- Department of Neurosurgery, Faculty of Medicine, The University of Tokyo, Japan.
Correspondence Address:
Satoru Miyawaki, Department of Neurosurgery, Faculty of Medicine, The University of Tokyo, Japan.
DOI:10.25259/SNI_1030_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yudai Hirano1, Satoru Miyawaki1, Yusuke Sakaguchi1, Satoshi Koizumi1, Hiroki Hongo1, Nobuhito Saito1. A bibliometric analysis of the 100 most-cited clinical articles in the research of intracranial artery stenosis and intracranial atherosclerosis. 08-Mar-2024;15:74
How to cite this URL: Yudai Hirano1, Satoru Miyawaki1, Yusuke Sakaguchi1, Satoshi Koizumi1, Hiroki Hongo1, Nobuhito Saito1. A bibliometric analysis of the 100 most-cited clinical articles in the research of intracranial artery stenosis and intracranial atherosclerosis. 08-Mar-2024;15:74. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12792
Abstract
Background: Intracranial arterial stenosis (ICAS), caused by intracranial atherosclerosis, is one of the major causes of ischemic stroke. This study identified the top 100 most-cited publications on ICAS through a bibliometric analysis.
Methods: Two independent authors conducted a search in the Web of Science database for clinical articles on ICAS published between 1993 and 2022. The top 100 most-cited articles were then extracted. For each article, the analysis covered the title, author, country of origin/affiliation, journal, total number of citations, number of citations per year, and type of study.
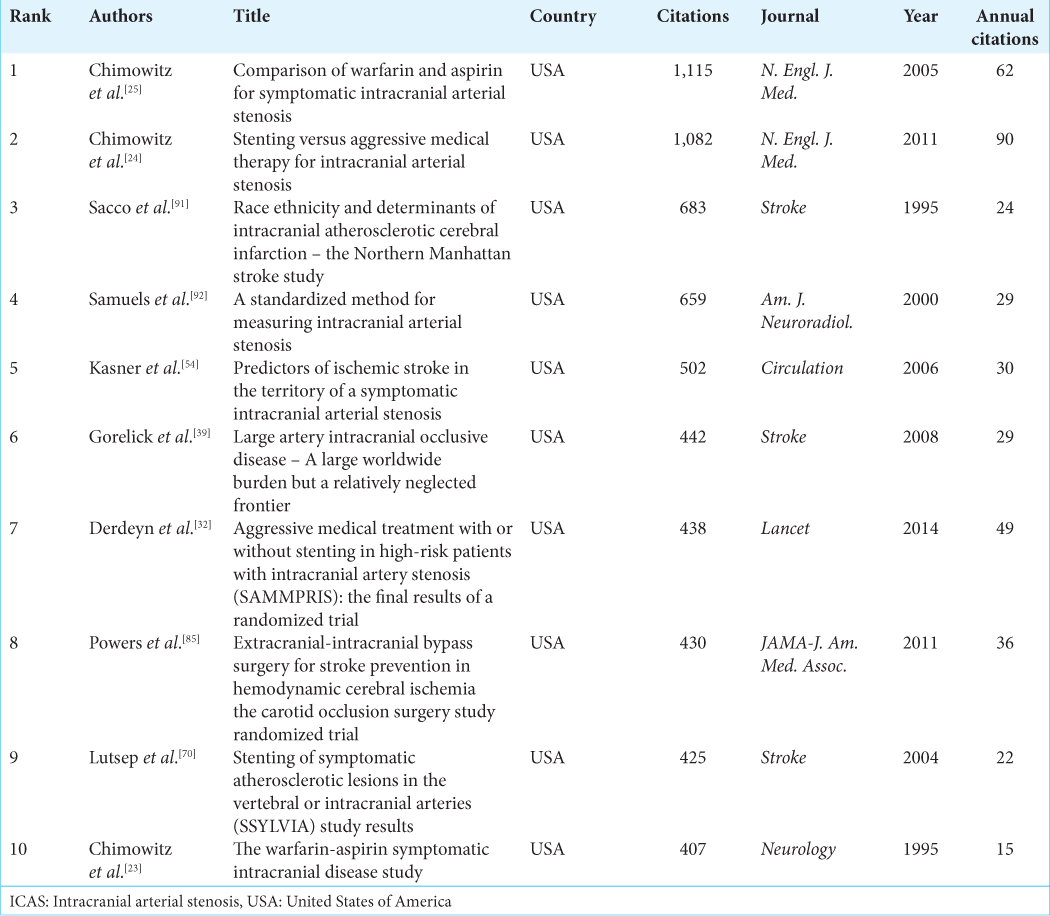
Results: The top 100 most-cited papers in the ICAS were authored by 565 authors from 12 countries and published in 29 journals. In terms of the 5-year trend, the largest number of papers were published between 2003 and 2007 (n = 31). The median number of citations for the 100 papers was 161 (range 109–1,115). The journal with the highest proportion of the 100 most published articles was Stroke, accounting for 41% of articles and 37% of the citations. According to country of origin, the United States of America accounted for the largest number of articles, followed by China, Japan, and South Korea, with these four countries together accounting for 81% of the total number of articles and 88% of the citations. Trends in the past five years included the use of terms such as acute ischemic stroke and mechanical thrombectomy.
Conclusion: The findings of this study provide novel insight into this field and will facilitate future research endeavors.
Keywords: Bibliometric analysis, Intracranial artery stenosis, Intracranial atherosclerosis, Neurosurgery, Vascular
INTRODUCTION
Intracranial artery stenosis (ICAS), of which intracranial atherosclerosis is the predominant background, is the leading cause of ischemic stroke, and its prevalence is high in individuals of Asian, African, and Hispanic ancestry.[
Numerous ICAS studies have been published to date. Bibliometric analysis has been conducted in various fields and has gained immense popularity. Specifically in neurosurgery, it has been increasingly applied to investigate diseases[
To the best of our knowledge, no published bibliometric studies have focused on ICAS and intracranial atherosclerosis. Therefore, in this study, we aim to extract the 100 most-cited articles in the field of ICAS/intracranial atherosclerosis and evaluate their influence using bibliometric methods.
