- Department of General Practice, OneCare Medical Clinic Aljunied MRT,
- Department of Orthopedic Surgery, Sengkang General Hospital, Singapore.
Correspondence Address:
Huang Yilun, Department of Orthopedic Surgery, Sengkang General Hospital, Singapore.
DOI:10.25259/SNI_863_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yu Bin Ariel Choy1, Daniel Nim Cho Chan2, Hao Bin Chen2, Huang Yilun2. Acute L1 chalkstick fracture post fall in a patient with known ankylosing spondylitis and previous instrumentation and fusion of T8-L1. 30-Nov-2021;12:589
How to cite this URL: Yu Bin Ariel Choy1, Daniel Nim Cho Chan2, Hao Bin Chen2, Huang Yilun2. Acute L1 chalkstick fracture post fall in a patient with known ankylosing spondylitis and previous instrumentation and fusion of T8-L1. 30-Nov-2021;12:589. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11252
Abstract
Background: Patients with ankylosing spondylitis (AS) are especially prone to sustaining spinal fractures. A 72-year-old male with AS had a previous T10/11 chalkstick fracture requiring a T8-L1 fusion 1 year ago. He subsequently presented with a newly diagnosed acute chalkstick fracture of L1 which was treated without surgery.
Case Description: A 72-year-old male with AS and a T10/11 chalkstick fracture had undergone a T8-L1 thoracolumbar fusion 1 year ago. He newly presented after a fall from his bed with a new acute L1 chalkstick fracture that was successfully managed nonsurgically.
Conclusion: Patients with AS are at high risk for spinal fractures. Here, elderly male, following an original T10/11 chalkstick fracture and a T8-L1 fusion 1 year ago, presented with a new acute L1 chalkstick fracture managed without surgery.
Keywords: Ankylosing spondylitis, Chalkstick fracture, Fall, Lower back pain, Spinal instrumentation and fusion
INTRODUCTION
Ankylosing spondylitis (AS) is one of the spondyloarthropathies. These patients may develop structurally unstable chalkstick (or carrot stick) fractures (i.e., fractures occurring in a brittle spine), which is a poor prognostic finding.[
