- Department of Neurosurgery, ARNAS Garibaldi, Via Palermo, Catania
- Department of Neurosurgery, Cannizzaro Hospital, Via Messina, Catania,
- Department of Biomedical and Dental Sciences and Morpho-Functional Imaging, Division of Neurosurgery, University of Messina, Via Consolare Valeria, Messina Sicily, Italy.
Correspondence Address:
Gianluca Scalia
Department of Biomedical and Dental Sciences and Morpho-Functional Imaging, Division of Neurosurgery, University of Messina, Via Consolare Valeria, Messina Sicily, Italy.
DOI:10.25259/SNI_108_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Giancarlo Ponzo, Massimo Furnari, Giuseppe Emmanuele Umana, Massimiliano Giuffrida, Giovanni Federico Nicoletti, Gianluca Scalia. Intradural lumbar disc herniations at the L1–L2 level: A case study and literature review. 11-Apr-2020;11:67
How to cite this URL: Giancarlo Ponzo, Massimo Furnari, Giuseppe Emmanuele Umana, Massimiliano Giuffrida, Giovanni Federico Nicoletti, Gianluca Scalia. Intradural lumbar disc herniations at the L1–L2 level: A case study and literature review. 11-Apr-2020;11:67. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=9954
Abstract
Background: Intradural disc herniations (IDHs) are rare occurrences (0.26–0.30%), and most frequently involve the lumbar spine at the L4–L5 level. Here, we present a patient with an L1–L2 IDH and reviewed the current literature.
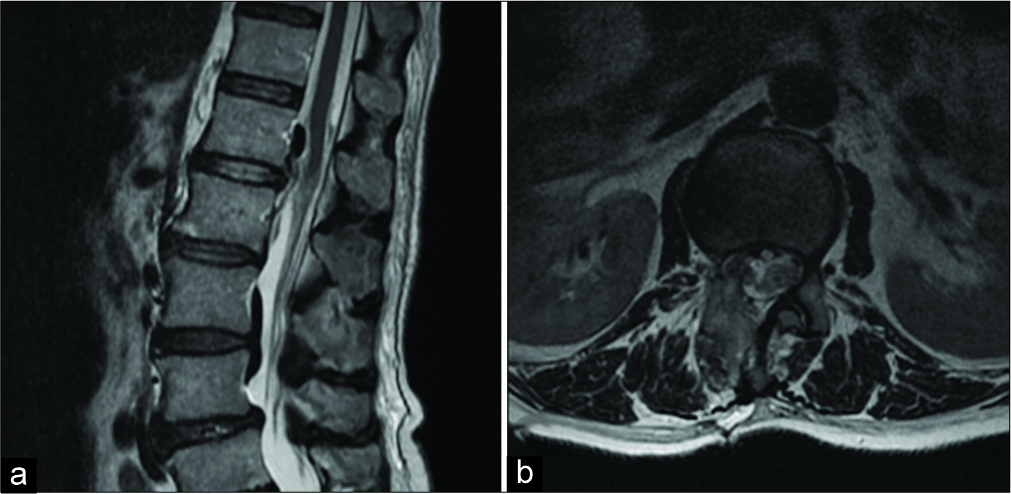
Case Description: A 65-year-old female presented with the acute onset of bilateral paraparesis accompanied by urinary dysfunction. The lumbar MRI showed a mass at the L1–L2 level with caudal migration, accompanied by a positive “hawk-beak” sign. At surgery, consisting of a L1–L2 laminectomy, a large IDH was encountered responsible for marked cauda equina/root compression. Postoperatively, the patient immediately fully recovered. The literature we identified cited just seven similar studies of L1–L2 IDH.
Conclusion: In a 65-year-old female, an IDH was anticipated at the L1–L2 level due to the combined MR findings of a large L1–L2 mass with caudal migration and the positive “hawk-beak” sign.
