- Department of Neurosurgery, Kansai Medical University, Hirakata, Japan.
Correspondence Address:
Masahiro Nonaka, Department of Neurosurgery, Kansai Medical University, Hirakata, Japan.
DOI:10.25259/SNI_1060_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Haruka Iwamura, Masahiro Nonaka, Yi Li, Katsuya Ueno, Junichi Takeda, Tetsuo Hashiba, Akio Asai. A case of acute hydrocephalus due to a giant prolactinoma rescued by transventricular neuroendoscopic tumorectomy. 27-Jan-2023;14:30
How to cite this URL: Haruka Iwamura, Masahiro Nonaka, Yi Li, Katsuya Ueno, Junichi Takeda, Tetsuo Hashiba, Akio Asai. A case of acute hydrocephalus due to a giant prolactinoma rescued by transventricular neuroendoscopic tumorectomy. 27-Jan-2023;14:30. Available from: https://surgicalneurologyint.com/surgicalint-articles/12126/
Abstract
Background: A giant prolactinoma extending to the suprasellar area and causing hydrocephalus may be life-threatening and should be treated promptly. A case of a giant prolactinoma with acute hydrocephalus that underwent transventricular neuroendoscopic tumor resection followed by cabergoline administration is presented.
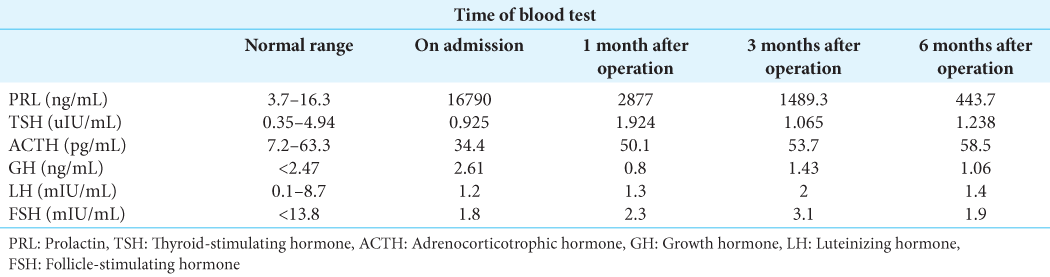
Case Description: A 21-year-old man had a headache lasting for about a month. He gradually developed nausea and disturbance of consciousness. Magnetic resonance imaging showed a contrast-enhanced lesion that extended from the intrasellar space to the suprasellar space and into the third ventricle. The tumor