- Department of Neurosurgery, King Edward Medical University, Punjab, Pakistan,
- Department of Neurosurgery, Allama Iqbal Medical College, Jinnah Hospital Lahore, Lahore, Punjab, Pakistan,
- Farooq Hospital, Westwood, Lahore, Pakistan,
- President Glasgow Neuro Society, Wolfson School of Medicine, University of Glasgow, Scotland, United Kingdom,
- Department of Neurology, Ameeruddin Medical College, Lahore, Punjab, Pakistan.
Correspondence Address:
Kashif Ali Sultan, Department of Neurosurgery, Allama Iqbal Medical College, Jinnah Hospital Lahore and Farooq Hospital, Westwood Lahore, Punjab Pakistan.
DOI:10.25259/SNI_790_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Minaam Farooq1, Biah Mustafa1, Kashif Ali Sultan2,3, Mohammad Ashraf4, Naveed Ashraf2, Abubakar Siddique3,5. Extraosseous extradural ewing sarcoma of the thoracic spine: Case report and literature review. 25-Oct-2021;12:542
How to cite this URL: Minaam Farooq1, Biah Mustafa1, Kashif Ali Sultan2,3, Mohammad Ashraf4, Naveed Ashraf2, Abubakar Siddique3,5. Extraosseous extradural ewing sarcoma of the thoracic spine: Case report and literature review. 25-Oct-2021;12:542. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11195
Abstract
Background: As part of the ‘small round-cell tumor’ family, Ewing’s sarcoma (ES) is a malignant mesenchymal tumor classified as a primitive neuroectodermal tumor (PNET). Within the PNETs, spinal extraosseous extradural lesions are exceedingly rare.
Case Description: A 19-year-old male presented with a one-month history of back pain and paraparesis with loss of urinary control. The MRI revealed an intradural, extramedullary mass at the T3-T4 level. Intraoperatively, the tumor was solely extradural, without evidence of local invasion; it was entirely removed. Due to the high risk of metastasis, the patient was subsequently treated with chemotherapy and radiation. In addition, similar studies on PNETs were reviewed.
Conclusion: A 19-year-old male presented with a paraparesis attributed to an extraosseous extradural ES at the T3-T4 level. Following total gross resection, he was successfully managed with chemotherapy and radiation. The patient has been in remission for one month.
Keywords: Ewing’s sarcoma, Extradural, Extraskeletal, Primitive neuroectodermal tumor, Spine
INTRODUCTION
