- Department of Neurosurgery, Madre Teresa Hospital, Belo Horizonte, São Paulo, Brazil.
- Department of Vascular and Skull Base, University of Sao Paulo, São Paulo, Brazil.
- Department of Neurosurgery, Federal Fluminense University, Niteroi, Brazil.
Correspondence Address:
Daniela de Oliveira Von Zuben, Department of Vascular and Skull Base, University of Sao Paulo, São Paulo, Brazil.
DOI:10.25259/SNI_939_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Roberto Leal da Silveira1, Daniela de Oliveira Von Zuben2, Raphael Bertani2, Jose Alberto Landeiro3. Foramen magnum meningioma approached by the midline subtonsilar approach – Revisiting Cushing’s classification of craniospinal meningiomas. 17-Feb-2023;14:56
How to cite this URL: Roberto Leal da Silveira1, Daniela de Oliveira Von Zuben2, Raphael Bertani2, Jose Alberto Landeiro3. Foramen magnum meningioma approached by the midline subtonsilar approach – Revisiting Cushing’s classification of craniospinal meningiomas. 17-Feb-2023;14:56. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12160
Abstract
Background: The management of foramen magnum meningiomas (FMMs) has been a challenge for skull base neurosurgeons. Since the initial description of a FMM in 1872, various surgical approaches have been described. Posterior and posterolateral FMMs are safely removed through a standard midline suboccipital approach. Nevertheless, we still face controversy regarding the management of anterior or anterolateral lesions.
Case Description: A 47-year-old patient presented with progressive headaches, unsteadiness, and tremor. Magnetic resonance imaging showed an FMM that caused significant displacement of the brainstem.
Conclusion: This operative video highlights a safe and effective surgical technique for the resection of an anterior foramen magnum meningioma.
Keywords: Cushing, Foramen magnum, Meningioma, Subtonsilar approach
INTRODUCTION
Since the initial description of a foramen magnum meningiomas (FMMs) in 1872, various surgical approaches have been described. The management of FMM has been a challenge for skull base neurosurgeons. Posterior and posterolateral FMMs are safely removed through a standard midline suboccipital approach.[
The foramen magnum is located in the occipital bone, which has three parts: a squamosal part located behind the foramen magnum; a basal (clival) portion located anterior to the foramen magnum; and a condylar part that connects the squamosal and clival parts.[
The foramen magnum is most commonly approached from posteriorly through the suboccipital and upper cervical region. Tumors arising in the region of the foramen magnum are divided by Cushing and Eisenhardt into a craniospinal group that arises above and grows downward toward the foramen magnum, and a spinocranial group that arises below and grows upward toward the foramen magnum.[
CASE DESCRIPTION
A 47-year-old female patient was referred to a neurosurgery consultation due to headaches that failed to improve with standard medical treatment. Her headaches had been progressively worse for the past 3 years. She also complained of tremors involving the upper limbs and being constantly unable to maintain balance, in which she described as an “unsteadiness.” She denied any issues with swallowing and reported to other deficits.