obstructed the foramen of Monro and caused hydrocephalus. A blood test showed marked elevation of prolactin (16,790 ng/mL). The tumor was diagnosed as a prolactinoma. The tumor in the third ventricle had formed a cyst, and the cyst wall blocked the right foramen of Monro. The cystic component of the tumor was resected using an Olympus VEF-V flexible neuroendoscope. The histological diagnosis was pituitary adenoma. The hydrocephalus improved rapidly and his consciousness became clear. After the operation, he was started on cabergoline. The tumor size subsequently decreased.
Conclusion: Prompt partial resection of the giant prolactinoma by transventricular neuroendoscopy resulted in early improvement of hydrocephalus with less invasiveness, allowing subsequent treatment with cabergoline.
Keywords: Endoscopy, Hydrocephalus, Prolactinoma
INTRODUCTION
A giant pituitary adenoma is defined as one that is >40 mm in its greatest dimension. It accounts for 5–15% of all pituitary adenomas.[
CASE PRESENTATION
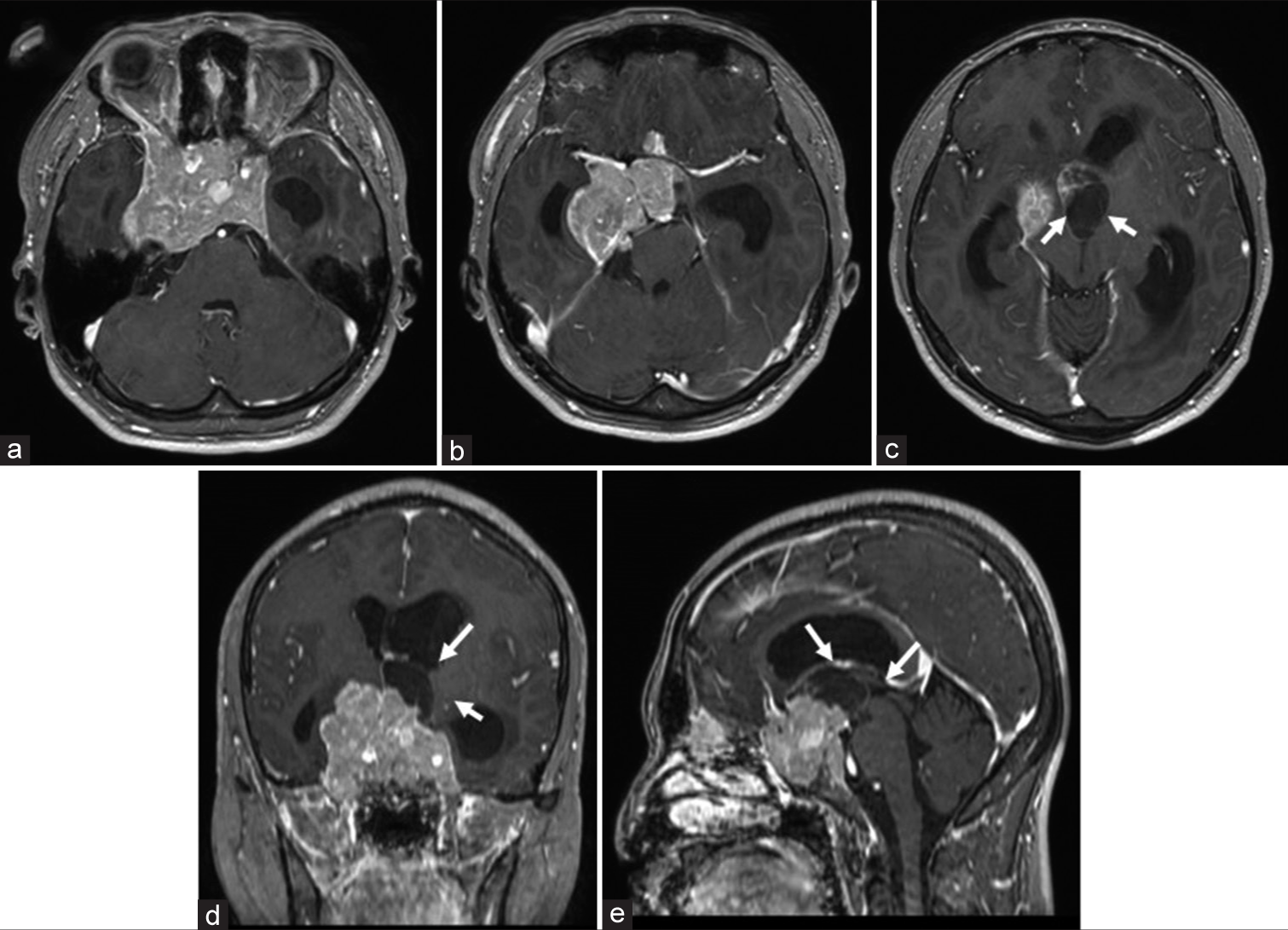
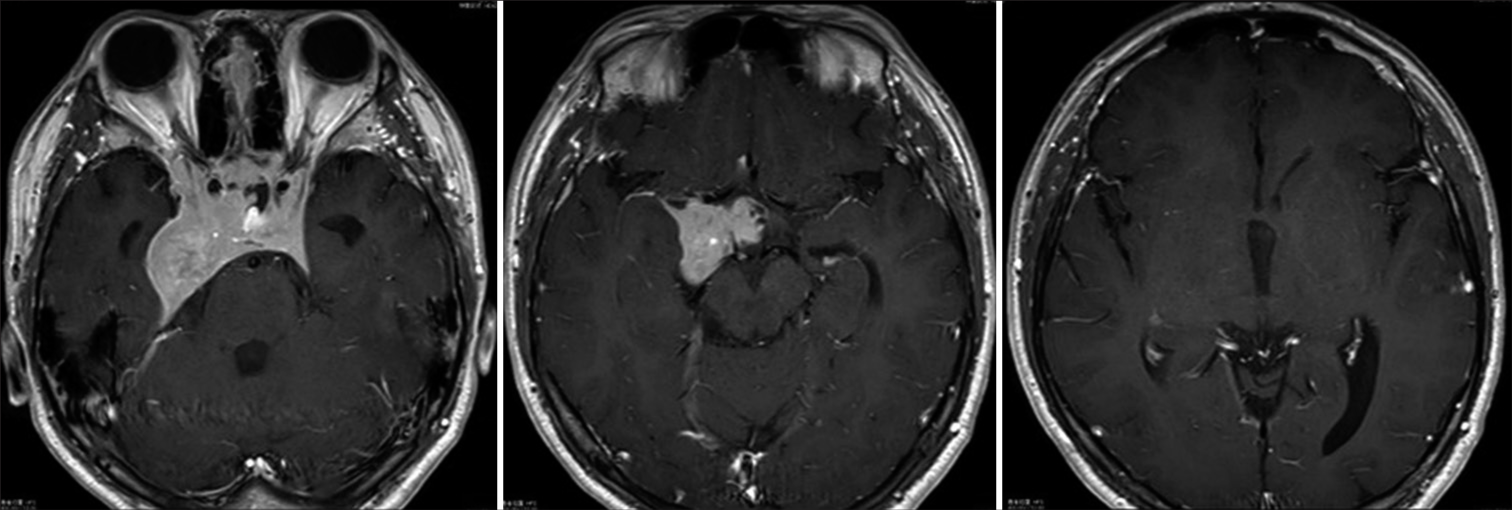
A 21-year-old man with no medical history had a headache that lasted about a month. During the course, he experienced nausea and a mild disturbance of consciousness, and magnetic resonance imaging (MRI) was performed at a nearby clinic. The MRI showed a large tumor in the sella and surrounding region and he was referred to our hospital. His level of consciousness assessed by the Glasgow Coma Scale was 