Primary spinal extradural Ewing’s sarcoma (ES), also known as primitive neuroectodermal tumors (PNETs), are rare. According to the World Health Organization classification, PNET is an undifferentiated round cell tumor that arises from primitive neuroepithelial cells. They constitute a heterogeneous group of malignant tumors of childhood and early adulthood. Spinal Epidural PNET/peripheral PNET have an incidence of <1% of primary spinal tumors.[
Here, we evaluated a 19-year-old male with an extradural extraosseous T3-T4 ES managed with total gross excision, radiation, and chemotherapy, showing no evidence of recurrence a month later.
CASE PRESENTATION
Clinical presentation
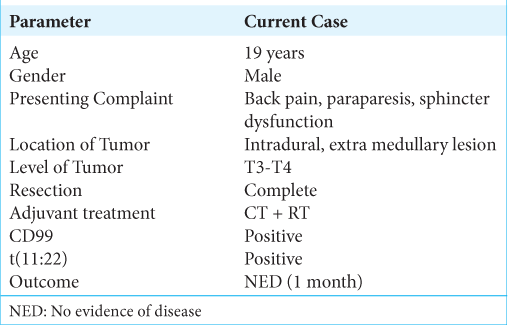
A 19-year-old male presented with a progressive T5-level paraparesis, a T5 sensory level, and sphincter dysfunction of one month’s duration [
Radiological evaluation
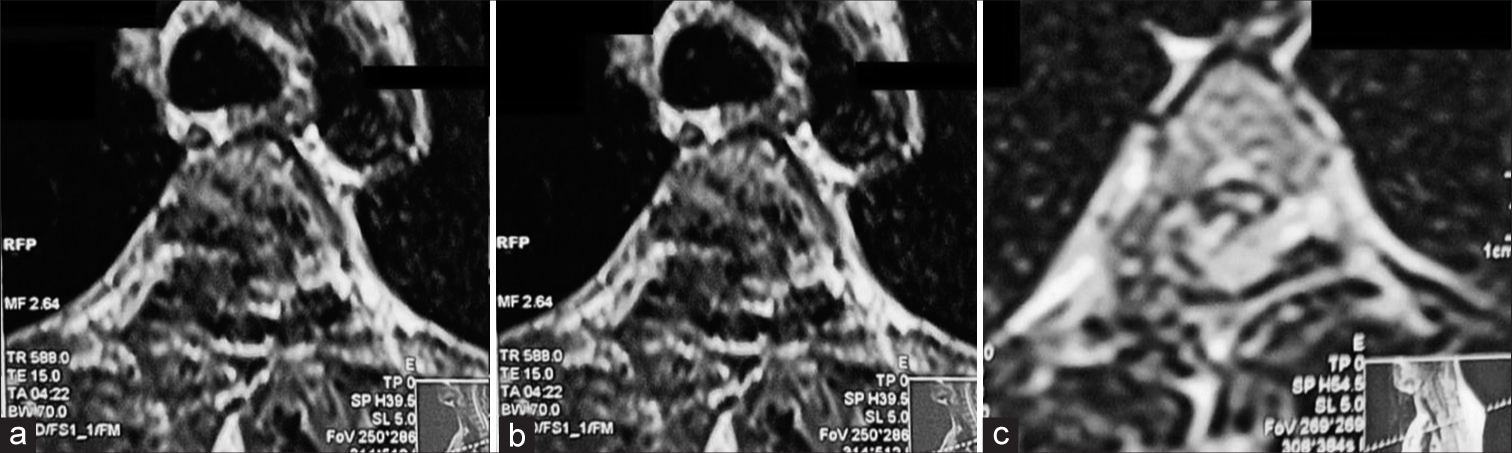
The thoracic MRI showed an intradural extramedullary lesion at the T3-T4 level; it was well-defined, predominantly right-sided with significant cord compression and lobulated, measuring 3.6 cm × 1.7 cm × 1.5 cm with “tentacles” extending superiorly. On MRI, it was isointense on T1, and heterogeneously hyperintense on T2 weighted sequences, showing partial peripheral enhancement with GadoliniumDTPA. There was also obliteration of CSF tab the level of T3/ T4 maximal compression [
Surgery
The patient underwent a T3-T4 laminectomy. The lesion proved to be entirely extradural in location and was soft and vascular; the lesion was fully excised. However, there was profuse intraoperative bleeding, requiring 1 unit of RBC transfusion.
Pathology and molecular cytogenetics confirmation of the diagnosis of epidural EWS
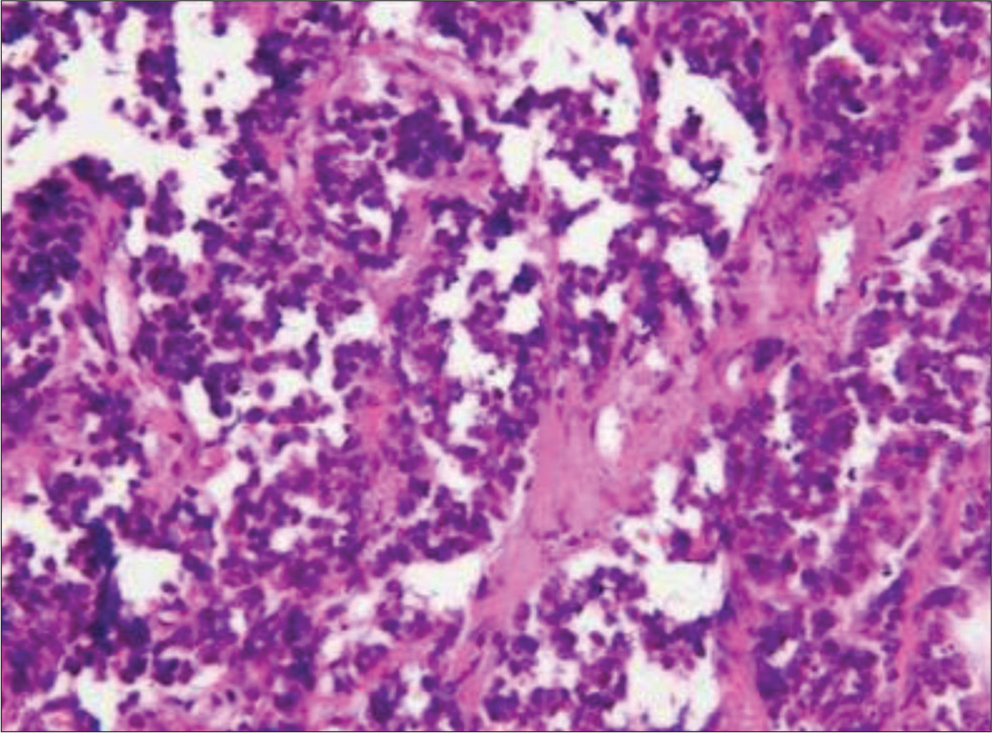
The histological examination revealed a malignant neoplasm consistent with Epidural EWS; cells were arranged in groups, sheets, and nests. Individual tumor cells were round/ oval, had uniform round nuclei and clear cytoplasm; a few cells showed a high nucleus to cytoplasm (N/C) ratio and prominent nucleoli. Atypical mitotic figures and areas of necrosis were also seen. [
Figure 3:
Immunohistochemically, the cells were positive for CD99. The complete reactivity pattern of the specimen is shown in
Molecular cytogenetics further confirmed the diagnosis, along with a fluorescence in situ hybridization analysis to assess the EWS gene locus.
