- Departments of Neurosurgery, Hamad General Hospital, Hamad Medical Corporation, Doha,
- Departments of Neurosurgery, Weill Cornell Medical College, Ar-Rayyan, Qatar,
- Departments of Neurosurgery, Michigan State University, Michigan, USA.
Correspondence Address:
Ahmed Taha Elsayed Shaaban
Departments of Neurosurgery, Hamad General Hospital, Hamad Medical Corporation, Doha,
Departments of Neurosurgery, Weill Cornell Medical College, Ar-Rayyan, Qatar,
Departments of Neurosurgery, Michigan State University, Michigan, USA.
DOI:10.25259/SNI_173_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Taha Elsayed Shaaban, Ahmed Doomi, Sirajeddin Belkheir. A case of cervical myelopathy following chronic hypertrophic non-union type 2 odontoid fracture managed with posterior C1 decompression and C1-3 instrumentation: Case report and brief review of literature. 30-May-2020;11:132
How to cite this URL: Ahmed Taha Elsayed Shaaban, Ahmed Doomi, Sirajeddin Belkheir. A case of cervical myelopathy following chronic hypertrophic non-union type 2 odontoid fracture managed with posterior C1 decompression and C1-3 instrumentation: Case report and brief review of literature. 30-May-2020;11:132. Available from: https://surgicalneurologyint.com/surgicalint-articles/10059/
Abstract
Background: Type 2 odontoid fractures are the most common type of fracture of the axis. In rare cases, nonunion of a type 2 odontoid fracture can be hypertrophic resulting in myelopathy due to cervical cord compression.
Case Description: A 48-year-old male presented with hypertrophic nonunion of a chronic type 2 odontoid fracture resulting in cord compression/myelopathy. This was adequately treated utilizing a C1 decompression and C1-3 instrumented fusion; no anterior procedure was necessary.