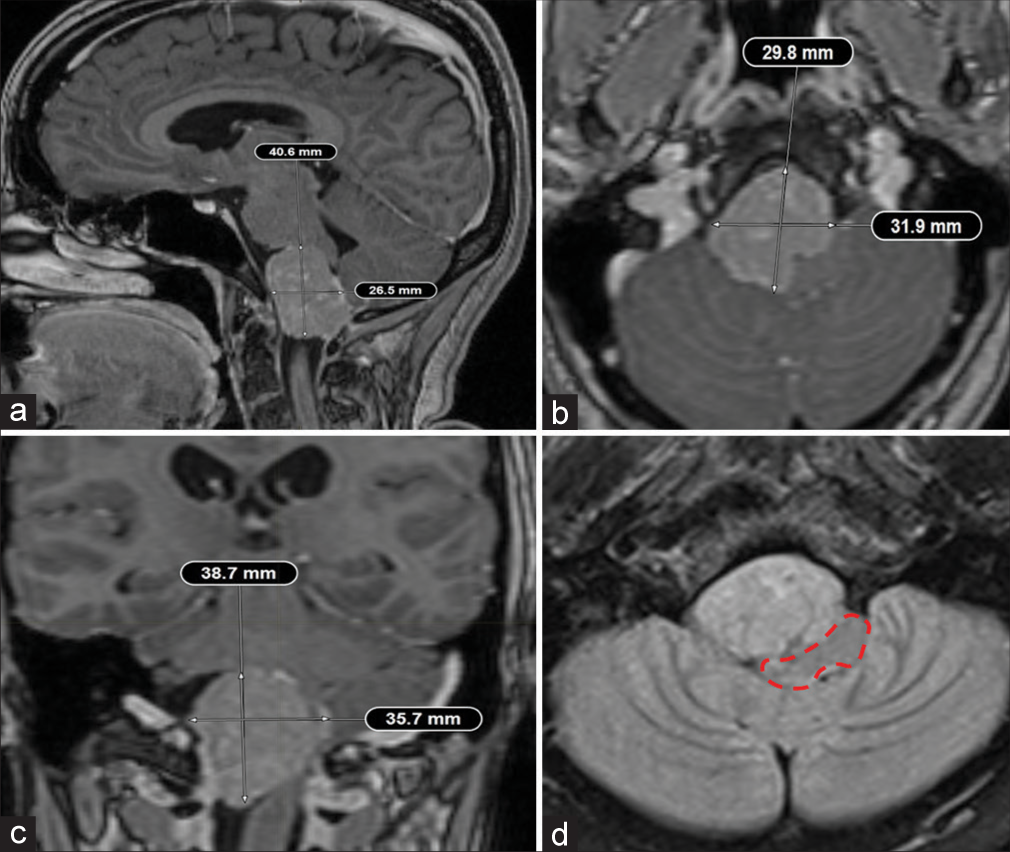
Magnetic resonance imaging (MRI) showed a mass-occupying lesion originating from the anterior aspect of the foramen magnum that caused significant displacement of the brainstem and extends from the pontomedullary sulcus to the cervical spinal cord [
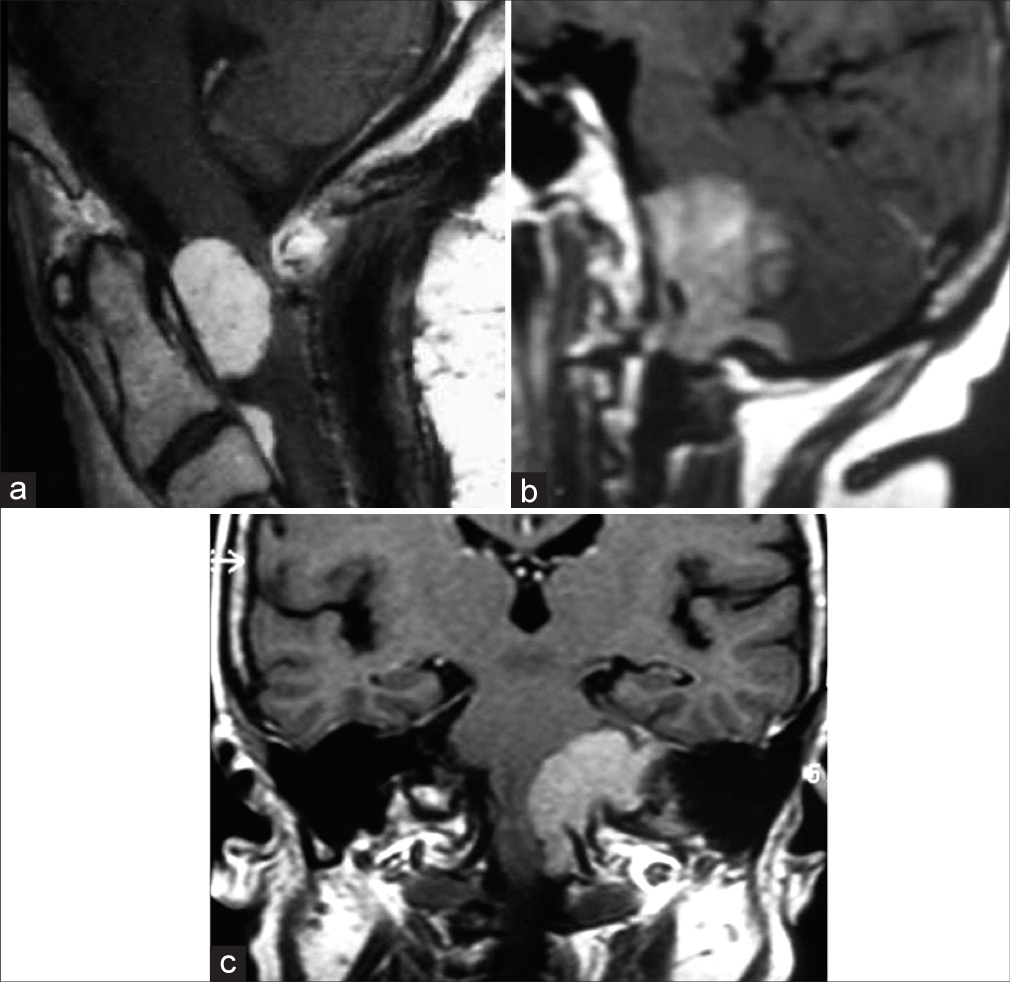
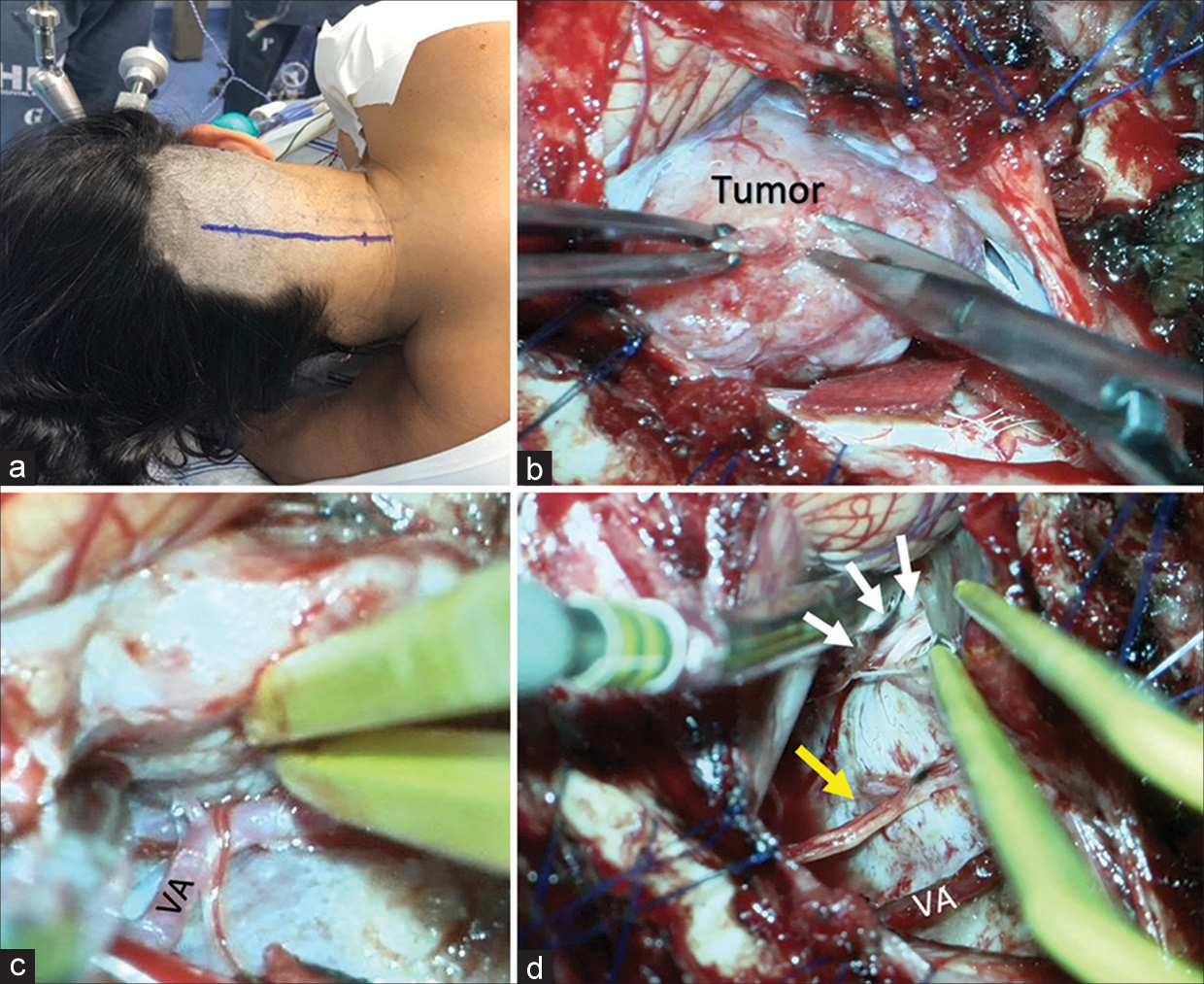
Figure 1:
Example of the last cases seen by the authors. Sagittal view of head magnetic resonance imaging showing a meningioma arising below the foramen magnum, the Spinocranial type (a). A craniospinal type 2 foramen magnum meningioma, reaching above the pontomedullary sulcus on sagittal and coronal views (b and c).
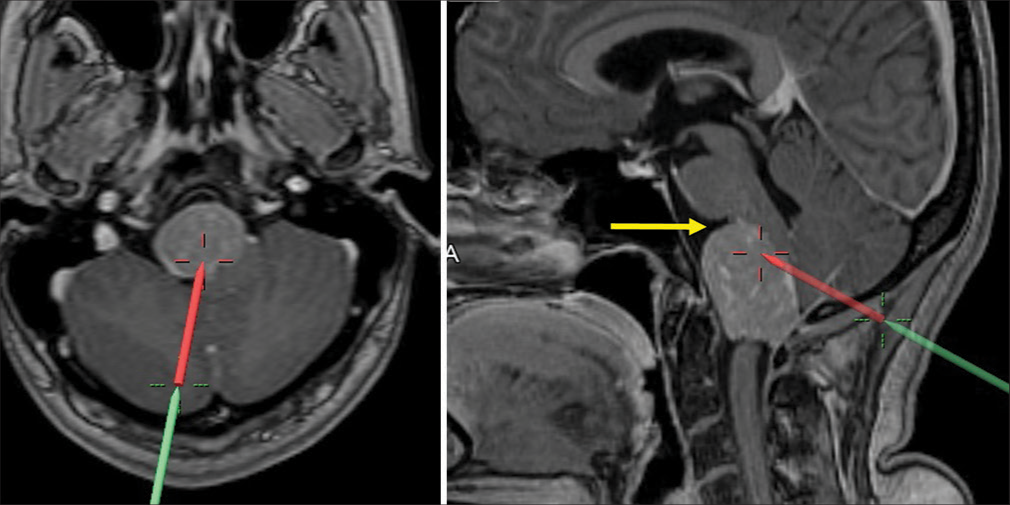
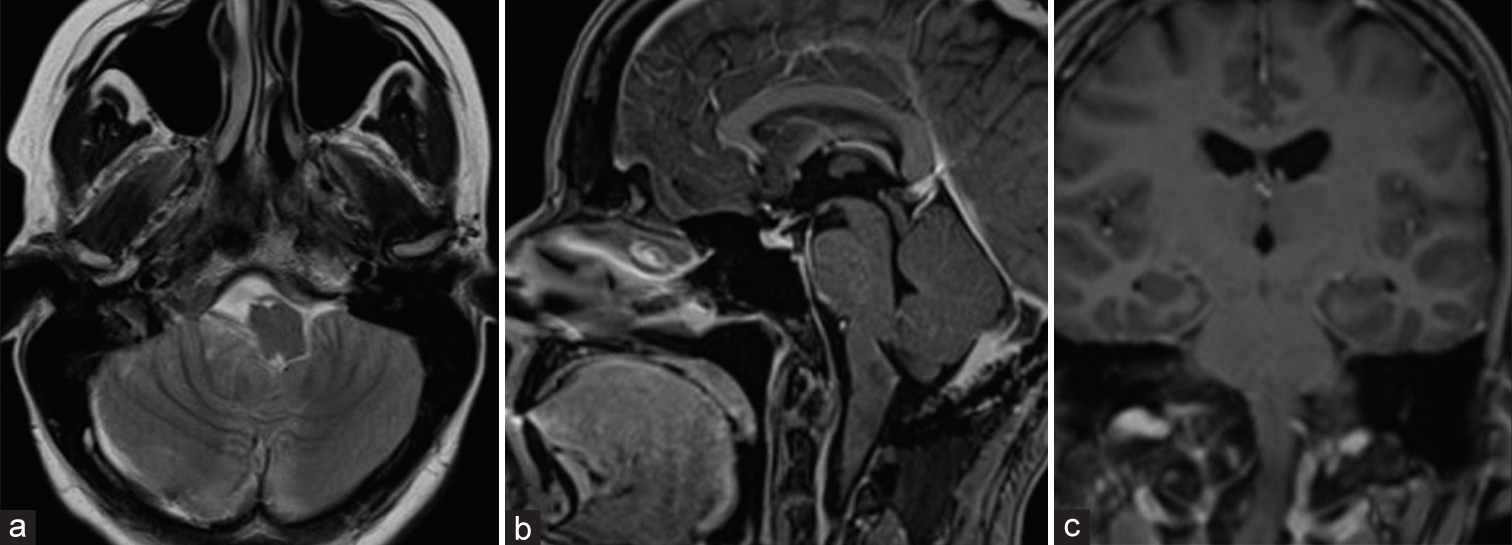
Figure 3:
Neuronavigation in magnetic resonance imaging showing the direction to the mass allowed for