MATERIALS AND METHODS
Bibliometric search strategy
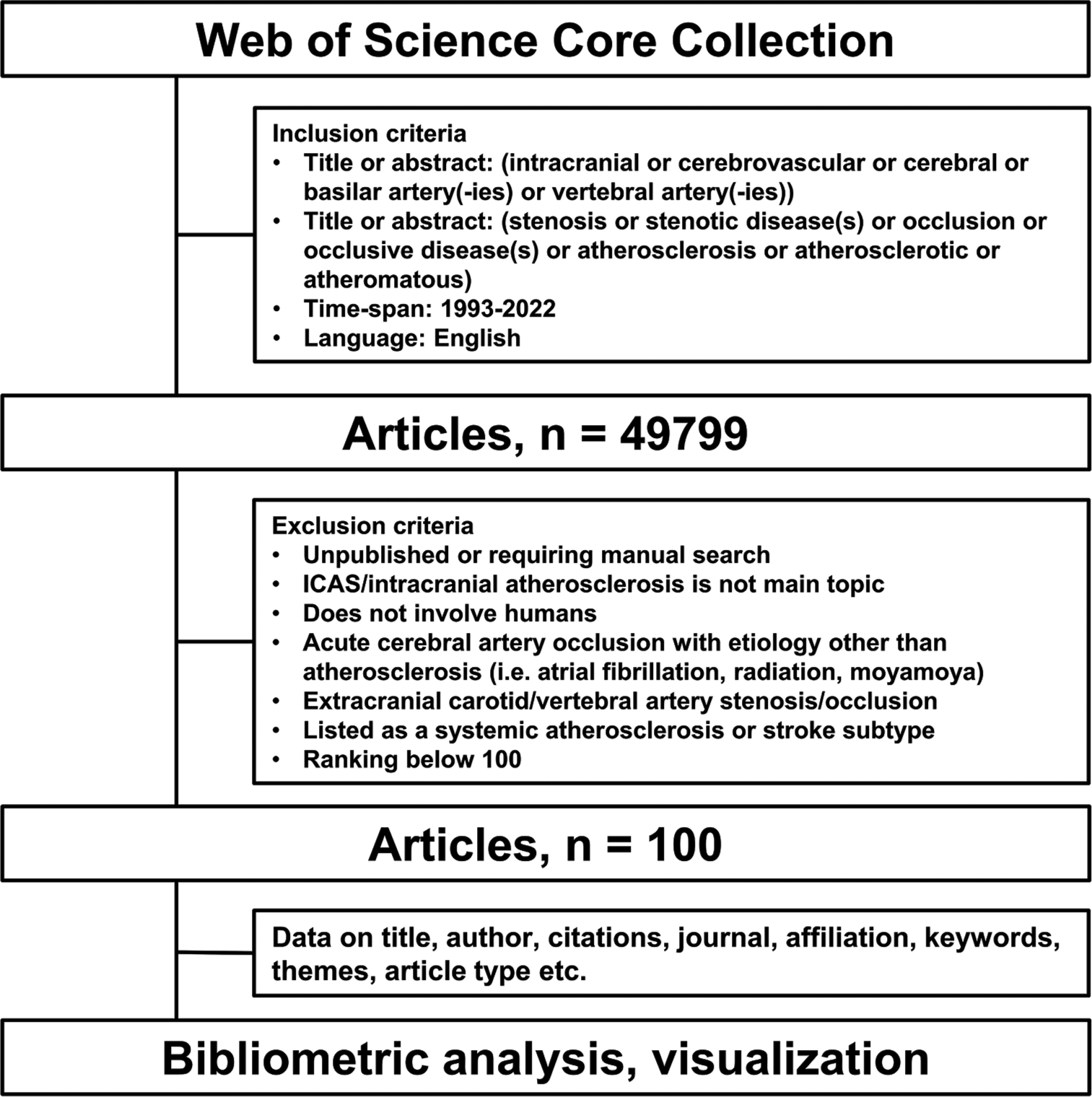
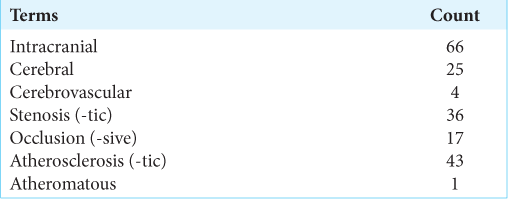
On February 12, 2023, we conducted a search in the Web of Science database to identify the most-cited papers on ICAS. The search terms were used based on the title or abstract, as presented in
Meanwhile, articles that are not published or require manual search, in which ICAS/intracranial atherosclerosis was not the main topic, that do not involve humans, with acute cerebral artery occlusion with etiology other than atherosclerosis (i.e., atrial fibrillation, radiation, and moyamoya) or extracranial carotid/vertebral artery stenosis/occlusion, and listed as a systemic atherosclerosis or stroke subtype were excluded from the study. A flow diagram of the data extraction is shown in
Extraction of data and bibliometric parameters
A list of the top 100 most-cited articles selected from the database was arranged in a data table. General data such as title, author, total citations, annual citations, journal publication, and year of publication were extracted directly from the search results. Countries and institutions were determined according to the corresponding author’s affiliation. Articles were classified as original articles or reviews based on the search results and subsequent checks. Two authors (Y.H. and Y.S.) classified the research themes of each article by screening 100 paper abstracts and keywords, and finally, verification was conducted by a third author (S.M.). Journal impact factors were obtained from the 2021 Incites Journal Citation Reports by Clarivate Analytics.
Statistical analysis
For comparisons between the two groups, the Student’s t-test was used for continuous variables. Statistical analyses were performed using the JMP Pro 16 software (SAS Institute Inc., Cary, NC, United States of America [USA]). In addition, VOSviewer software, version 1.6.19 (Leiden University, Leiden, the Netherlands), for Windows, was used to plot the data of the visualization network.
RESULTS
A total of 49,799 publications were retrieved from the Web of Science database. The top 100 most-cited articles are listed in
Publication year and citation
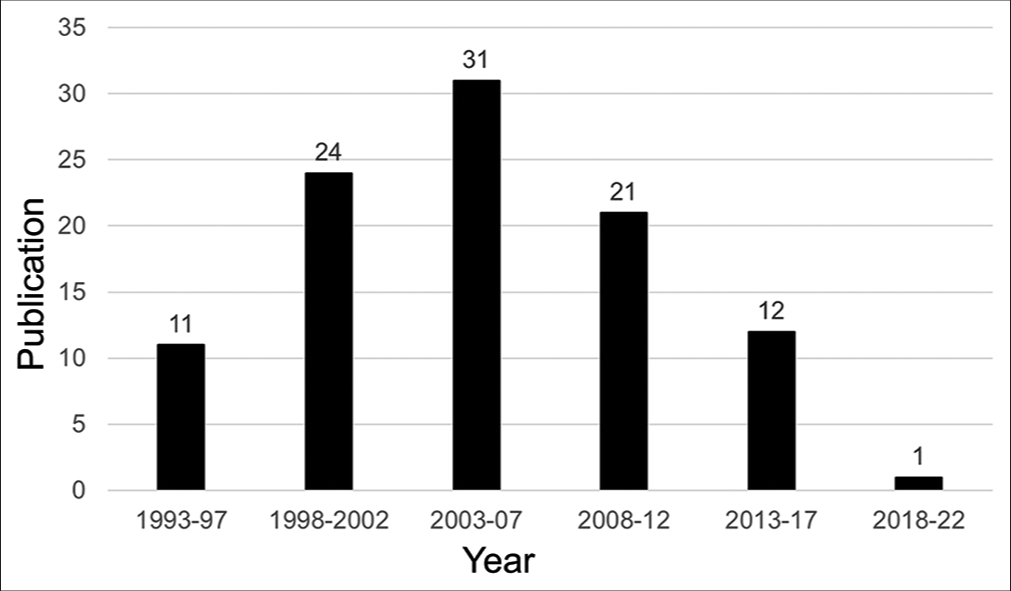
A total of 100 articles were published between 1993 and 2019. For the 5-year trends, the most published interval was 2003–2007 (n = 31), followed by 1997–2002 (n = 24) and 2008–2012 (n = 21) [
Article types, keywords, and themes
Of the top 100 most-cited articles, 91 were original articles, and nine were reviews. There was no significant difference in the total number of citations (213 vs. 225; P = 0.84) or annual number of citations (13.4 vs. 20.3; P = 0.12) between the original and the review articles. Among the 100 most-cited papers, excluding reviews, the most featured themes were endovascular treatment (29%), radiological features and diagnosis (16%), risk factors (15%), and epidemiology (10%). To visualize the connection between keywords, the relationship between the words in the title and abstract was drawn using VOSviewer [
Figure 3:
Network visualization of keywords in the titles and abstracts. The minimum number of keyword occurrences was fixed at 10, and the minimum cluster size was 3. The keywords that met the threshold were plotted in several clusters, with each color representing a different cluster: The red and purple clusters represent intracranial atherosclerosis and its pathophysiology; the yellow cluster represents radiological methods; the green cluster represents antithrombotic therapy for intracranial artery stenosis; and the blue cluster represents intracranial arterial stenosis and percutaneous endovascular treatment.
