- Department of Neurosurgery, Tokyo Women’s Medical University, Tokyo, Japan.
Correspondence Address:
Seiichiro Eguchi, Department of Neurosurgery, Tokyo Women’s Medical University, Tokyo, Japan.
DOI:10.25259/SNI_921_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Seiichiro Eguchi, Go Matsuoka, Naoki Suzuki, Tatsuya Ishikawa, Koji Yamaguchi, Takakazu Kawamata. Aspergillus sphenoiditis growth on long cut ends of a non-absorbable sellar floor dura closure suture. 23-Nov-2021;12:567
How to cite this URL: Seiichiro Eguchi, Go Matsuoka, Naoki Suzuki, Tatsuya Ishikawa, Koji Yamaguchi, Takakazu Kawamata. Aspergillus sphenoiditis growth on long cut ends of a non-absorbable sellar floor dura closure suture. 23-Nov-2021;12:567. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11248
Abstract
Background: Cerebrospinal fluid (CSF) rhinorrhea is a common complication after transsphenoidal surgery (TSS). Suturing of sellar dura is effective in the prevention of postoperative CSF rhinorrhea, but it may cause rare postoperative infections. Herein, we report a case of Aspergillus sphenoiditis with the growth noted on cut ends of a polyvinylidene fluoride (PVDF) suture used for dural closure.
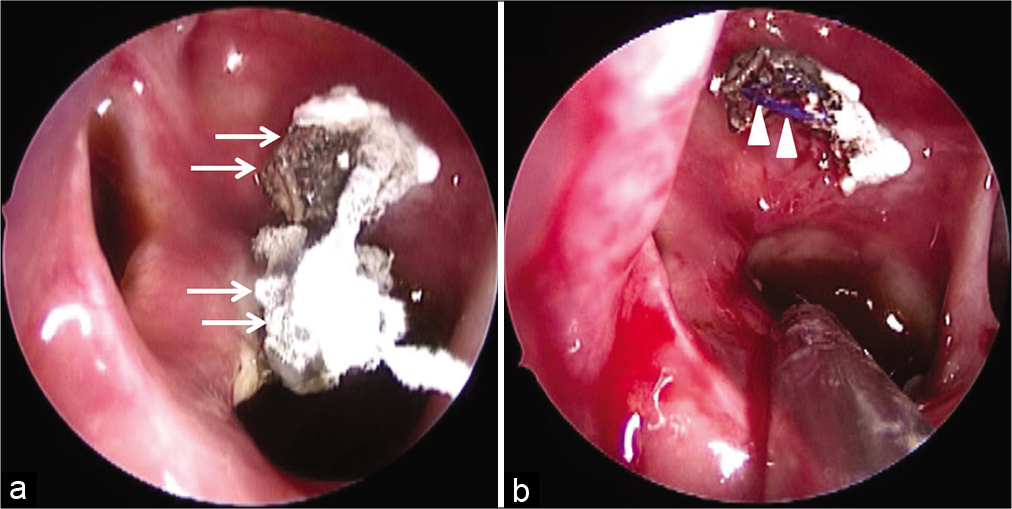
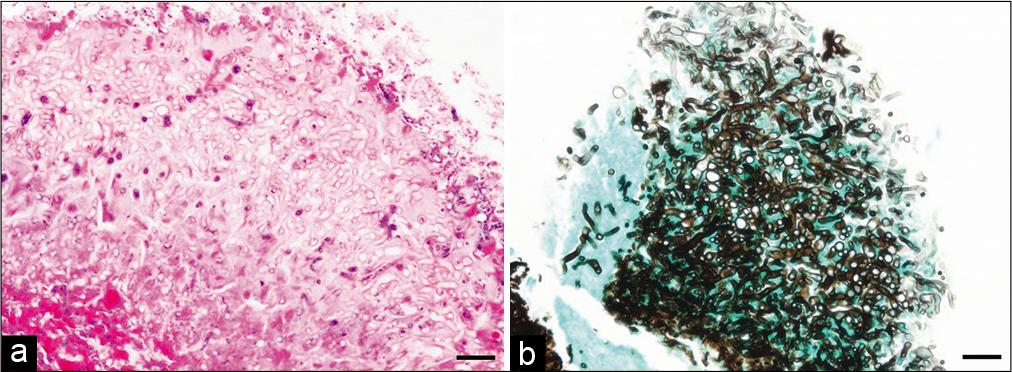
Case Description: A previously healthy 51-year-old woman complained of abnormal odor 5 years after TSS for null cell adenoma. A white mass in the sphenoidal sinus was detected on rhinoscopy. Fungal balls were found clustered around the ends of a PVDF suture used for dural closure at the initial surgery. She underwent removal of both the fungal ball and dural suture. The pathological diagnosis was Aspergillus hyphae. It is thought that a dural suture protruding out of the sphenoid sinus mucosa can cause Aspergillus infection even in immunocompetent patients. A rapid and accurate diagnosis followed by surgical removal of the fungal ball and follow-up with oral antimycotic drugs result in good clinical outcomes.