Adjuvant therapy
Following confirmation, the patient was treated with a multi-agent chemotherapy regimen as well as radiation therapy.
Review of literature
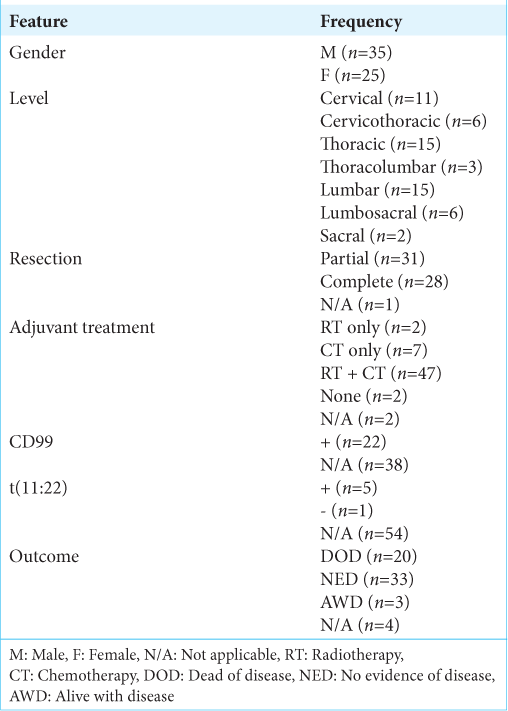
Forty-three studies have previously reported a total of 59 cases. The findings of these studies, including our current case, are summarised in [
DISCUSSION
Till today, about 40 case reports/series of extradural spinal ED have been reported, mostly occurring in adolescents and young adults and mostly in males. The most common presenting complaint is chronic back pain, paraparesis, and sphincter dysfunction later in the clinical course.
Most extradural ES involve multiple levels and may vary in location for each case, mostly presenting in the sacral region. CT scans best document dumb-bell-shaped tumors with foraminal widening,[
CONCLUSION
Extraskeletal Ewing sarcomas are exceedingly rare. The best outcomes are achieved with gross total resection, followed by adjuvant radiation and chemotherapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Allam K, Sze G. MR of primary extraosseous Ewing sarcoma. AJNR Am J Neuroradiol. 1994. 15: 305-7
2. Delattre O, Zucman J, Plougastel B, Desmaze C, Melot T, Peter M. Gene fusion with an ETS DNA-binding domain caused by chromosome translocation in human tumours. Nature. 1992. 359: 162-5
3. Folpe AL, Goldblum JR, Rubin BP, Shehata BM, Liu W, Dei Tos AP. Morphologic and immunophenotypic diversity in Ewing family tumors: A study of 66 genetically confirmed cases. Am J Surg Pathol. 2005. 29: 1025-33
4. García-Moreno R, Bernal-García LM, Pineda-Palomo M, Botana-Fernández M, Gilete-Tejero IJ, Cabezudo-Artero JM. Sarcoma de Ewing extraesquelético epidural. Caso clínico y revisión de la literatura. Neurocirugia. 2015. 26: 151-6
5. Patil AS, Gupta PP, Iratwar SW. Primary spinal extradural extraosseous primitive neuroectodermal Tumor/Ewing’s sarcoma: A critical analysis and review. Asian J Neurosurg. 2021. 16: 276-80
6. Shin JH, Lee HK, Rhim SC, Cho KJ, Choi CG, Suh DC. Spinal epidural extraskeletal Ewing sarcoma: MR findings in two cases. AJNR Am J Neuroradiol. 2001. 22: 795-8