Recent trends
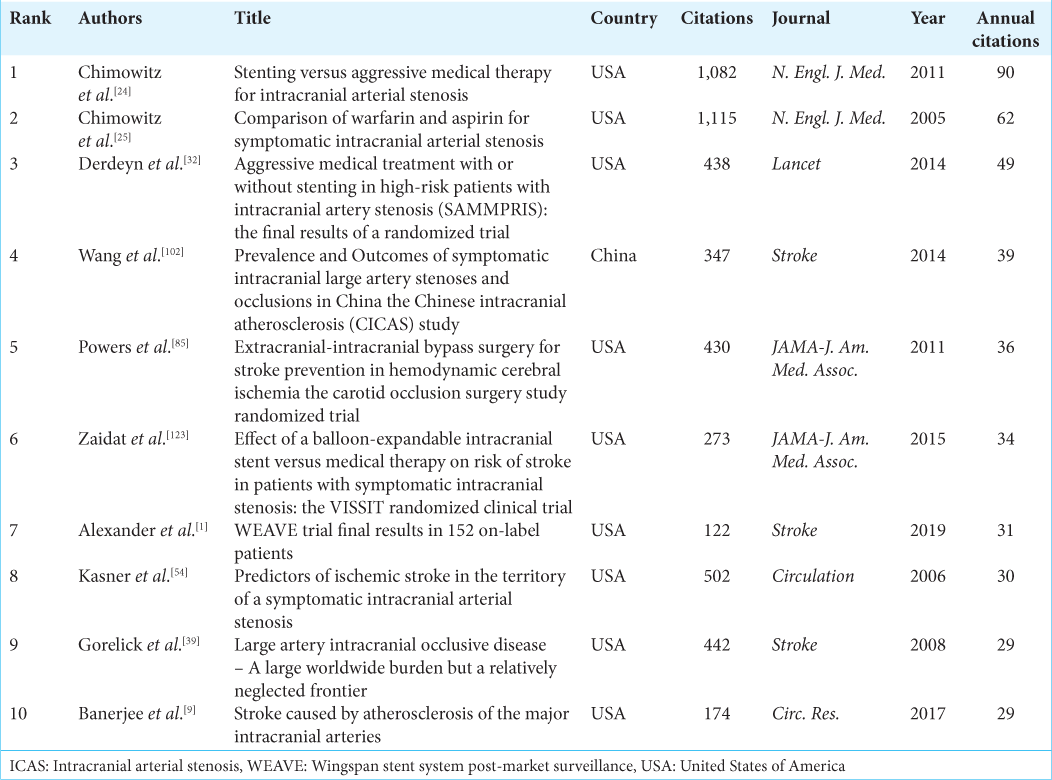
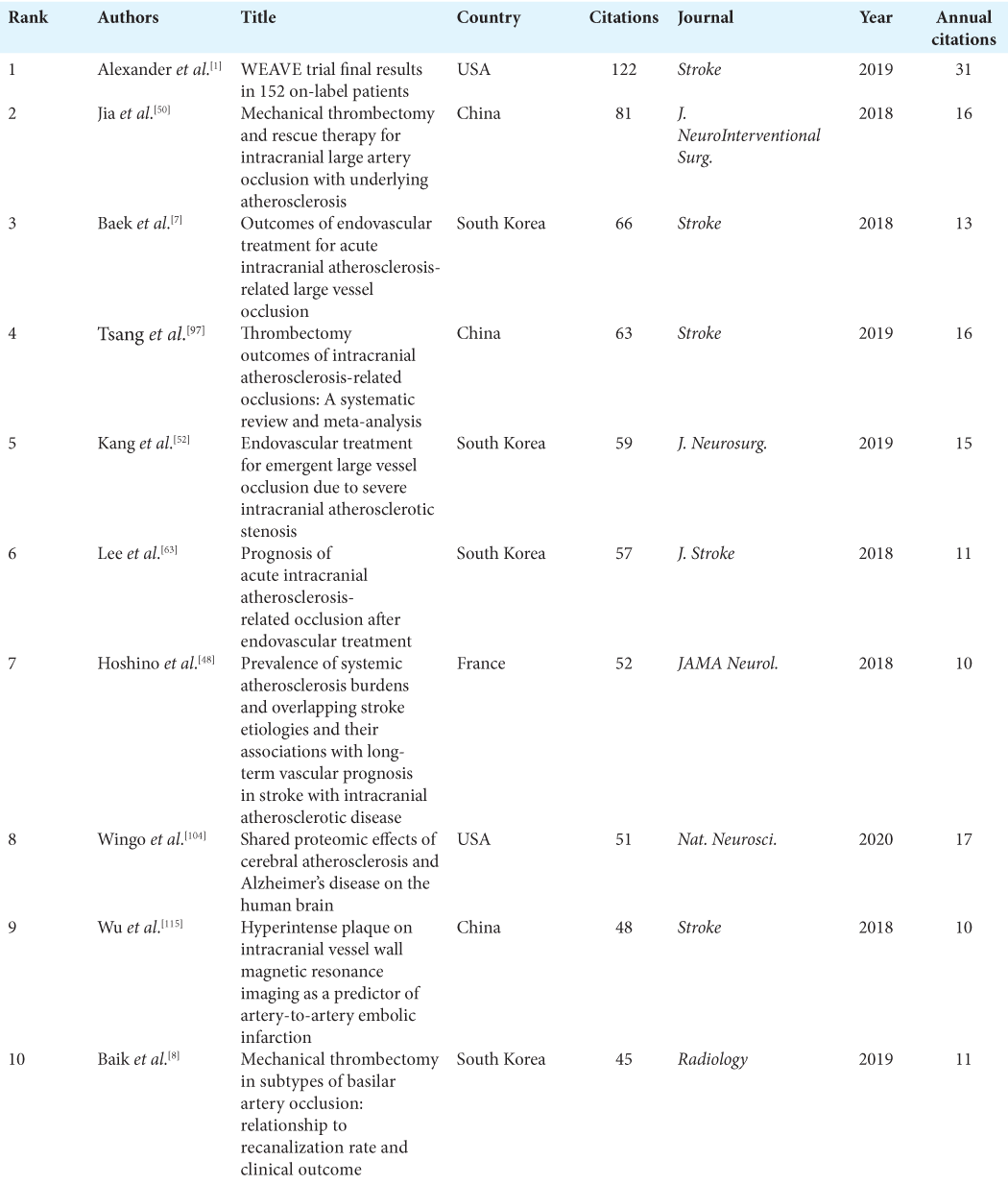
Since all but one of the papers published after 2018 were not included in the top 100 list, trends in the past few years could not be reflected in the analysis. The top 10 most-cited papers published since 2018 are listed in
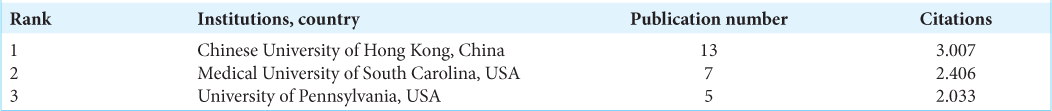
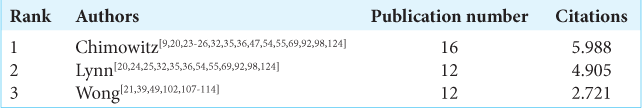
Journals, countries, authors, and institutions
In total, 100 articles were published in 27 journals. Stroke was the most common journal (n = 41), followed by Neurology (n = 13) and the American Journal of Neuroradiology (n = 9). The three journals accounted for 63% of the total publications. The journal’s impact factors are presented in
There were 565 authors involved in the 100 publications; the corresponding authors were from 12 countries [
DISCUSSION
Our study identified the 100 most-cited publications on ICAS/intracranial atherosclerosis and analyzed their overall characteristics, which clarified the overall progress of the research field, along with the journals, institutions, authors, and keyword levels. Bibliometric analysis is used to examine the characteristics of published articles based on specific parameters and has been applied in the field of neurosurgery.[
The top 100 most-cited articles are highly rated articles in a particular field, and a quantitative analysis of these articles reveals the synthesizing characteristics of key research. ICAS, the major cause of which is intracranial atherosclerosis, is the leading cause of ischemic stroke. Several hotspots regarding the epidemiology, pathophysiology, radiology/diagnosis, and medical and surgical treatments for the disease have been identified.
Terminology selection was challenging in this study since the terminology for ICAS and intracranial atherosclerosis was not standardized; multiple search terms were necessary to enable a comprehensive analysis. The search terms were elaborated such that a wide range of articles could be extracted without missing important papers. The results of the analysis of the terminology used in the titles are listed in
Regarding the year of publication, both the number of papers and citations increased after 2003; the number of annual citations also significantly increased after 2003 compared with before 2002. This may be due to the publication of the warfarin-aspirin symptomatic intracranial disease trial, a representative RCT on medical treatment with two antithrombotic agents,[
The top four topics in the papers were endovascular treatment, radiological features and diagnosis, risk factors, and epidemiology, accounting for approximately 70% of the total. These results indicate that the mainstream research lies in endovascular treatment, whose efficacy has not yet been proven for ICAS, as well as diagnostic imaging and pathophysiology, including radiological features. Negative data on intracranial stents have a significant impact, and many articles on intracranial stenting have been subsequently published.