Conclusion: It is crucial to cut short the suture end and cover it with sphenoid sinus mucosa to avoid such complications.
Keywords: Aspergillus sphenoiditis, Endoscopic transsphenoidal surgery, Polyvinylidene fluoride suture
INTRODUCTION
Cerebrospinal fluid (CSF) rhinorrhea is a major complication of transsphenoidal surgery (TSS). The rate of postoperative CSF leak is approximately 10%,[
CASE DESCRIPTION
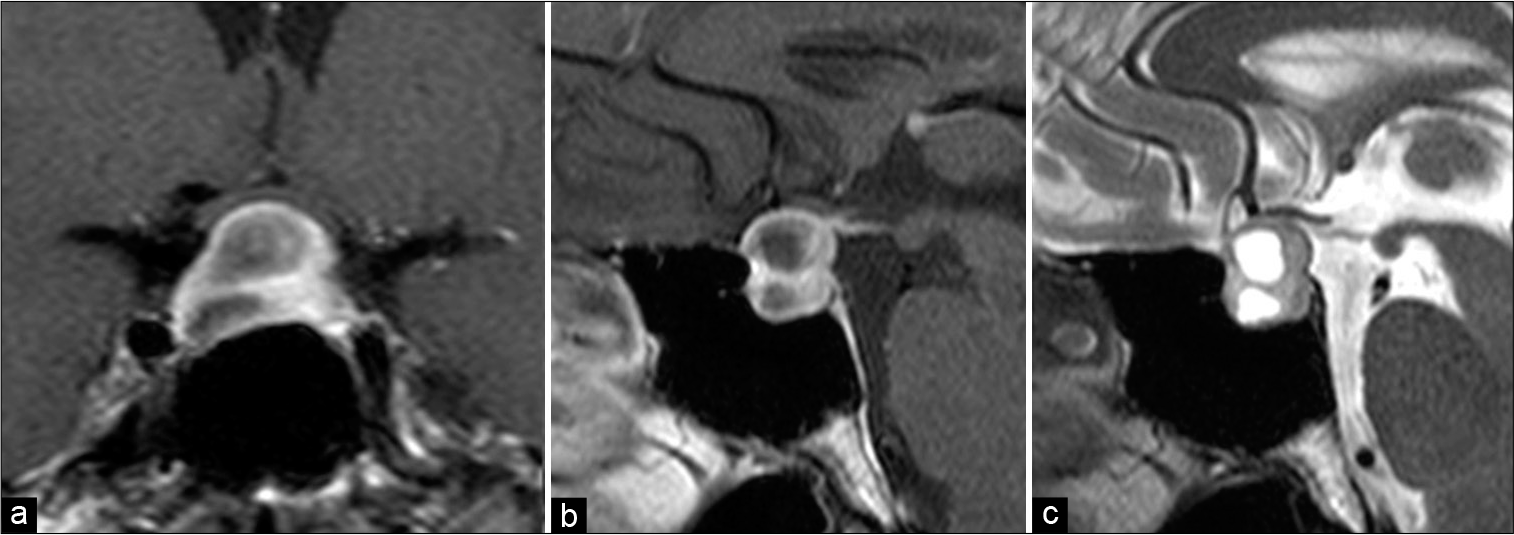
A healthy 51-year-old woman underwent a neurologic checkup because of persistent, severe headache. An intrasellar, multilobular, and cystic lesion extending to the suprasellar region was detected by brain magnetic resonance imaging (MRI) [
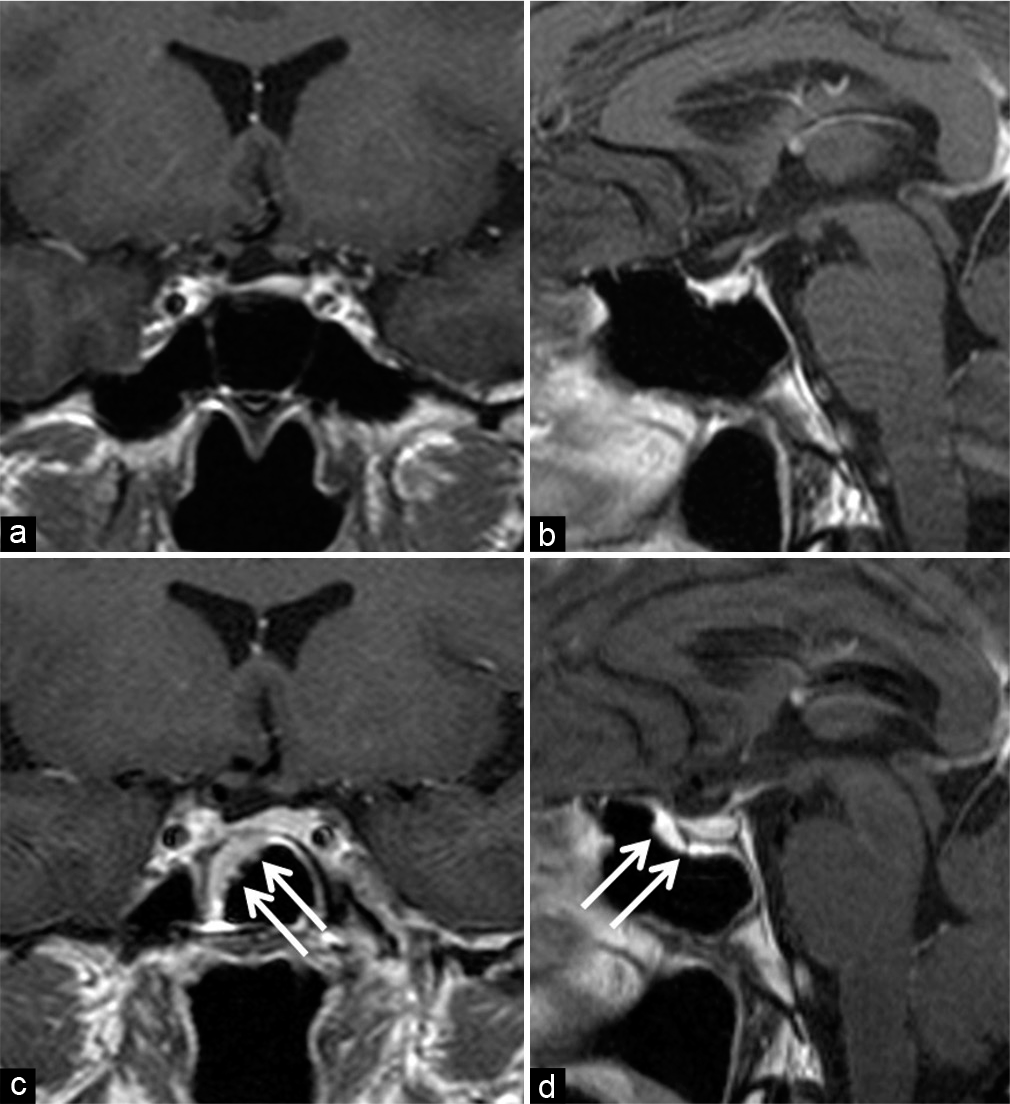
Five years after the TSS, she complained about abnormal odor and visited an otolaryngologist at a local clinic. On rhinoscopy, a white mass was detected in the sphenoidal sinus. A diagnosis of bacterial sphenoiditis was made, and daily intake of oral antibiotic drugs for 2 weeks improved her symptoms. However, after 3 months, the unusual odor recurred. Brain MRI showed a thickened sphenoid sinus mucosa, well-enhanced on T1-weighted images [
DISCUSSION
It is important to repair CSF leakage with suitable material to avoid postoperative infection because the mortality rate from bacterial meningitis is as high as 12.0%.[
In our case, the patient developed aspergilloma despite her immunocompetent state. She underwent TSS 5 years earlier, but the tumor did not secrete hormones such as adrenocorticotrophic hormone or growth hormone. She took a small dose of oral hydrocortisone for only 2 weeks during the postoperative course. Nevertheless, in her case, fungal balls of Aspergillus were detected encasing the end of the PVDF suture. PVDF is a synthetic, non-absorbable monofilament suture which is highly resistant to infection and contamination.[
CONCLUSION
Suturing the dura on the sellar floor is an effective procedure for preventing postoperative CSF leakage and its potential infectious complications. However, even in immunocompetent patients, despite using a suture more resistant to infection, when the end of the suture is left exposed in the sphenoid sinus mucosa, it may act as a nidus for postoperative fungal infections. We should cut the dural suture end short and cover it completely with sphenoid sinus mucosa when performing TSS.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
How to cite this article: Eguchi S, Matsuoka G, Suzuki N, Ishikawa T, Yamaguchi K, Kawamata T. Aspergillus sphenoiditis growth on long cut ends of a non-absorbable sellar floor dura closure suture. Surg Neurol Int 2021;12:567.