Conclusion: Here, we successfully treated a patient with a hypertrophic nonunion of a chronic type 2 odontoid fracture utilizing a posterior only approach consisting of a C1 laminectomy with C1-C3 fusion.
Keywords: Fracture, Hypertrophic, Myelopathy, Non-union, Odontoid
INTRODUCTION
Type 2 odontoid fracture is the most common type of fracture of axis and most common cervical spine fractures in elderly population. Incidence in the USA is estimated 21.4/100,000 inpatient.[
CASE DESCRIPTION
Clinical presentation
A 48-year-old male presented with chronic neck pain and 4 months of progressive myelopathy (i.e., unsteady gait and clumsiness). Two years ago, he had fallen from 2 m height, hitting his head and neck on the ground. Since then, he continued to experience Lhermitte’s signs. On examination, he had no motor or sensory deficits, but exhibited a spastic gait, bilateral Hoffman’s sign, diffuse upper and lower extremity hyperreflexia, and bilateral ankle clonus.
Diagnostic studies
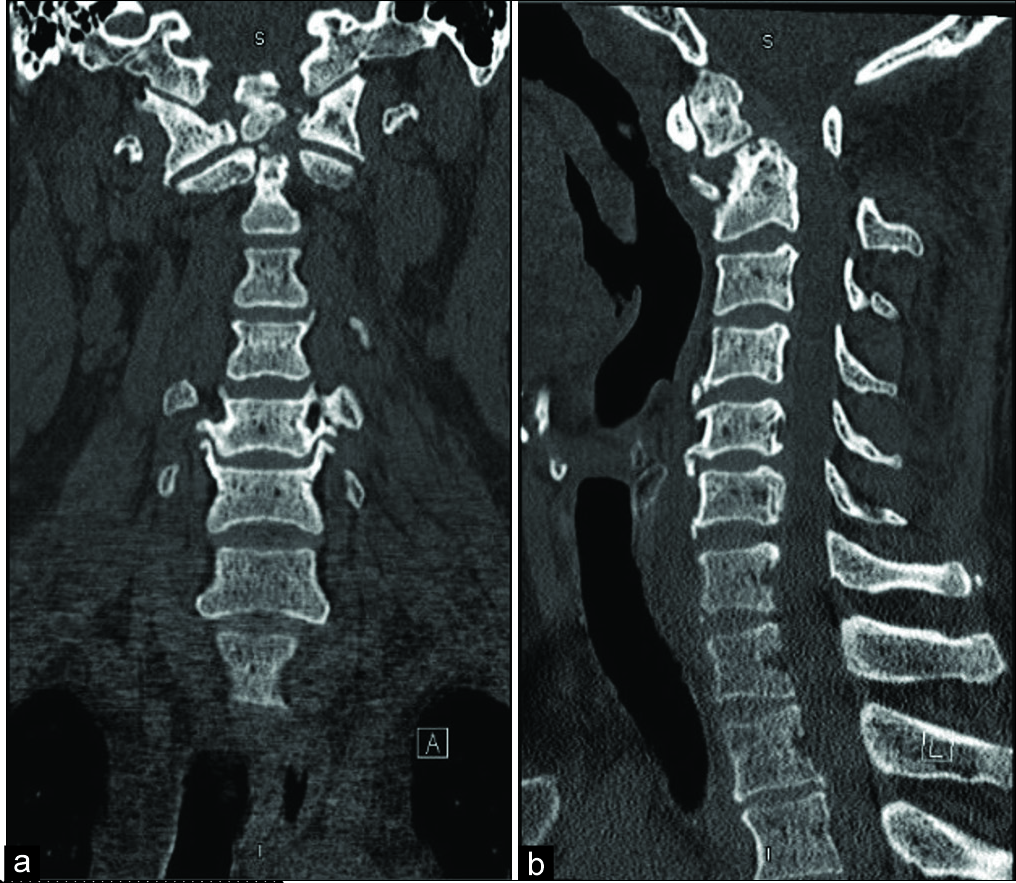
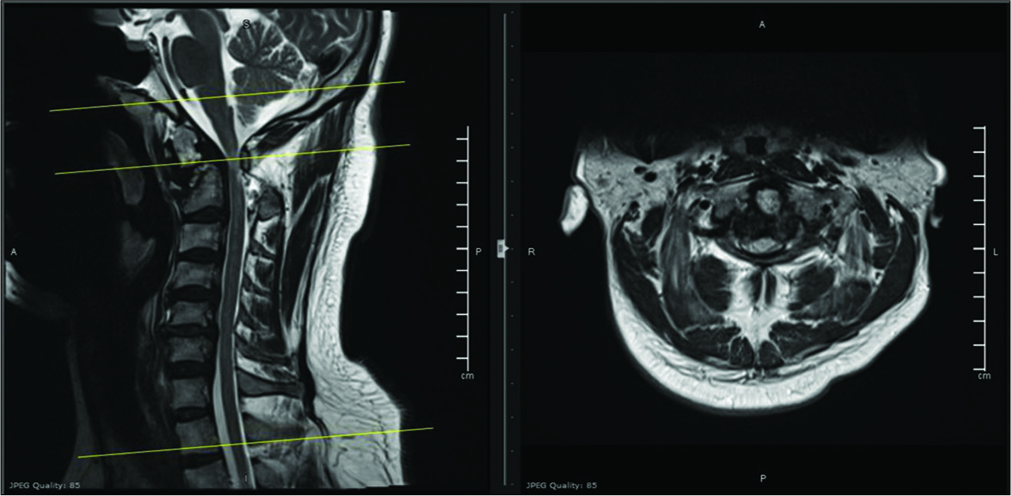
Cervical spine X-ray and computed tomography (CT) studies confirmed an old nonunited displaced fracture at the base of the odontoid process of the C2 vertebra narrowing the spinal canal at the C1-2 level due to displacement of C1 [
Figure 2:
(a) Preoperative computed tomography (CT) cervical spine coronal showing old nonunited fracture at the base of the odontoid process of C2 with narrow spinal canal at C1-2 levels. (b) Preoperative CT cervical spine sagittal showing old nonunited fracture at the base of the odontoid process of C2 with narrow spinal canal at C1-2 levels.
Surgery
The patient underwent awake fiber-optic endotracheal intubation. Intraoperative neurophysiological monitoring included somatosensory evoked and motor evoked potentials.