Among them, the Wingspan stent system post market surveillance trial, published in 2019, is the most important study in recent years that demonstrated the potential of intracranial stents.[
One limitation of this research method is that except for one paper published after 2018,[
Analysis of keyword relevance yielded four independent clusters. The research topics differed slightly between intracranial atherosclerosis and ICAS. Since the former represents a pathological condition, it has typically been utilized in epidemiology, risk factors, pathophysiology, and diagnostic radiology studies. In the context of ICAS, secondary prevention is a primary aim, especially in symptomatic cases. Therefore, treatment measures were the focus of these studies, which can be interpreted as being closely associated with studies on the use of antithrombotic drugs and stent therapy.
Regarding journal analysis, most of the 100 articles were published in Stroke, followed by Neurology and the American Journal of Neuroradiology, which accounted for more than 60% of all publications. Two representative RCTs were published in the New England Journal of Medicine, the journal with the highest impact factor on the list. This may be explained by the high quality of articles in these journals and the fact that researchers tend to select journals with high-impact factors citing. Another factor is that neuroradiological diagnosis is very important in research on intracranial atherosclerosis. As for authors, Chimowitz, the authors of two RCTs from the USA,[
This study has some limitations. First, although the Web of Science is a powerful tool for literature search, it does not necessarily cover all publications. Second, some authors might have been overestimated because self-citations were not excluded. Third, the analysis was mainly based on the number of citations; hence, recent papers were less likely to be cited, resulting in an underestimation of recent valuable papers. As a precaution, we have added an analysis of papers published in the most recent five years. Even though publications on the most recent topics that remain under development through research, such as genetic analyses, could not be covered. The prevalence of ICAS is higher in Asian, African, and Hispanic populations;[
CONCLUSION
This study conducted a bibliometric analysis of research on ICAS and intracranial atherosclerosis, listing important publications in this field. This analysis provides an objective view of the current state of knowledge in the clinical and research aspects within this field, providing insights into future research emphases.
Data availability
Data supporting this study’s findings are available on request from the corresponding author.