CASE REPORT
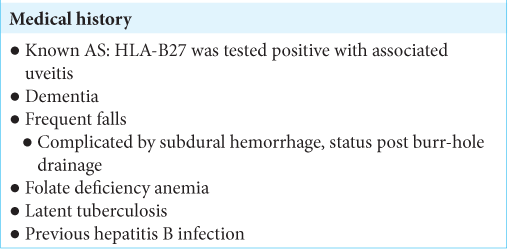
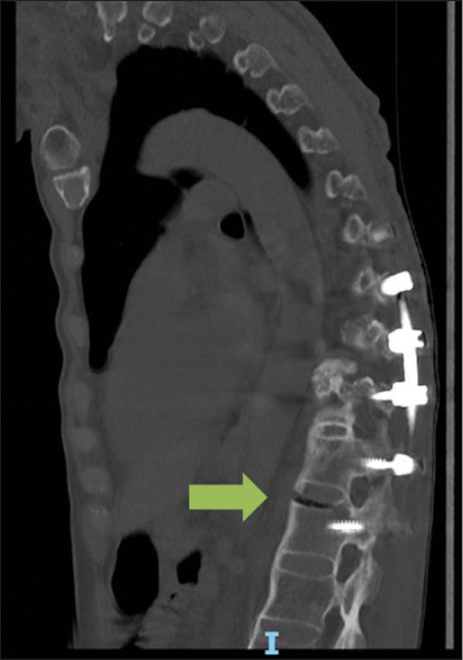
A 72-year-old male with a complex medical history [
Radiological studies
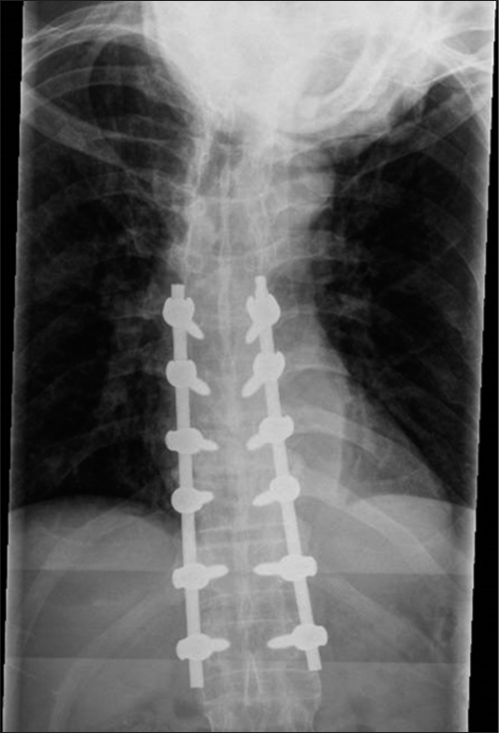
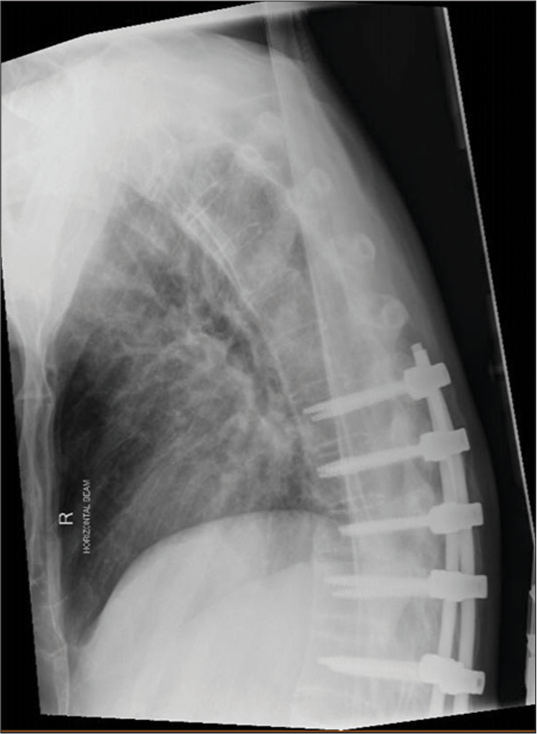
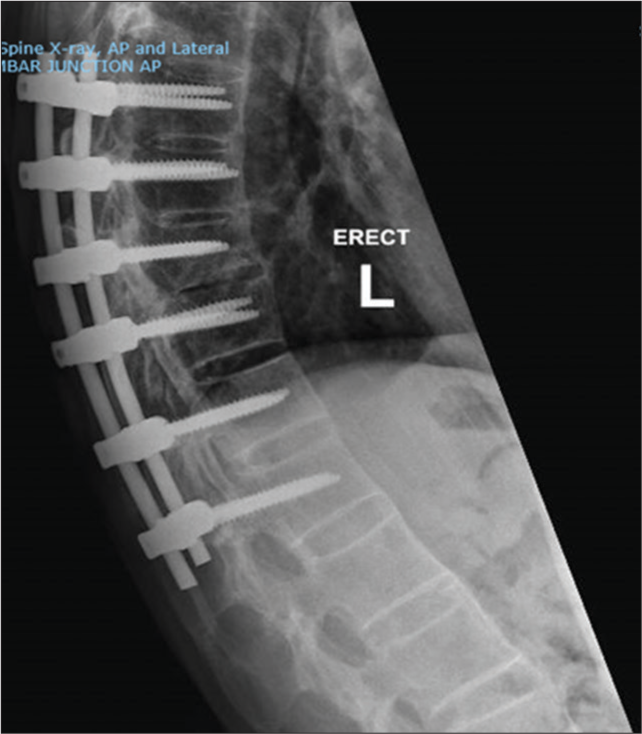
Lumbar X-rays showed AS, a loss of height of T10 vertebral body, and new T12-L1 anterior syndesmophyte disruption [
Management
As the patient had no new neurological deficit, he was managed nonsurgically; rather, analgesia was optimized. Notably, due to his severe dementia, he was unable to tolerate a thoracic lumbar sacral orthosis. One month later, the patient’s neurological examination and X-rays remained unchanged [
DISCUSSION
As patients living with AS are up to 4 times more likely to sustain spinal fractures, they should undergo definitive diagnostic radiographic studies early in their clinical courses to determine appropriate treatment. Here, a 72-year-old male presented with a second L1 chalkstick fracture 1 year following the previous T10/11 chalkstick fracture and T8/ L1 fusion. This time, without any neurological deficits, it was elected to treat him nonsurgically. Notably, a systematic review involving 76 Medline and EMBASE articles (345 AS patients) revealed no significant differences in mortality rates <3 months after presentation with AS-related chalkstick fractures (4.9% with surgery vs. 7.3% without surgery).[
CONCLUSION
Patients with AS have an increased susceptibility to spinal fractures. Here, a 72-year-old male, 1 year following a T10/11 chalkstick fracture warranting a T8-L1 fusion, presented with a new L1 chalkstick fracture that was successfully managed nonsurgically.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Tomar SS. Chalkstick fracture: A catastrophic injury. Asian J Neurosurg. 2018. 13: 383-5
2. Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009. 18: 145-56