the suboccipital midline approach. Note that the tumor was at the level of the pontomedullary sulcus (yellow arrow), and almost completely anterior to the tonsil. Red and green line represents the operative trajectory, shown with neuronavigation.
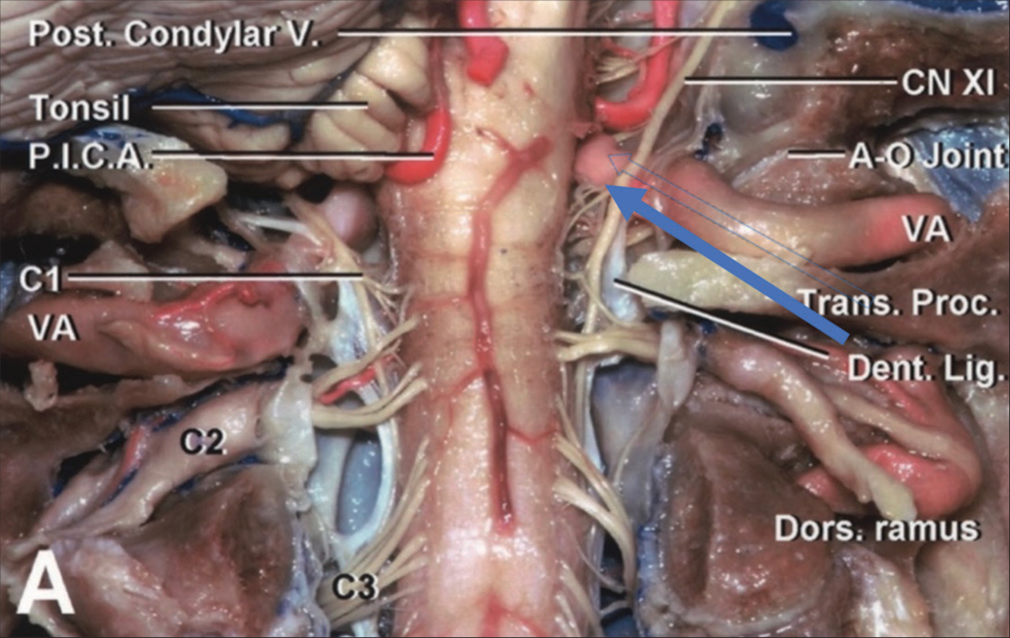
Figure 4:
Courtesy of the Rhoton Collection, American Association of Neurological Surgeons/Neurosurgical Research, and Education Foundation. The complex craniocervical junction anatomy from a posterior view from foramen magnum opening. The blue arrow indicates the surgery approach view in our case. P.I.C.A = posterior inferior cerebellar artery, VA = vertebral artery, CN XI = cranial nerve XI (accesory nerve), AO joint = atlanto-occipital joint, Dent. lig. = dentate ligament, Dors. ramus = Dorsal ramus, Trans. proc. = transverse process, Post. condylar V. = posterior condylar vein.