Ethical approval
Institutional review board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
SUPPLEMENTAL TABLES
References
1. Alexander MJ, Zauner A, Chaloupka JC, Baxter B, Callison RC, Gupta R. WEAVE trial: Final results in 152 on-label patients. Stroke. 2019. 50: 889-94
2. Alfaifi A, AlMutairi O, Allhaidan M, Alsaleh S, Ajlan A. The top 50 most-cited articles on acoustic neuroma. World Neurosurg. 2018. 111: e454-64
3. Almutairi O, Albakr A, Al-Habib A, Ajlan A. The top-100 most-cited articles on meningioma. World Neurosurg. 2017. 107: 1025-32.e5
4. Arenillas JF. Intracranial atherosclerosis: Current concepts. Stroke. 2011. 42: S20-3
5. Arenillas JF, Alvarez-Sabín J, Molina CA, Chacón P, Montaner J, Rovira A. C-reactive protein predicts further ischemic events in first-ever transient ischemic attack or stroke patients with intracranial large-artery occlusive disease. Stroke. 2003. 34: 2463-8
6. Arenillas JF, Molina CA, Montaner J, Abilleira S, GonzálezSánchez MA, Alvarez-Sabín J. Progression and clinical recurrence of symptomatic middle cerebral artery stenosis: A long-term follow-up transcranial Doppler ultrasound study. Stroke. 2001. 32: 2898-904
7. Baek JH, Kim BM, Heo JH, Kim DJ, Nam HS, Kim YD. Outcomes of endovascular treatment for acute intracranial atherosclerosis-related large vessel occlusion. Stroke. 2018. 49: 2699-705
8. Baik SH, Park HJ, Kim JH, Jang CK, Kim BM, Kim DJ. Mechanical thrombectomy in subtypes of basilar artery occlusion: Relationship to recanalization rate and clinical outcome. Radiology. 2019. 291: 730-7
9. Banerjee C, Chimowitz MI. Stroke caused by atherosclerosis of the major intracranial arteries. Circ Res. 2017. 120: 502-13
10. Bang OY. Intracranial atherosclerosis: Current understanding and perspectives. J Stroke. 2014. 16: 27-35
11. Bang OY, Kim JW, Lee JH, Lee MA, Lee PH, Joo IS. Association of the metabolic syndrome with intracranial atherosclerotic stroke. Neurology. 2005. 65: 296-8
12. Bash S, Villablanca JP, Jahan R, Duckwiler G, Tillis M, Kidwell C. Intracranial vascular stenosis and occlusive disease: Evaluation with CT angiography, MR angiography, and digital subtraction angiography. AJNR Am J Neuroradiol. 2005. 26: 1012-21
13. Baumgartner RW, Mattle HP, Schroth G. Assessment of >/=50% and <50% intracranial stenoses by transcranial color-coded duplex sonography. Stroke. 1999. 30: 87-92
14. Beach TG, Wilson JR, Sue LI, Newell A, Poston M, Cisneros R. Circle of Willis atherosclerosis: Association with Alzheimer’s disease, neuritic plaques and neurofibrillary tangles. Acta Neuropathol. 2007. 113: 13-21
15. Bos D, Portegies ML, van der Lugt A, Bos MJ, Koudstaal PJ, Hofman A. Intracranial carotid artery atherosclerosis and the risk of stroke in whites: The Rotterdam Study. JAMA Neurol. 2014. 71: 405-11
16. Bos D, van der Rijk MJ, Geeraedts TE, Hofman A, Krestin GP, Witteman JC. Intracranial carotid artery atherosclerosis: Prevalence and risk factors in the general population. Stroke. 2012. 43: 1878-84
17. Bose A, Hartmann M, Henkes H, Liu HM, Teng MM, Szikora I. A novel, self-expanding, nitinol stent in medically refractory intracranial atherosclerotic stenoses: The Wingspan study. Stroke. 2007. 38: 1531-7
18. Brekenfeld C, Schroth G, Mattle HP, Do DD, Remonda L, Mordasini P. Stent placement in acute cerebral artery occlusion: Use of a self-expandable intracranial stent for acute stroke treatment. Stroke. 2009. 40: 847-52
19. Caplan LR, Gorelick PB, Hier DB. Race, sex and occlusive cerebrovascular disease: A review. Stroke. 1986. 17: 648-55
20. Chaturvedi S, Turan TN, Lynn MJ, Kasner SE, Romano J, Cotsonis G. Risk factor status and vascular events in patients with symptomatic intracranial stenosis. Neurology. 2007. 69: 2063-8
21. Chen XY, Wong KS, Lam WW, Zhao HL, Ng HK. Middle cerebral artery atherosclerosis: Histological comparison between plaques associated with and not associated with infarct in a postmortem study. Cerebrovasc Dis. 2008. 25: 74-80
22. Cheng W, Kang Q, Xiao Q. Bibliometric analysis of the top 100 influential studies on carotid artery stenting. World Neurosurg. 2019. 122: e1321-31
23. Chimowitz MI, Kokkinos J, Strong J, Brown MB, Levine SR, Silliman S. The Warfarin-aspirin symptomatic intracranial disease study. Neurology. 1995. 45: 1488-93
24. Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011. 365: 993-1003
25. Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR. Warfarin-aspirin symptomatic intracranial disease trial investigators. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005. 352: 1305-16
26. Chimowitz MI, Strong J, Brown MB, Perkins A, Liang WM, Yang I. Prognosis of patients with symptomatic vertebral or basilar artery stenosis. Stroke. 1998. 29: 1389-92
27. Clark WM, Barnwell SL, Nesbit G, O’Neill OR, Wynn ML, Coull BM. Safety and efficacy of percutaneous transluminal angioplasty for intracranial atherosclerotic stenosis. Stroke. 1995. 26: 1200-4
28. Cloud GC, Markus HS. Diagnosis and management of vertebral artery stenosis. QJM. 2003. 96: 27-54
29. Connors JJ, Wojak JC. Percutaneous transluminal angioplasty for intracranial atherosclerotic lesions: Evolution of technique and short-term results. J Neurosurg. 1999. 91: 415-23
30. Coward LJ, McCabe DJ, Ederle J, Featherstone RL, Clifton A, Brown MM. Long-term outcome after angioplasty and stenting for symptomatic vertebral artery stenosis compared with medical treatment in the Carotid And Vertebral Artery Transluminal Angioplasty Study (CAVATAS): A randomized trial. Stroke. 2007. 38: 1526-30
31. D’Armiento FP, Bianchi A, de Nigris F, Capuzzi DM, D’Armiento MR, Crimi G. Age-related effects on atherogenesis and scavenger enzymes of intracranial and extracranial arteries in men without classic risk factors for atherosclerosis. Stroke. 2001. 32: 2472-9
32. Derdeyn CP, Chimowitz MI, Lynn MJ, Fiorella D, Turan TN, Janis LS. Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): The final results of a randomised trial. Lancet. 2014. 383: 333-41