14 (E4 V4 M6). He had no significant visual disturbances at bedside examination. MRI taken at our hospital showed a contrast-enhanced lesion extending from the intrasellar area to the suprasellar area. The maximum tumor diameter was 53 mm. The cystic component of the tumor occupied the third ventricle and obstructed the foramen of Monro, causing acute hydrocephalus [
Figure 1:
Magnetic resonance imaging T1-CE (contrast-enhanced) axial images (a-c), coronal image (d), and sagittal image (e). The tumor consists of a solid component and a cystic component, extending from the intrasellar turcica to the suprasellar turcica. It has also spread to both internal carotid arteries and the right cavernous sinus. The cystic components of the tumor (arrows) occupy the third ventricle causing acute hydrocephalus.
Surgical findings
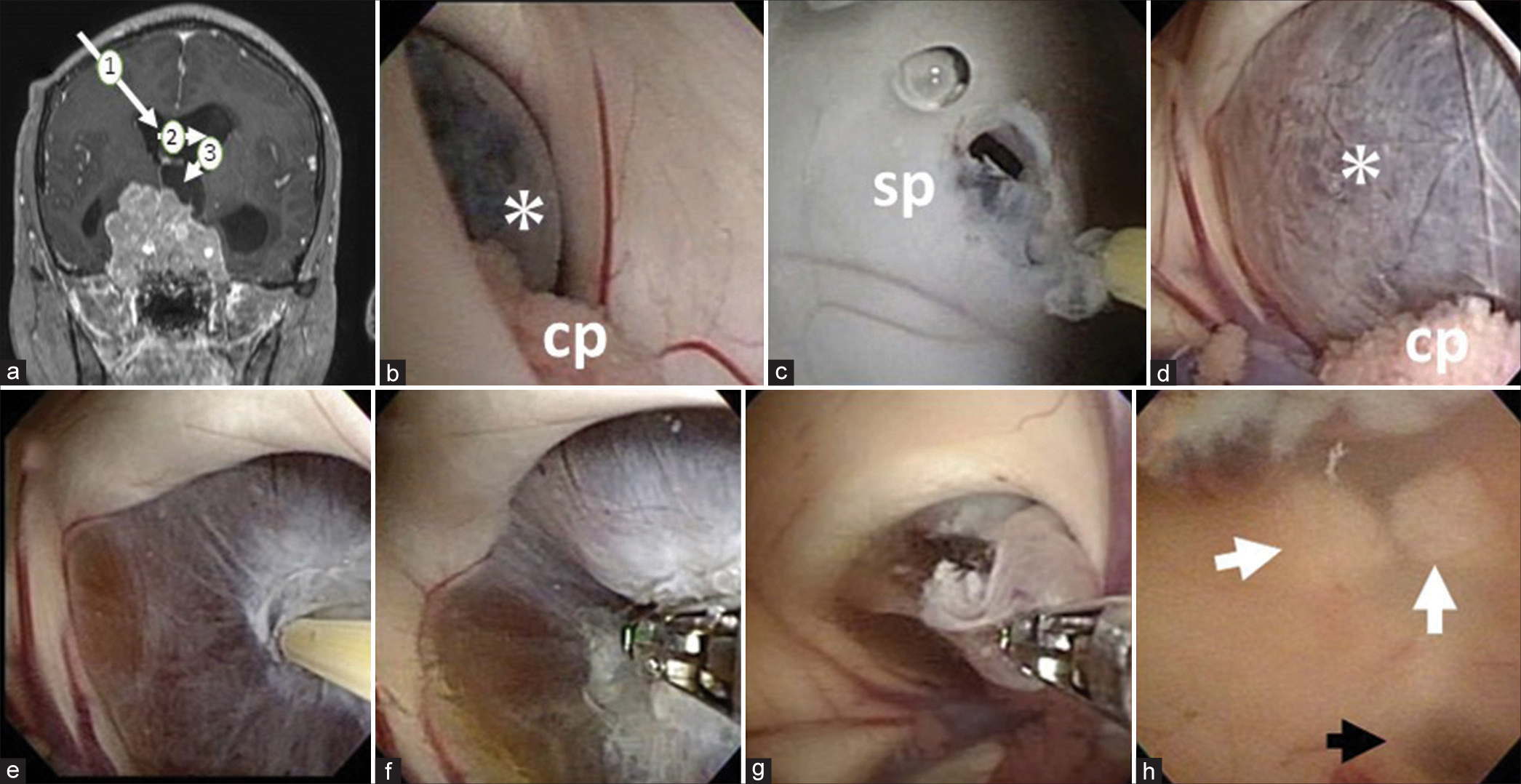
The patient was placed in the supine position under general anesthesia. His head was set vertex up without rotation. A planned right anterior horn puncture was performed under navigational guidance [
Figure 2:
(a): The route of entry of the flexible neuroendoscope is illustrated. First, the right ventricle was punctured (1) and then fenestration of the septum pellucidum was performed to enter the left ventricle (2). The cyst was then removed from the left foramen of Monro (3). (b): A purple-colored cystic wall blocking the foramen of Monro (asterisk) was observed. cp: Choroid plexus. (c) The septum pellucidum was fenestrated