- Department of Neurosurgery, Shimane University Faculty of Medicine, Izumo, Shimane, Japan.
- Advanced Stroke Center, Shimane University Hospital, Izumo, Shimane, Japan.
- Department of Otorhinolaryngology-Head and Neck Surgery, Shimane University Faculty of Medicine, Izumo, Shimane, Japan.
Correspondence Address:
Masahiro Uchimura, Department of Neurosurgery, Shimane University Faculty of Medicine, Izumo, Shimane, Japan.
DOI:10.25259/SNI_404_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masahiro Uchimura1, Kentaro Hayashi2, Tatsunori Sakamoto3, Hidemasa Nagai1. A case of intraorbital malignant lymphoma biopsied using an endoscopic transnasal approach. 21-Jul-2023;14:259
How to cite this URL: Masahiro Uchimura1, Kentaro Hayashi2, Tatsunori Sakamoto3, Hidemasa Nagai1. A case of intraorbital malignant lymphoma biopsied using an endoscopic transnasal approach. 21-Jul-2023;14:259. Available from: https://surgicalneurologyint.com/surgicalint-articles/12446/
Abstract
Background: While most orbital tumors are primary, some are secondary, including extension or invasion from adjacent sites. The diagnosis varies widely, and the treatment strategy depends on the pathological diagnosis. Transcranial and transorbital surgical approaches are typically used. Recently, a transnasal endoscopic approach has emerged as a viable option. We report a case of an intraorbital tumor treated with endoscopic transnasal biopsy and compare the results with those of other surgical approaches.
Case Description: A 74-year-old woman visited a nearby hospital due to a right eye protrusion and decreased visual acuity. An intraorbital tumor was detected and the patient was referred to our hospital. Head computed tomography revealed a mass along the posterior wall of the right orbital