Figure 5:
Steps from the suboccipital midline approach. Programmed skin incision (a); Intraoperative view, tumor exposition and beginning of debulking (b); dissection and exposure of right vertebral artery (VA), arterial branches for the mass (c); complete resection and view of IX, X, XI complex (white arrows) and XII cranial nerve (yellow arrow) and VA intact (d).
Video 1
Postoperative CT scan and MRI showed no hemorrhages, significant improvement of mass effect, and complete removal of the tumor. The patient was discharged after 10 days. She returned to the outpatient clinic after 16 and 30 days having recovered fully from all previous symptoms. The histopathological results confirmed a grade 1 (the World Health Organization classification) meningioma.
CONCLUSION
We, hereby, endorse that the midline suboccipital subtonsillar approach allowed safe and effective treatment of this anterior FMM.[
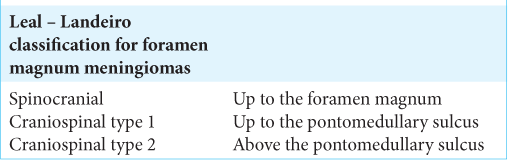
Cushing divided these FMMs into a variety arising above the foramen magnum – craniospinal – and those arising below the foramen magnum – spinocranial.[ The craniospinal type 1 meningiomas may be reached by a posterolateral subtonsillar approach without removing the condyle mainly if they dislocate the brain stem to the opposite side, as we have done in this present case
The craniospinal type 2 meningiomas are those reaching above the pontomedullary sulcus. Herein, the cerebellar hemisphere is wider laterally, above the upper part the tonsils are located, needing more cerebellar retraction, so it is better to use a far-lateral and/or transcondylar approaches to a safer exposure. Indications for each approach can be found on
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cushing H, editors. Meningiomas: Their Classification, Regional Behavior, Life History, and Surgical end Result. Springfield: Charles C Thomas; 1938. 111: 735
2. Dobrowolski S, Ebner F, Lepski G, Tatagiba M. Foramen magnum meningioma: The midline suboccipital subtonsillar approach. Clin Neurol Neurosurg. 2016. 145: 28-34
3. Dobrowolski S, Lepski G, Tatagiba M. Meningioma arising in the hypoglossal canal: The midline suboccipital subtonsillar approach. J Surg Case Rep. 2016. 2016: rjw039
4. Herlan S, Ebner FH, Nitz A, Hirt B, Tatagiba M, Roser F. The midline suboccipital subtonsillar approach to the cerebellomedullary cistern and its structures: Anatomical considerations, surgical technique and clinical application. Clin Neurol Neurosurg. 2014. 125: 98-105
5. Rabadán AT, Campero A, Hernández D. Surgical application of the suboccipital subtonsillar approach to reach the inferior half of medulla oblongata tumors in adult patients. Front Surg. 2015. 2: 72
6. Rhoton AL. The foramen magnum. Neurosurgery. 2000. 47: S155-93
7. Tatagiba M, Koerbel A, Roser F. The midline suboccipital subtonsillar approach to the hypoglossal canal: Surgical anatomy and clinical application. Acta Neurochir (Wien). 2006. 148: 965-9