posterior mediastinal schwannoma are mostly benign they are usually asymptomatic. They show cystic degeneration and are encapsulated.[
In this case, the patient was experiencing persistent aching sensation in the right side of thoracoabdominal region. She had no neurological symptoms or signs related to this. She was a bit overweight (BMI 36) and had lower lumbar spine facet joint tenderness. She had no breathing difficulty and no problems with hiccups or coughing episodes.
Imagıng fındıngs
Imaging such as digital X-rays, CT scans and MRIs are the usual diagnostic tools used. CT scan usually reveals a clear demarcated mass with low density, mild enhancement, and punctate calcifications.[
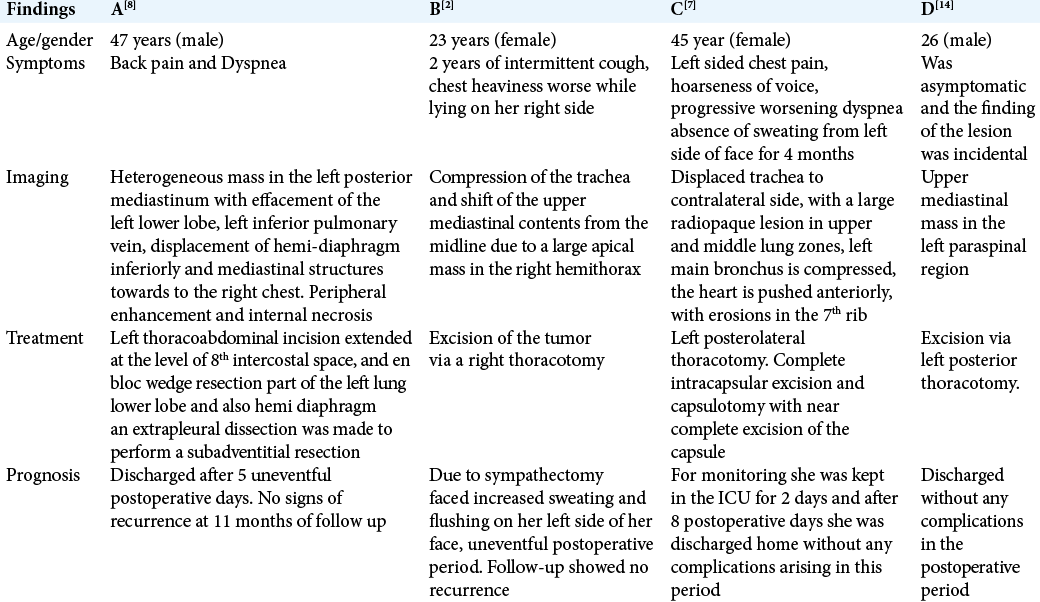
A review of the literature found only four other cases of giant posterior mediastinal schwanommas. Only one of these needed a thoracoabdominal approach for removal of the tumor [
Management and operative technique
Mediastinal schwannomas are often found incidentally and can be left alone if asymptomatic. However, if they are growing, causing symptoms or very large in size, surgery is undertaken. Large tumors have the potential for malignant transformation though they are in most cases found to be benign after excision. Small lesions in the upper mediastinum can be removed via a posterolateral approach or from a suprclavicular approach. Lesions in the mid mediastinum can be removed through a standard thoracotomy.[
In the lower mediastinum, as in our case, a thoracoabdominal approach with incising the diaphragm has to be considered, particularly if the lesion is very big. This is a major operation with some morbidity and hence reserved for cases which are symptomatic.
CONCLUSION
Posterior mediastinal giant schwannomas are rare. Their large size can raise concern for malignancy but they are usually benign. When a giant schwannoma occurs in the thoracolumbar region, careful study of the images is necessary to see if they are above or below the diaphragm. A thoracoabdominal approach can enable satisfactory excision when they are in the lower mediastinum.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest. 2005. 128: 2893-909
2. Fay KA, Finley DJ, Phillips JD. Giant posterior mediastinal schwannoma with ancient features. Curr Chall Thorac Surg. 2020. 2: 9
3. Fierro N, D’Ermo G, Di Cola G, Gallinaro LS, Galassi G. Posterior mediastinal schwannoma. Asian Cardiovasc Thorac Ann. 2003. 11: 72-3
4. Gangadharan SP, Sugarbaker DJ, Bueno R, Krasna MJ, Mentzer SJ, Zellos L.editors. Neurogenic tumours of the posterior mediastinum. Adult Chest Surgery. China: McGraw-Hill; 2008. p.
5. Hayasaka K, Tanaka Y, Soeda S, Huppert P, Claussen CD. MR findings in primary retroperitoneal schwannoma. Acta Radiol. 1999. 40: 78-82
6. Mueller DK, Mancini MC.editors. Neurogenic Tumors of the Mediastinum Treatment and Management. New York: Medscape; 2014. p.
7. Onakpoya UU, Adeniyi BO, Eyekpegha JO, Ogunrombi AB. Large posterior mediastinal schwannoma in a 45-year-old woman. Lung India. 2017. 34: 109-10
8. Quartey B, Lenert J, Deb SJ, Henry LR. Giant posterior mediastinal ancient schwannoma requiring thoracoabdominal resection: A case report and literature review. World J Oncol. 2011. 2: 181-4
9. Ribet ME, Cardot GR. Neurogenic tumors of the thorax. Ann Thorac Surg. 1994. 58: 1091-5
10. Singhal D, Kaiser LR, Nido PJ, Swanson SJ.editors. The posterior mediastinum. Surgery of the Chest. Philadelphia, PA: Elsevier Inc; 2005. p.
11. Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors: Part II. Tumors of the middle and posterior mediastinum. Chest. 1997. 112: 1344-57
12. Takeda S, Miyoshi S, Minami M, Matsuda H. Intrathoracic neurogenic tumors--50 years’ experience in a Japanese institution. Eur J Cardiothorac Surg. 2004. 26: 807-12
13. Whooley BP, Urschel JD, Antkowiak JG, Takita H. Primary tumors of the mediastinum. J Surg Oncol. 1999. 70: 95-9
14. Wu Y, Zhang J, Chai Y. Giant mediastinal schwannoma located in the lower right side of the chest. Niger J Clin Pract. 2016. 19: 678-80