Keywords: Disc herniation, Hawk beak, Intradural, Lumbar, Posterior longitudinal ligament
INTRODUCTION
Intradural disc herniations (IDHs) comprise only 0.26–0.30% of all disc herniations, typically involve the lower lumbar spine (92%), and are mostly located at the L4–L5 level. We identified only seven cases of IDH involving the L1–L2 level.[
MATERIALS AND METHODS
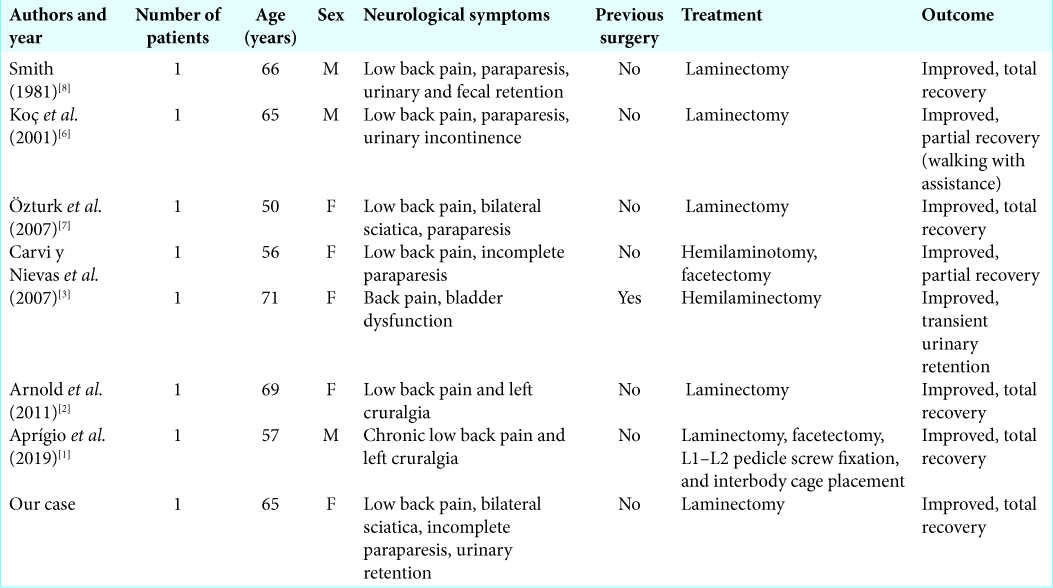
A comprehensive literature search was performed on PubMed, MEDLINE, and Google Scholar databases, using the following MESH terms: “intradural lumbar disc herniation,” “intradural lumbar herniated disc,” “transdural herniated disc,” “transdural disc herniation,” “sequestered lumbar disc,” and “lumbar intradural disc rupture.” Only six (seven patients) out of 63 articles regarding L1–L2 IDH were identified [
CASE REPORT
History
A 65-year-old female had a 2-month history of low back pain and intermittent neurogenic claudication. Over the course of a few days, she developed perineal hypoesthesia accompanied by paraparesis and urinary retention. On examination, she had a positive Laségue’s sign on the right at 30°, right-sided quadriceps weakness, bilateral lower extremity hyporeflexia (loss of patellar and Achilles responses), and loss of pin appreciation in the perineal region.
Preoperative imaging
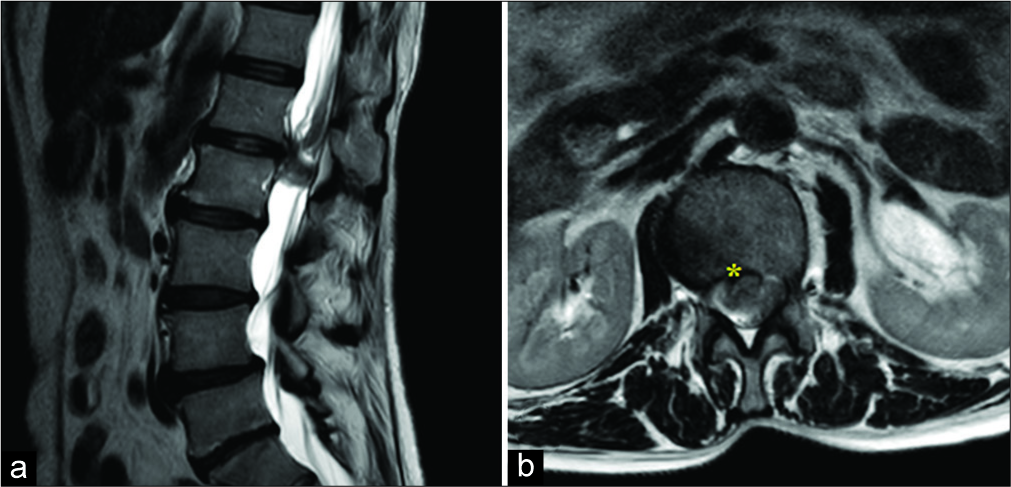
The lumbar MR (T2-weighted sagittal and axial images) showed marked dural compression at the at the L1–L2 level with caudal migration to L2, combined with a positive “hawk- beak” sign. The lesion itself at L1–L2 did not enhance with contrast, but there was enhancement of the surroundings tissues [
Surgical intervention
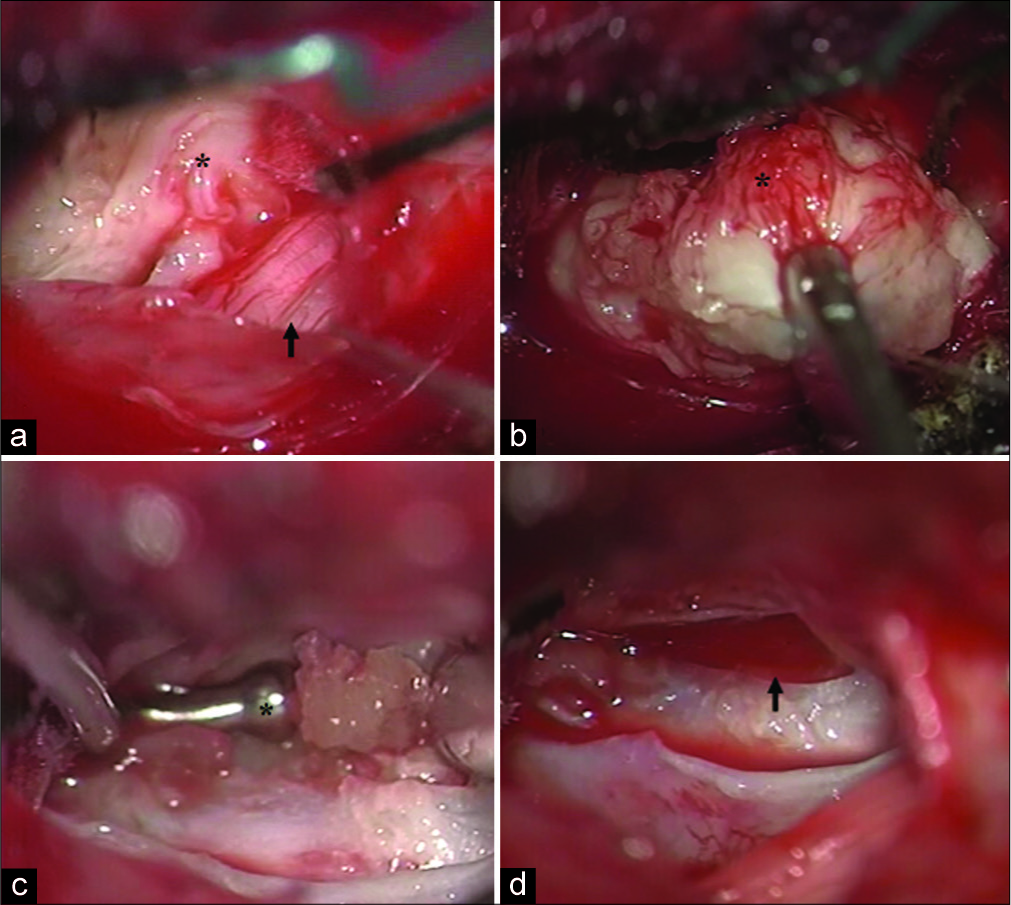
At surgery, consisting of a L1–L2 laminectomy, no significant epidural lesion was present. However, when the dura was opened, a large IDH/fragment was encountered measuring 2 × 1 cm. This was carefully teased away under the operating microscope from the surrounding nerve roots of the cauda equina and ventral dura [
Figure 2:
Intraoperative description of the IDH removal. After the L1-L2 laminectomy, a dural incision is made. The roots of the cauda equina (black arrow) appear dislocated by a voluminous migrated intradural disc fragment. (black asterisk) (a) With the use of disc pounches a removal of the voluminous IDH is performed. (b) Microsurgical discectomy is completed with the use of a Cushing’s buttoned nerve hook (black asterisk) through the ventral dural defect (c), achieving a macroscopic complete disc removal and decompression of the nerve roots (black arrow). (d).
DISCUSSION
IDHs are rare, accounting for 0.27–0.33% of all herniated discs. Of the approximate 151 cases of IDH reported, 3% occur in the cervical region, 5% in thoracic region, and 92% in the lumbar spine.[
Noncontrast and contrast MR findings for IDH
On T1- and T2-weighted MR images, IDHs are homogeneously isointense. Notably, Hidalgo-Ovejero et al.[
Gadolinium-enhanced MR scans demonstrate a positive “Hawk-Beak” sign (e.g., a “Beak-Like” appearance at the level of the lesion sharply compressing the dural sac, especially on T2-weighted axial images). Hida et al.[
CONCLUSION
IDHs are rare, the authors found only seven such cases reported in the literature involving the L1–L2 level.[
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aprígio RM, Caramanti RL, Santos FO, Maia IP, Filipe FM, de Moraes DF. Intradural disc herniation at the L1-L2 level: A case report and literature review. Surg Neurol Int. 2019. 10: 196-
2. Arnold PM, Wakwaya YT. Intradural disk herniation at L1-L2 Report of two cases. J Spinal Cord Med. 2011. 34: 312-4
3. Carvi y Nievas MN, Hoellerhage HG. Unusual sequestered disc fragments simulating spinal tumors and other space-occupying lesions. Clinical article. J Neurosurg Spine. 2009. 11: 42-8
4. Hida K, Iwasaki Y, Abe H, Shimazaki M, Matsuzaki T. Magnetic resonance imaging of intradural lumbar disc herniation. J Clin Neurosci. 1999. 6: 345-7
5. Hidalgo-Ovejero AM, Garcia-Mata S, Gozzi-Vallejo S, Izco-Cabezon T, Martinez-Morentin J, Martinez-Grande M. Intradural disc herniation and epidural gas: Something more than a casual association?. Spine (Phila Pa 1976). 2004. 29: E463-7
6. Koc RK, Akdemir H, Oktem IS, Menku A. Intradural lumbar disc herniation: Report of two cases. Neurosurg Rev. 2001. 24: 44-7
7. Oztürk A, Avci E, Yazgan P, Torun F, Yücetaş S, Karabağ H. Intradural herniation of intervertebral disc at the level of lumbar 1-lumbar 2. Turk Neurosurg. 2007. 17: 134-7
8. Smith RV. Intradural disc rupture. Report of two cases. J Neurosurg. 1981. 55: 117-20