33. Dofuku S, Sonehara K, Miyawaki S, Sakaue S, Imai H, Shimizu M. Genome-wide association study of intracranial artery stenosis followed by phenome-wide association study. Transl Stroke Res. 2023. 14: 322-33
34. Feldmann E, Daneault N, Kwan E, Ho KJ, Pessin MS, Langenberg P. Chinese-white differences in the distribution of occlusive cerebrovascular disease. Neurology. 1990. 40: 1541-5
35. Feldmann E, Wilterdink JL, Kosinski A, Lynn M, Chimowitz MI, Sarafin J. The stroke outcomes and neuroimaging of intracranial atherosclerosis (SONIA) trial. Neurology. 2007. 68: 2099-106
36. Fiorella D, Derdeyn CP, Lynn MJ, Barnwell SL, Hoh BL, Levy EI. Detailed analysis of periprocedural strokes in patients undergoing intracranial stenting in Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS). Stroke. 2012. 43: 2682-8
37. Fiorella D, Levy EI, Turk AS, Albuquerque FC, Niemann DB, Aagaard-Kienitz B. US multicenter experience with the wingspan stent system for the treatment of intracranial atheromatous disease: Periprocedural results. Stroke. 2007. 38: 881-7
38. Gomez CR, Misra VK, Liu MW, Wadlington VR, Terry JB, Tulyapronchote R. Elective stenting of symptomatic basilar artery stenosis. Stroke. 2000. 31: 95-9
39. Gorelick PB, Wong KS, Bae HJ, Pandey DK. Large artery intracranial occlusive disease: A large worldwide burden but a relatively neglected frontier. Stroke. 2008. 39: 2396-9
40. Goyal M, Menon BK, van Zwam WH, J Dippel DW, Mitchell PJ, Demchuk AM. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet. 2016. 387: 1723-31
41. Gröschel K, Schnaudigel S, Pilgram SM, Wasser K, Kastrup A. A systematic review on outcome after stenting for intracranial atherosclerosis. Stroke. 2009. 40: e340-7
42. Gupta R, Al-Ali F, Thomas AJ, Horowitz MB, Barrow T, Vora NA. Safety, feasibility, and short-term follow-up of drug-eluting stent placement in the intracranial and extracranial circulation. Stroke. 2006. 37: 2562-6
43. Henkes H, Miloslavski E, Lowens S, Reinartz J, Liebig T, Kühne D. Treatment of intracranial atherosclerotic stenoses with balloon dilatation and self-expanding stent deployment (WingSpan). Neuroradiology. 2005. 47: 222-8
44. Higashida RT, Tsai FY, Halbach VV, Dowd CF, Smith T, Fraser K. Transluminal angioplasty for atherosclerotic disease of the vertebral and basilar arteries. J Neurosurg. 1993. 78: 192-8
45. Hirai T, Korogi Y, Ono K, Nagano M, Maruoka K, Uemura S. Prospective evaluation of suspected stenoocclusive disease of the intracranial artery: Combined MR angiography and CT angiography compared with digital subtraction angiography. AJNR Am J Neuroradiol. 2002. 23: 93-101
46. Hirano T, Minematsu K, Hasegawa Y, Tanaka Y, Hayashida K, Yamaguchi T. Acetazolamide reactivity on 123I-IMP single photon emission computed tomography in patients with major cerebral artery occlusive disease: Correlation with positron emission tomography parameters. J Cereb Blood Flow Metab. 1994. 14: 763-70
47. Holmstedt CA, Turan TN, Chimowitz MI. Atherosclerotic intracranial arterial stenosis: Risk factors, diagnosis, and treatment. Lancet Neurol. 2013. 12: 1106-14
48. Hoshino T, Sissani L, Labreuche J, Ducrocq G, Lavallée PC, Meseguer E. Prevalence of systemic atherosclerosis burdens and overlapping stroke etiologies and their associations with long-term vascular prognosis in stroke with intracranial atherosclerotic disease. JAMA Neurol. 2018. 75: 203-11
49. Huang YN, Gao S, Li SW, Huang Y, Li JF, Wong KS. Vascular lesions in Chinese patients with transient ischemic attacks. Neurology. 1997. 48: 524-5
50. Jia B, Feng L, Liebeskind DS, Huo X, Gao F, Ma N. Mechanical thrombectomy and rescue therapy for intracranial large artery occlusion with underlying atherosclerosis. J Neurointerv Surg. 2018. 10: 746-50
51. Jiang WJ, Wang YJ, Du B, Wang SX, Wang GH, Jin M. Stenting of symptomatic M1 stenosis of middle cerebral artery: An initial experience of 40 patients. Stroke. 2004. 35: 1375-80
52. Kang DH, Yoon W, Kim SK, Baek BH, Lee YY, Kim YW. Endovascular treatment for emergent large vessel occlusion due to severe intracranial atherosclerotic stenosis. J Neurosurg. 2018. 130: 1-8
53. Kappelle LJ, Eliasziw M, Fox AJ, Sharpe BL, Barnett HJ. Importance of intracranial atherosclerotic disease in patients with symptomatic stenosis of the internal carotid artery. The North American Symptomatic Carotid Endarterectomy Trail. Stroke. 1999. 30: 282-6
54. Kasner SE, Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS. Warfarin aspirin symptomatic intracranial disease trial investigators. Predictors of ischemic stroke in the territory of a symptomatic intracranial arterial stenosis. Circulation. 2006. 113: 555-63
55. Kasner SE, Lynn MJ, Chimowitz MI, Frankel MR, Howlett-Smith H, Hertzberg VS. Warfarin vs aspirin for symptomatic intracranial stenosis: Subgroup analyses from WASID. Neurology. 2006. 67: 1275-8
56. Kern R, Steinke W, Daffertshofer M, Prager R, Hennerici M. Stroke recurrences in patients with symptomatic vs asymptomatic middle cerebral artery disease. Neurology. 2005. 65: 859-64
57. Kim JS, Nah HW, Park SM, Kim SK, Cho KH, Lee J. Risk factors and stroke mechanisms in atherosclerotic stroke: Intracranial compared with extracranial and anterior compared with posterior circulation disease. Stroke. 2012. 43: 3313-8
58. Konishi M, Iso H, Komachi Y, Iida M, Shimamoto T, Jacobs DR. Associations of serum total cholesterol, different types of stroke, and stenosis distribution of cerebral arteries. The Akita Pathology Study. Stroke. 1993. 24: 954-64
59. Kuroda S, Houkin K, Kamiyama H, Mitsumori K, Iwasaki Y, Abe H. Long-term prognosis of medically treated patients with internal carotid or middle cerebral artery occlusion: Can acetazolamide test predict it?. Stroke. 2001. 32: 2110-6
60. Kwon SU, Cho YJ, Koo JS, Bae HJ, Lee YS, Hong KS. Cilostazol prevents the progression of the symptomatic intracranial arterial stenosis: The multicenter double-blind placebo-controlled trial of cilostazol in symptomatic intracranial arterial stenosis. Stroke. 2005. 36: 782-6