apex. Contrast-enhanced magnetic resonance imaging showed a 37-mm lesion with a uniform contrast effect and no intracranial extension. Intraorbital lymphoma was considered a differential diagnosis, and a biopsy was performed using an endoscopic transnasal approach. The pathological diagnosis was B-cell lymphoma, and chemotherapy was administered.
Conclusion: The endoscopic transnasal approach for intraorbital tumors is less invasive, highly cosmetic, and useful, especially for medial and inferior orbital lesions.
Keywords: Biopsy, Endoscopic transnasal approach, Malignant lymphoma, Orbital tumor
INTRODUCTION
Approximately 90% of orbital tumors are primary; 10% are secondary tumors, including extension or invasion from adjacent sites.[
CASE REPORT
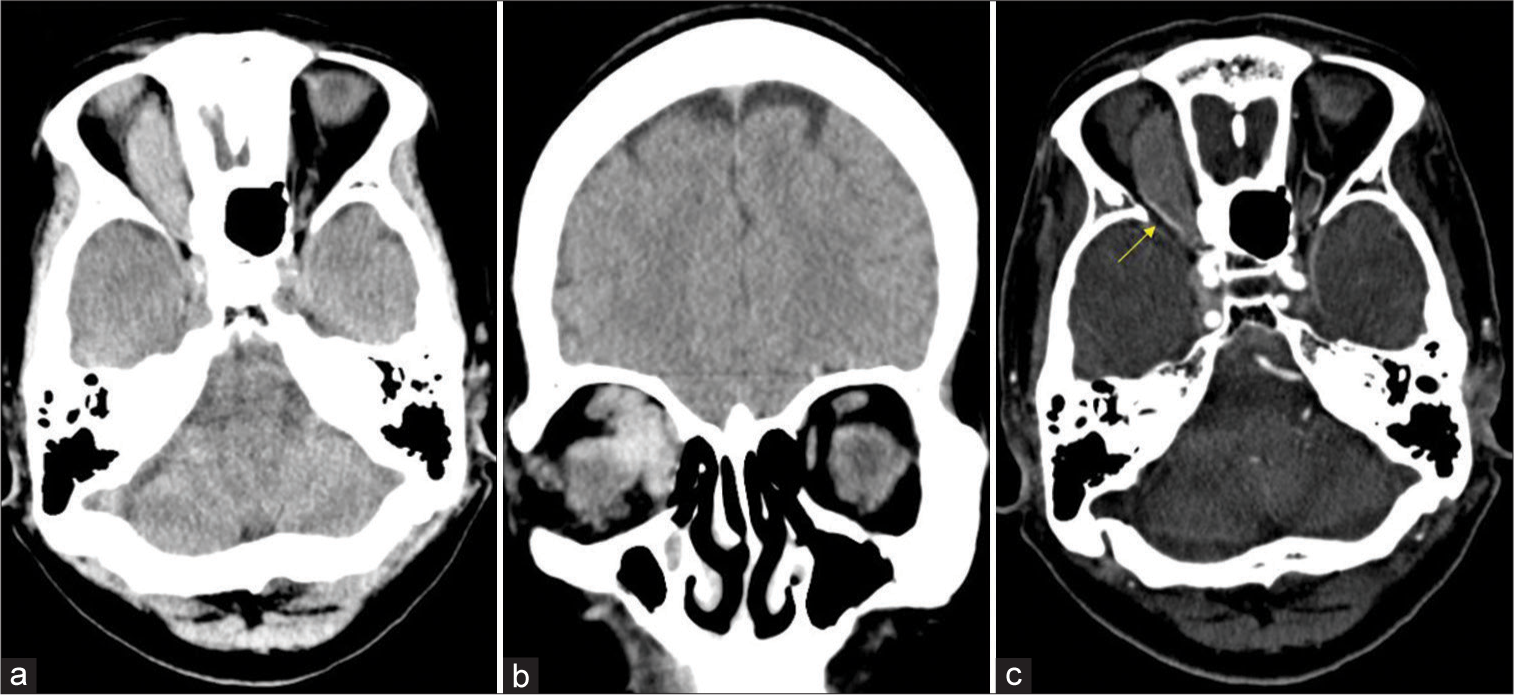
A 74-year-old woman visited a nearby hospital with a 3-month history of right ocular protrusion and decreased right-eye visual acuity. She had no relevant medical history. Based on computed tomography (CT), an intraorbital tumor was suspected, and the patient was referred to our hospital. The patient was conscious and explicit during the initial examination. Right exophthalmos, conjunctival edema, and papillary edema of the optic nerve were observed. No intraocular hypertension was observed. Her corrected visual acuity was 0.3 on the right and 0.6 on the left. Head CT revealed a mass superior to the medial side of the right orbit [
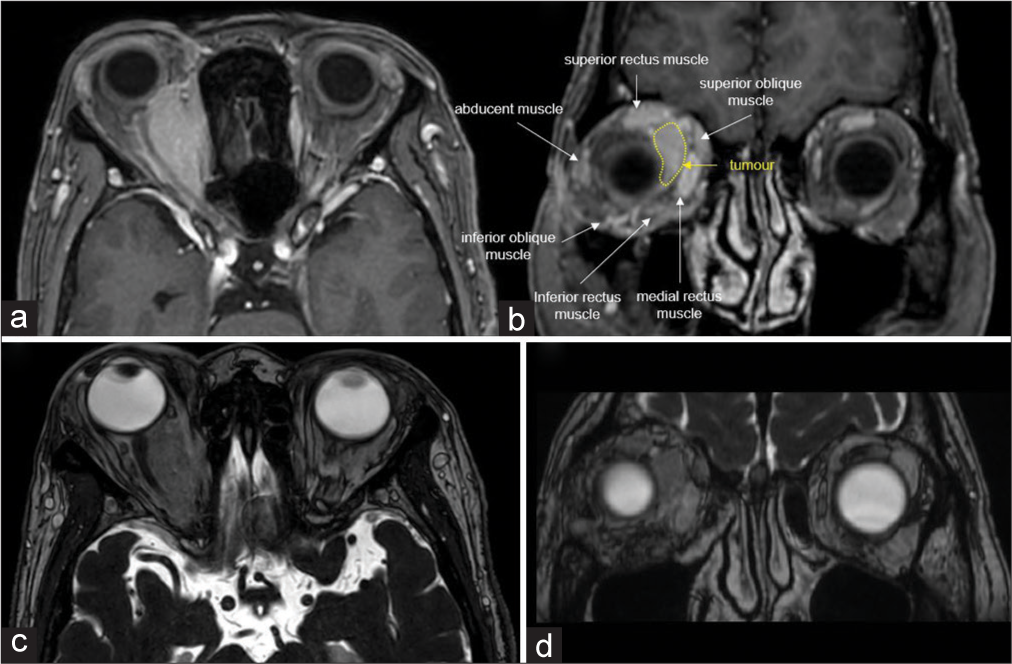
Figure 2:
(a and b) T1-weighted Gd-enhanced magnetic resonance imaging showing a homogeneously enhanced lesion on the superior to medial side of the right orbit. (c and d) Constructive interference in steady-state sequence showing the internal rectus and superior oblique muscles compressed externally by the tumor.