by RAF electrode. sp: septum pellucidum. (d) Left foramen of Monro enlarged by the cyst (asterisk). cp: Choroid plexus: Cyst wall is cauterized with RAF electrodes (e), and perforated with biopsy forceps (f). The cyst wall is excised with biopsy forceps (g). (h) Image of the third ventricle obtained after cyst removal. The mammillary body (white arrow) and aqueduct are confirmed (black arrow).
The cyst wall was cauterized with RAF electrodes [
Postoperative course
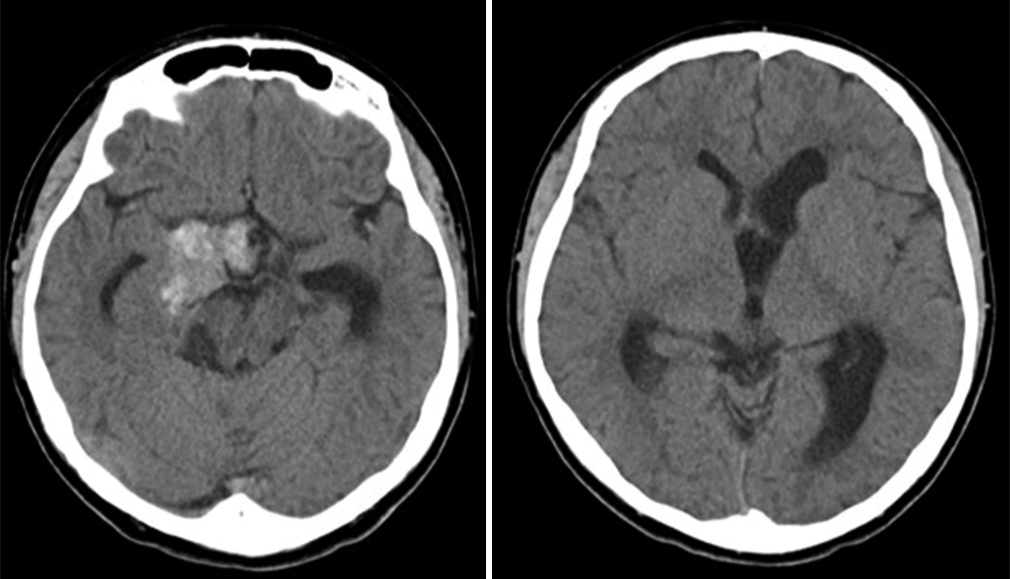
Cabergoline 0.25 mg was started orally every week from 2 days after surgery until now. Head CT taken 7 days after surgery showed improvement in acute hydrocephalus and reduction in ventricle size [
DISCUSSION
Giant pituitary adenomas are often approached by extended transsphenoidal surgery or simultaneous craniotomy with transsphenoidal surgery. In endoscopic transsphenoidal surgery, it is difficult to remove tumors that have extended to the suprasellar area, ventricles, or cavernous sinus, and there is also a possibility of postoperative bleeding from residual tumors. It has been reported that simultaneous surgery is preferable because it may be possible to remove the tumor by adding craniotomy to transsphenoidal surgery. Simultaneous surgery with a transsphenoidal approach includes microscopic surgery,[
In addition, pituitary function was preserved in this case, so no postoperative hormone replacement therapy was required, and early discharge from the hospital was possible.