61. Lammie GA, Sandercock PA, Dennis MS. Recently occluded intracranial and extracranial carotid arteries. Relevance of the unstable atherosclerotic plaque. Stroke. 1999. 30: 1319-25
62. Lee DK, Kim JS, Kwon SU, Yoo SH, Kang DW. Lesion patterns and stroke mechanism in atherosclerotic middle cerebral artery disease: Early diffusion-weighted imaging study. Stroke. 2005. 36: 2583-8
63. Lee JS, Lee SJ, Yoo JS, Hong JH, Kim CH, Kim YW. Prognosis of acute intracranial atherosclerosis-related occlusion after endovascular treatment. J Stroke. 2018. 20: 394-403
64. Leung SY, Ng TH, Yuen ST, Lauder IJ, Ho FC. Pattern of cerebral atherosclerosis in Hong Kong Chinese. Severity in intracranial and extracranial vessels. Stroke. 1993. 24: 779-86
65. Levy EI, Horowitz MB, Koebbe CJ, Jungreis CC, Pride GL, Dutton K. Transluminal stent-assisted angiplasty of the intracranial vertebrobasilar system for medically refractory, posterior circulation ischemia: early results. Neurosurgery. 2001. 48: 1215-21 discussion 1221-3
66. Levy EI, Mehta R, Gupta R, Hanel RA, Chamczuk AJ, Fiorella D. Self-expanding stents for recanalization of acute cerebrovascular occlusions. AJNR Am J Neuroradiol. 2007. 28: 816-22
67. Levy EI, Turk AS, Albuquerque FC, Niemann DB, AagaardKienitz B, Pride L. Wingspan in-stent restenosis and thrombosis: incidence, clinical presentation, and management. Neurosurgery. 2007. 61: 644-50 discussion 650-1
68. Li X, Wang A, Wang J, Wu J, Wang D, Gao X. Association between High-density-lipoprotein-cholesterol levels and the prevalence of asymptomatic intracranial arterial stenosis. Sci Rep. 2017. 7: 573
69. Liebeskind DS, Cotsonis GA, Saver JL, Lynn MJ, Turan TN, Cloft HJ. Collaterals dramatically alter stroke risk in intracranial atherosclerosis. Ann Neurol. 2011. 69: 963-74
70. Lutsep HL, Barnwell S, Mawad M, Chiu D, Hartmann M, Hacke W. Stenting of symptomatic atherosclerotic lesions in the vertebral or intracranial arteries (SSYLVIA): Study results. Stroke. 2004. 35: 1388-92
71. Lylyk P, Cohen JE, Ceratto R, Ferrario A, Miranda C. Angioplasty and stent placement in intracranial atherosclerotic stenoses and dissections. AJNR Am J Neuroradiol. 2002. 23: 430-6
72. Marks MP, Marcellus M, Norbash AM, Steinberg GK, Tong D, Albers GW. Outcome of angioplasty for atherosclerotic intracranial stenosis. Stroke. 1999. 30: 1065-9
73. Marks MP, Wojak JC, Al-Ali F, Jayaraman M, Marcellus ML, Connors JJ. Angioplasty for symptomatic intracranial stenosis: Clinical outcome. Stroke. 2006. 37: 1016-20
74. Marquardt L, Kuker W, Chandratheva A, Geraghty O, Rothwell PM. Incidence and prognosis of > or = 50% symptomatic vertebral or basilar artery stenosis: Prospective population-based study. Brain. 2009. 132: 982-8
75. Mazighi M, Labreuche J, Gongora-Rivera F, Duyckaerts C, Hauw JJ, Amarenco P. Autopsy prevalence of intracranial atherosclerosis in patients with fatal stroke. Stroke. 2008. 39: 1142-7
76. Mazighi M, Tanasescu R, Ducrocq X, Vicaut E, Bracard S, Houdart E. Prospective study of symptomatic atherothrombotic intracranial stenoses: The GESICA study. Neurology. 2006. 66: 1187-91
77. Meng R, Asmaro K, Meng L, Liu Y, Ma C, Xi C. Upper limb ischemic preconditioning prevents recurrent stroke in intracranial arterial stenosis. Neurology. 2012. 79: 1853-61
78. Miyawaki S, Imai H, Shimizu M, Yagi S, Ono H, Hukasa A. Genetic variant RNF213 c.14576G>A in various phenotypes of intracranial major artery stenosis/occlusion. Stroke. 2013. 44: 2894-7
79. Miyawaki S, Imai H, Takayanagi S, Mukasa A, Nakatomi H, Saito N. Identification of a genetic variant common to moyamoya disease and intracranial major artery stenosis/occlusion. Stroke. 2012. 43: 3371-4
80. Mori T, Fukuoka M, Kazita K, Mori K. Follow-up study after intracranial percutaneous transluminal cerebral balloon angioplasty. AJNR Am J Neuroradiol. 1998. 19: 1525-33
81. Mori T, Kazita K, Chokyu K, Mima T, Mori K. Short-term arteriographic and clinical outcome after cerebral angioplasty and stenting for intracranial vertebrobasilar and carotid atherosclerotic occlusive disease. AJNR Am J Neuroradiol. 2000. 21: 249-54
82. Nguyen-Huynh MN, Wintermark M, English J, Lam J, Vittinghoff E, Smith WS. How accurate is CT angiography in evaluating intracranial atherosclerotic disease?. Stroke. 2008. 39: 1184-8
83. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018. 378: 11-21
84. Ogasawara K, Ogawa A, Yoshimoto T. Cerebrovascular reactivity to acetazolamide and outcome in patients with symptomatic internal carotid or middle cerebral artery occlusion: A xenon-133 single-photon emission computed tomography study. Stroke. 2002. 33: 1857-62
85. Powers WJ, Clarke WR, Grubb RL, Videen TO, Adams HP, Derdeyn CP. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: The Carotid Occlusion Surgery Study randomized trial. JAMA. 2011. 306: 1983-92
86. Qiao Y, Zeiler SR, Mirbagheri S, Leigh R, Urrutia V, Wityk R. Intracranial plaque enhancement in patients with cerebrovascular events on high-spatial-resolution MR images. Radiology. 2014. 271: 534-42
87. Qureshi AI, Caplan LR. Intracranial atherosclerosis. Lancet. 2014. 383: 984-98
88. Qureshi AI, Ziai WC, Yahia AM, Mohammad Y, Sen S, Agarwal P. Stroke-free survival and its determinants in patients with symptomatic vertebrobasilar stenosis: A multicenter study. Neurosurgery. 2003. 52: 1033-9 discussion 1039-40
89. Ritz K, Denswil NP, Stam OC, van Lieshout JJ, Daemen MJ. Cause and mechanisms of intracranial atherosclerosis. Circulation. 2014. 130: 1407-14
90. Roher AE, Esh C, Rahman A, Kokjohn TA, Beach TG. Atherosclerosis of cerebral arteries in Alzheimer disease. Stroke. 2004. 35: 2623-7
91. Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The Northern Manhattan Stroke Study. Stroke. 1995. 26: 14-20
92. Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol. 2000. 21: 643-6