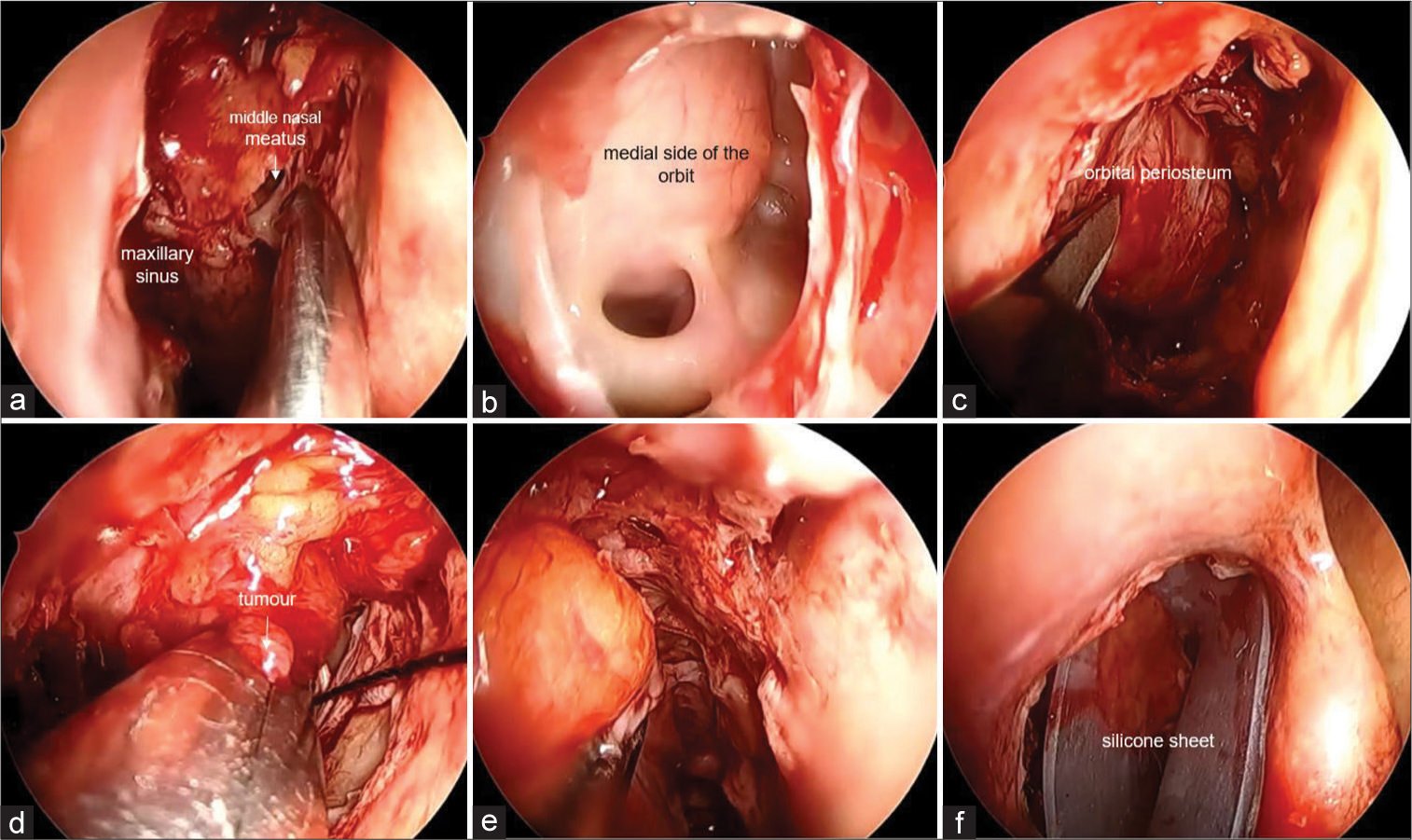
Endoscopic transnasal approach
Bosmin (0.1%) was injected into the incision site of the nasal septal mucosa in the right nasal cavity, and the right maxillary sinus was opened by resecting the uncinate process of the ethmoid [
Figure 3:
(a) The right maxillary sinus entered through the right nasal cavity and was freed by excision of the cribriform stalk. The superior wall of the maxillary sinus is an important landmark because it serves as the inferior wall of the orbit. (b) The middle nasal meatus is punctured to release the ethmoid sinus, exposing the medial side of the orbit. (c) Mucosa of the medial orbit was dissected, and the bone was removed to expose the orbital periosteum. (d) The orbital periosteum was