CONCLUSION
Rapid partial resection of a giant prolactinoma with cystic component by transventricular neuroendoscopy resulted in early improvement of hydrocephalus and allowed subsequent treatment with cabergoline.
Ethical approval and informed consent
This study was approved by the Ethics Committee of Kansai Medical University (No. 2020055). Need for written patient consent was waived by the Ethics Committee because data were deidentified.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ceylan S, Sen HE, Ozsoy B, Ceylan EC, Ergen A, Selek A. Endoscopic approach for giant pituitary adenoma: Clinical outcomes of 205 patients and comparison of two proposed classification systems for preoperative prediction of extent of resection. J Neurosurg. 2022. 136: 786-800
2. Constantino ER, Leal R, Ferreira CC, Acioly MA, Landeiro JA. Surgical outcomes of the endoscopic endonasal transsphenoidal approach for large and giant pituitary adenomas: Institutional experience with special attention to approach-related complications. Arq Neuropsiquiatr. 2016. 74: 388-95
3. Guinto-Nishimura GY, Caballero-Delgado S, EguiluzMelendez AG, Ortega-Porcayo LA, Valencia-Ramos C, AragonArreola JF. Combined endoscopic transsphenoidal and tubular retractor-assisted transventricular approach for giant pituitary adenomas. World Neurosurg. 2021. 155: e761-9
4. Han S, Gao W, Jing Z, Wang Y, Wu A. How to deal with giant pituitary adenomas: Transsphenoidal or transcranial, simultaneous or two-staged?. J Neurooncol. 2017. 132: 313-21
5. Huang HY, Lin SJ, Zhao WG, Wu ZB. Cabergoline versus bromocriptine for the treatment of giant prolactinomas: A quantitative and systematic review. Metab Brain Dis. 2018. 33: 969-96
6. Koktekir E, Karabagli H, Ozturk K. Simultaneous transsphenoidal and transventricular endoscopic approaches for giant pituitary adenoma with hydrocephalus. J Craniofac Surg. 2015. 26: e39-42
7. Koutourousiou M, Gardner PA, Fernandez-Miranda JC, Paluzzi A, Wang EW, Snyderman CH. Endoscopic endonasal surgery for giant pituitary adenomas: Advantages and limitations. J Neurosurg. 2013. 118: 621-31
8. Matsumoto T, Ono T, Onodera T, Oda M, Takahashi M, Omae T. Transventricular preforniceal approach combined with endoscopic transnasal surgery for a giant pituitary adenoma: A case report and literature review. NMC Case Rep J. 2021. 8: 827-33
9. Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA. Diagnosis and treatment of hyperprolactinemia: An endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011. 96: 273-88
10. Moraes AB, Silva CM, Neto LV, Gadelha MR. Giant prolactinomas: The therapeutic approach. Clin Endocrinol (Oxf). 2013. 79: 447-56
11. Romano A, Chibbaro S, Marsella M, Oretti G, Spiriev T, Iaccarino C. Combined endoscopic transsphenoidaltransventricular approach for resection of a giant pituitary macroadenoma. World Neurosurg. 2010. 74: 161-4
12. Shimon I. Giant prolactinomas. Neuroendocrinology. 2019. 109: 51-6
13. Takeuchi K, Nagatani T, Watanabe T, Okumura E, Sato Y, Wakabayashi T. A purely endoscopic and simultaneous transsphenoidal and transcranial keyhole approach for giant pituitary adenoma resection: A technical case report. NMC Case Rep J. 2015. 2: 101-5
14. Tang OY, Hsueh WD, Eloy JA, Liu JK. Giant pituitary adenoma-special considerations. Otolaryngol Clin North Am. 2022. 55: 351-79
15. Witek P, Zielinski G, Maksymowicz M, Zgliczynski W. Transsphenoidal surgery for a life-threatening prolactinoma apoplexy during pregnancy. Neuro Endocrinol Lett. 2012. 33: 483-8
16. Yamada E, Akutsu H, Kino H, Tanaka S, Miyamoto H, Hara T. Combined simultaneous endoscopic endonasal and microscopic transventricular surgery using a port retractor system for giant pituitary adenoma: A technical case report. Surg Neurol Int. 2021. 12: 90