References
1. Boutarbouch M, Arkha Y, El Ouahabi A, Derraz S, El Khamlichi A. Sphenoid sinus aspergillosis simulating pituitary tumor in immunocompetent patient. J Clin Neurosci. 2009. 16: 840-1
2. Bridges KJ, Li R, Fleseriu M, Cetas JS. Candida meningitis after transsphenoidal surgery: A single-institution case series and literature review. World Neurosurg. 2017. 108: 41-9
3. Byrne M, Aly A. The surgical suture. Aesthet Surg J. 2019. 39: S67-72
4. Delevaux I, Hoen B, Kures L, Braun M, Civit T, Salloum E. Isolated invasive sphenoid aspergillosis. Presse Med. 1996. 25: 587-9
5. Dubey A, Patwardhan RV, Sampth S, Santosh V, Kolluri S, Nanda A. Intracranial fungal granuloma: Analysis of 40 patients and review of the literature. Surg Neurol. 2005. 63: 254-60
6. Ferguson BJ. Definitions of fungal rhinosinusitis. Otolaryngol Clin North Am. 2000. 33: 227-35
7. Fukui I, Hayashi Y, Kita D, Nakanishi S, Tachibana O. Aspergillus sphenoiditis associated with an artificial bone graft used for transsphenoidal surgery. NMC Case Rep J. 2015. 2: 68-71
8. Huang KT, Bi WL, Smith TR, Zamani AA, Dunn IF, Laws ER. Intrasellar abscess following pituitary surgery. Pituitary. 2015. 18: 731-7
9. Iplikcioglu AC, Bek S, Bikmaz K, Ceylan D, Gökduman CA. Aspergillus pituitary abscess. Acta Neurochir (Wien). 2004. 146: 521-4
10. Jin Y, Liu X, Gao L, Guo X, Wang Q, Bao X. Risk factors and microbiology of meningitis and/or bacteremia after transsphenoidal surgery for pituitary adenoma. World Neurosurg. 2018. 110: e851-63
11. Liu B, Wang Y, Zheng T, Liu S, Lv W, Lu D. Effect of intraoperative lumbar drainage on gross total resection and cerebrospinal fluid leak rates in endoscopic transsphenoidal surgery of pituitary macroadenomas. World Neurosurg. 2020. 135: e629-39
12. Moore LA, Erstine EM, Prayson RA. Pituitary Aspergillus infection. J Clin Neurosci. 2016. 29: 178-80
13. Nishioka H, Izawa H, Ikeda Y, Namatame H, Fukami S, Haraoka J. Dural suturing for repair of cerebrospinal fluid leak in transnasal transsphenoidal surgery. Acta Neurochir (Wien). 2009. 151: 1427-30
14. Prickett J, Altafulla J, Knisely A, Litvack Z. Invasive cryptococcal meningitis presenting as a skull base mass in an immunocompetent host: A case report. J Neurol Surg Rep. 2019. 80: e31-5
15. Sajko T, Gnjidić Ž, Sesar N, Malenica M. Sphenoid sinus aspergilloma in trans-sphenoidal surgery for pituitary adenomas. Acta Neurochir. 2015. 157: 1345-51
16. Thery A, Espitalier F, Cassagnau E, Durand N, Malard O. Clinical features and outcome of sphenoid sinus aspergillosis: A retrospective series of 15 cases. Eur Ann Otorhinolaryngol Head Neck Dis. 2012. 129: 179-84