incised, but distinguishing between the fat, tumor, and medial rectus muscle was difficult. The medial rectus muscle and tumor area were bluntly dissected, and the tissue was removed. (e) The exposed orbital contents were partially covered with mucosa. (f) A silicone sheet is placed in an inverted U-shape to complete the surgery.
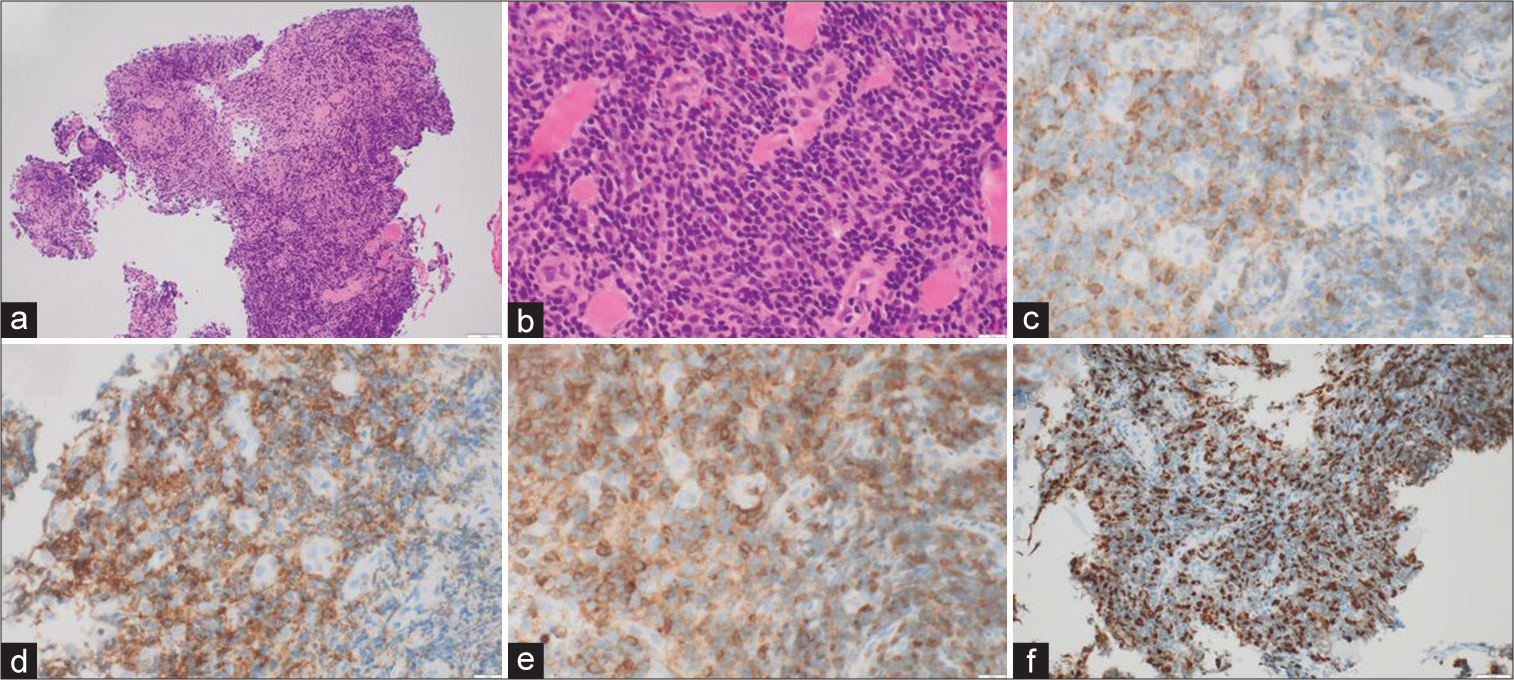
Pathological study
Histopathological examination revealed proliferating lymphocytes with moderate cellular atypia [
First, radiotherapy (40 Gy) was administered to the right intraorbital tumor and neck. We then administered three cycles of rituximab, cyclophosphamide, doxorubicin hydrochloride (hydroxydaunorubicin), vincristine sulfate (Oncovin), and prednisone. Six months after treatment, T1-weighted