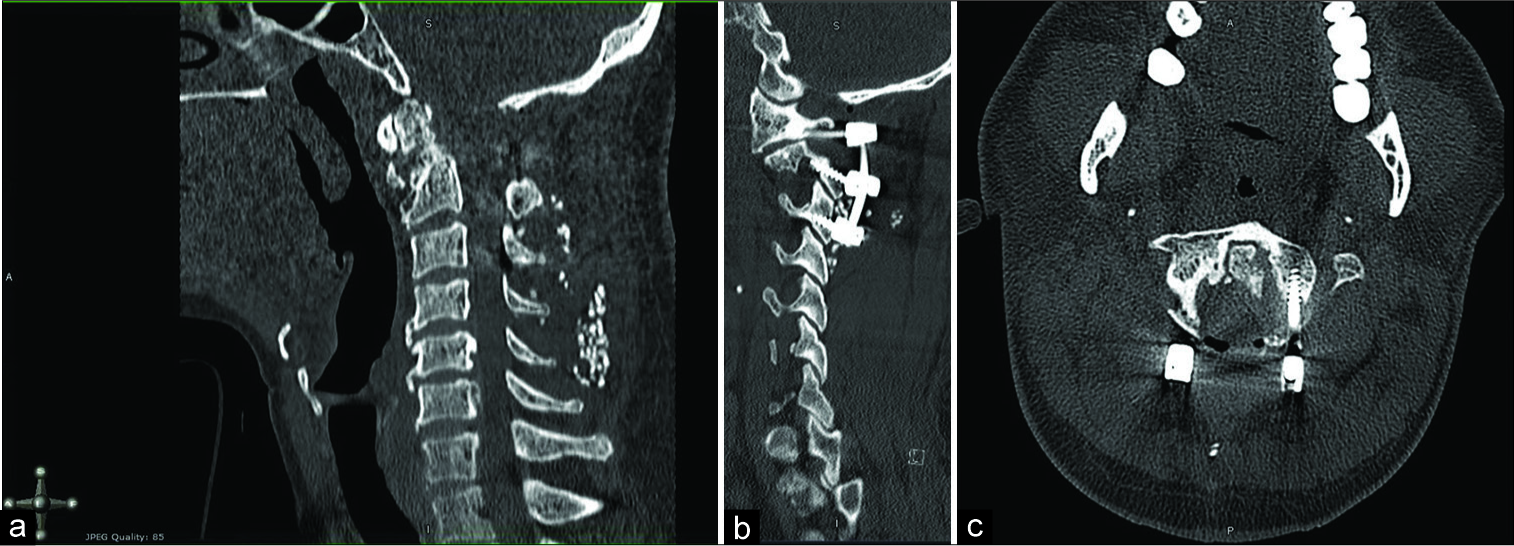
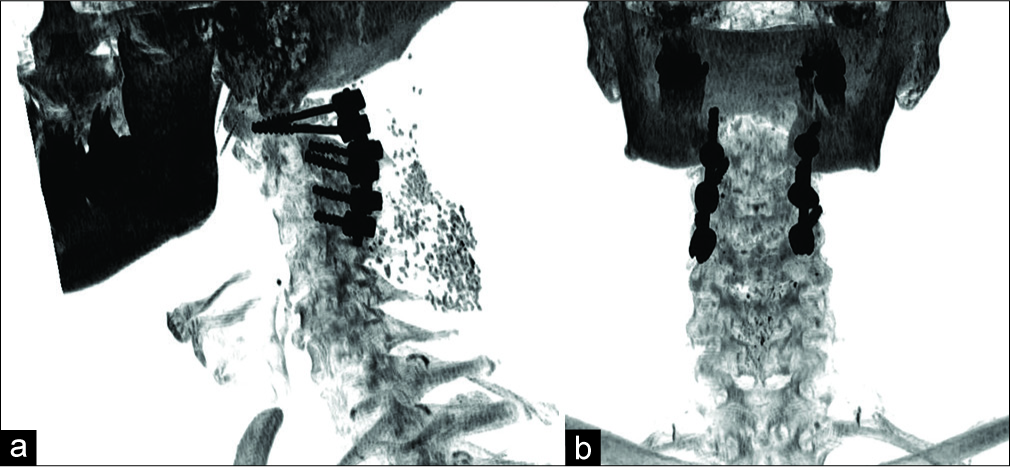
A C1 decompressive laminectomy was performed and all were placed under CT neuronavigation guidance. These included lateral mass screws at C1 applied (32 × 3.5 mm partially threaded), bilateral C2 pars articularis screws (18 × 3.5 mm), and C3 lateral mass screws (16 × 3.5 mm). After the rods were applied, the intraoperative CT showed reduction of the C1/2 malalignment. Routine completion of the Instrumentation and closure followed [
DISCUSSION
Frequency of type 2 odontoid fractures resulting in nonunion
Odontoid fractures are the most common fractures involving axis and are the most frequently encountered cervical spine fractures seen in adults over 65 years of age. Nonoperative management is associated with a high risk of nonunion (i.e., 36.3%).[
Incidence of hypertrophic nonunion of type 2 odontoid fractures
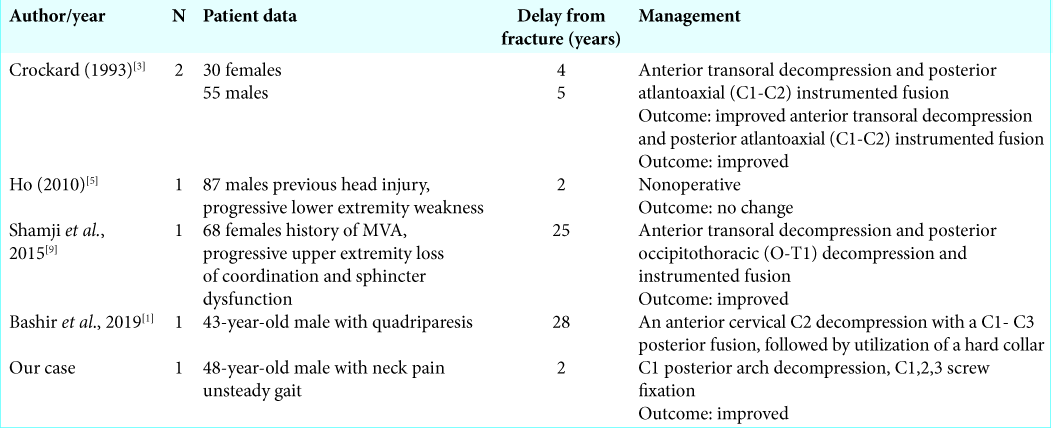
Hypertrophic nonunion of type 2 odontoid fracture is rare. Of five such cases found in the literature, four were managed with anterior decompression/posterior fusion, while one was treated nonsurgically [
Table 1:
(Adopted from Shamji et al., 2015)[
CONCLUSION
We recommend a posterior only approach consisting of a C1 laminectomy with C1-C3 posterior fusion for managing a hypertrophic chronic nonunion of a type 2 odontoid fracture.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bashir SK, Batool SM, Javed G. Chronic hypertrophic malunion of C2 fracture causing cervical quadriparesis; Case report and focused literature review. Surg Neurol Int. 2019. 10: 107-