93. Sheehan JP. Journal of neurosurgery’s top 25 highly cited articles on gamma knife surgery for meningioma. J Neurosurg. 2017. 27: 1-2
94. Singh R, McLelland MD, De La Peña NM, Pollock JR, Catapano JS, Srinivasan VM. Research advances in the diagnosis and treatment of moyamoya disease: A bibliometric analysis. Neurosurg Rev. 2022. 45: 1977-85
95. Takis C, Kwan ES, Pessin MS, Jacobs DH, Caplan LR. Intracranial angioplasty: Experience and complications. AJNR Am J Neuroradiol. 1997. 18: 1661-8
96. Thijs VN, Albers GW. Symptomatic intracranial atherosclerosis: Outcome of patients who fail antithrombotic therapy. Neurology. 2000. 55: 490-7
97. Tsang AC, Orru E, Klostranec JM, Yang IH, Lau KK, Pong Tsanget FC. Thrombectomy outcomes of intracranial atherosclerosis-related occlusions. Stroke. 2019. 50: 1460-6
98. Turan TN, Cotsonis G, Lynn MJ, Chaturvedi S, Chimowitz M. Relationship between blood pressure and stroke recurrence in patients with intracranial arterial stenosis. Circulation. 2007. 115: 2969-75
99. Turk AS, Levy EI, Albuquerque FC, Pride GL, Woo H, Welch BG. Influence of patient age and stenosis location on wingspan in-stent restenosis. AJNR Am J Neuroradiol. 2008. 29: 23-7
100. Voetsch B, DeWitt LD, Pessin MS, Caplan LR. Basilar artery occlusive disease in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 2004. 61: 496-504
101. Wang Y, Mambiya M, Li Q, Yang L, Jia H, Han Y. RNF213 p.R4810K Polymorphism and the risk of moyamoya disease, intracranial major artery stenosis/occlusion, and quasi-moyamoya disease: A meta-analysis. J Stroke Cerebrovasc Dis. 2018. 27: 2259-70
102. Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: The Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke. 2014. 45: 663-9
103. White H, Boden-Albala B, Wang C, Elkind MS, Rundek T, Wringht CB. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005. 111: 1327-31
104. Wingo AP, Fan W, Duong DM, Gerasimov ES, Dammer EB, Liu Y. Shared proteomic effects of cerebral atherosclerosis and Alzheimer’s disease on the human brain. Nat Neurosci. 2020. 23: 696-700
105. Wityk RJ, Lehman D, Klag M, Coresh J, Ahn H, Litt B. Race and sex differences in the distribution of cerebral atherosclerosis. Stroke. 1996. 27: 1974-80
106. Wolff Fernandes F, Krauss JK. Microvascular decompression: A bibliometric analysis of the 100 most cited articles. World Neurosurg. 2022. 64: e671
107. Wong KS, Gao S, Chan YL, Hansberg T, Lam WW, Droste DW. Mechanisms of acute cerebral infarctions in patients with middle cerebral artery stenosis: A diffusion-weighted imaging and microemboli monitoring study. Ann Neurol. 2002. 52: 74-81
108. Wong KS, Huang YN, Gao S, Lam WW, Chan YL, Kay R. Intracranial stenosis in Chinese patients with acute stroke. Neurology. 1998. 50: 812-3
109. Wong KS, Li H. Long-term mortality and recurrent stroke risk among Chinese stroke patients with predominant intracranial atherosclerosis. Stroke. 2003. 34: 2361-6
110. Wong KS, Li H, Chan YL, Ahuja A, Lam WW, Wong A. Use of transcranial Doppler ultrasound to predict outcome in patients with intracranial large-artery occlusive disease. Stroke. 2000. 31: 2641-7
111. Wong KS, Li H, Lam WW, Chan YL, Kay R. Progression of middle cerebral artery occlusive disease and its relationship with further vascular events after stroke. Stroke. 2002. 33: 532-6
112. Wong KS, Ng PW, Tang A, Liu R, Yeung V, Tomlinson B. Prevalence of asymptomatic intracranial atherosclerosis in high-risk patients. Neurology. 2007. 68: 2035-8
113. Wong KS, Chen C, Fu J, Chang HM, Suwanwela NC, Huang YN. Clopidogrel plus aspirin versus aspirin alone for reducing embolisation in patients with acute symptomatic cerebral or carotid artery stenosis (CLAIR study): A randomised, open-label, blinded-endpoint trial. Lancet Neurol. 2010. 9: 489-97
114. Wong LK. Global burden of intracranial atherosclerosis. Int J Stroke. 2006. 1: 158-9
115. Wu F, Song H, Ma Q, Xiao J, Jiang T, Huang X. Hyperintense plaque on intracranial vessel wall magnetic resonance imaging as a predictor of artery-to-artery embolic infarction. Stroke. 2018. 49: 905-11
116. Xu WH, Li ML, Gao S, Ni J, Yao M, Zhou LX. Middle cerebral artery intraplaque hemorrhage: Prevalence and clinical relevance. Ann Neurol. 2012. 71: 195-8
117. Xu WH, Li ML, Gao S, Ni J, Zhou LX, Yao M. In vivo high-resolution MR imaging of symptomatic and asymptomatic middle cerebral artery atherosclerotic stenosis. Atherosclerosis. 2010. 212: 507-11
118. Yamauchi H, Fukuyama H, Nagahama Y, Nabatame H, Nakamura K, Yamamoto Y. Evidence of misery perfusion and risk for recurrent stroke in major cerebral arterial occlusive diseases from PET. J Neurol Neurosurg Psychiatry. 1996. 61: 18-25
119. Yamauchi H, Fukuyama H, Nagahama Y, Nabatame H, Ueno M, Nishizawa S. Significance of increased oxygen extraction fraction in five-year prognosis of major cerebral arterial occlusive diseases. J Nucl Med. 1999. 40: 1992-8
120. Yarchoan M, Xie SX, Kling MA, Toledo JB, Wolk DA, Lee EB. Cerebrovascular atherosclerosis correlates with Alzheimer pathology in neurodegenerative dementias. Brain. 2012. 135: 3749-56
121. Yoo JH, Chung CS, Kang SS. Relation of plasma homocyst(e) ine to cerebral infarction and cerebral atherosclerosis. Stroke. 1998. 29: 2478-83
122. Yoon W, Kim SK, Park MS, Kim BC, Kang HK. Endovascular treatment and the outcomes of atherosclerotic intracranial stenosis in patients with hyperacute stroke. Neurosurgery. 2015. 76: 680-6 discussion 686
123. Zaidat OO, Fitzsimmons BF, Woodward BK, Wang Z, Killer-Oberpfalzer M, Wakhloo A. Effect of a balloon-expandable intracranial stent vs medical therapy on risk of stroke in patients with symptomatic intracranial stenosis: The VISSIT randomized clinical trial. JAMA. 2015. 313: 1240-8
124. Zaidat OO, Klucznik R, Alexander MJ, Chaloupka J, Lutsep H, Barnwell S. The NIH registry on use of the Wingspan stent for symptomatic 70-99% intracranial arterial stenosis. Neurology. 2008. 70: 1518-24