2. Carvalho AD, Figueiredo J, Schroeder GD, Vaccaro AR, Rodrigues-Pinto R. Odontoid fractures: A critical review of current management and future directions. Clin Spine Surg. 2019. 32: 313-23
3. Crockard HA, Heilman AE, Stevens JM. Progressive myelopathy secondary to odontoid fractures: Clinical, radiological, and surgical features. J Neurosurg. 1993. 78: 579-86
4. Daniels AH, Arthur M, Esmende SM, Vigneswaran H, Palumbo MA. Incidence and cost of treating axis fractures in the United States from 2000 to 2010. Spine. 2014. 39: 1498-505
5. Ho AW, Ho YF. Atlanto-axial deformity secondary to a neglected odontoid fracture: A report of six cases. J Orthop Surg (Hong Kong). 2010. 18: 235-40
6. Hsu WK, Anderson PA. Odontoid fractures: Update on management. J Am Acad Orthop Surg. 2010. 18: 383-94
7. Iyer S, Hurlbert RJ, Albert TJ. Management of odontoid fractures in the elderly: A review of the literature and an evidence-based treatment algorithm. Neurosurgery. 2018. 82: 419-30
8. Robinson Y, Robinson AL, Olerud C. Systematic review on surgical and nonsurgical treatment of Type II odontoid fractures in the elderly. Biomed Res Int. 2014. 2014: 231948-
9. Shamji MF, Alotaibi N, Ghare A, Fehlings MG. Chronic hypertrophic nonunion of the Type II odontoid fracture causing cervical myelopathy: Case report and review of literature. Surg Neurol Int. 2016. 7: S53-6