Gd-enhanced MRI showed that the tumor had shrunk, ocular protrusion had improved, and no evidence of visual acuity or visual field abnormalities was present.
DISCUSSION
Because the diagnosis of orbital tumors is diverse, and treatment strategies differ according to the type of disease, pathological diagnosis is essential. Approximately 90% of orbital tumors are primary; <10% are secondary, including extension or invasion from adjacent sites, and a few are reported to be metastatic.[
In addition to the transcranial and transorbital approaches for treatment, another alternative has been used recently: the endoscopic transnasal approach.[
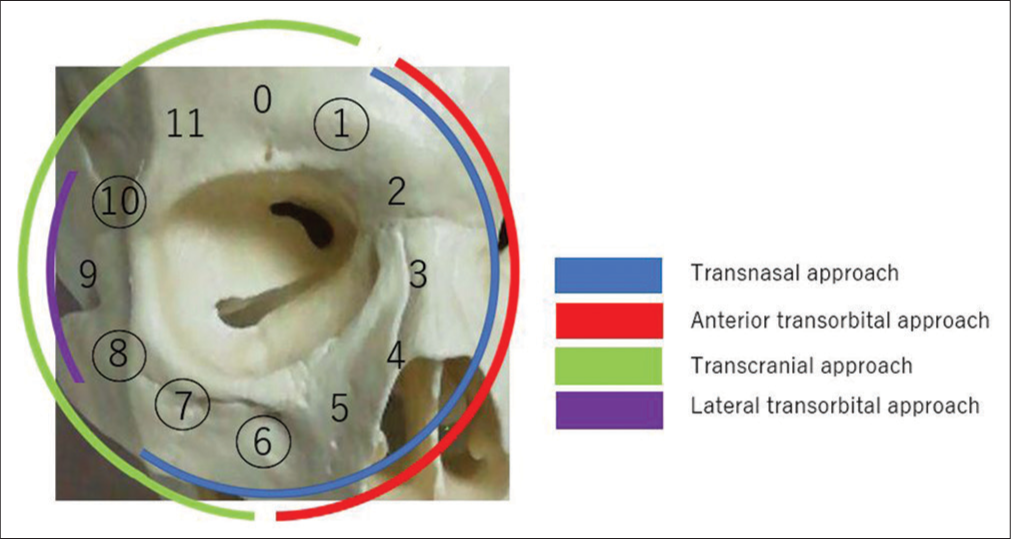
Figure 5:
Schematic diagram created from the report by Paluzzi et al.[
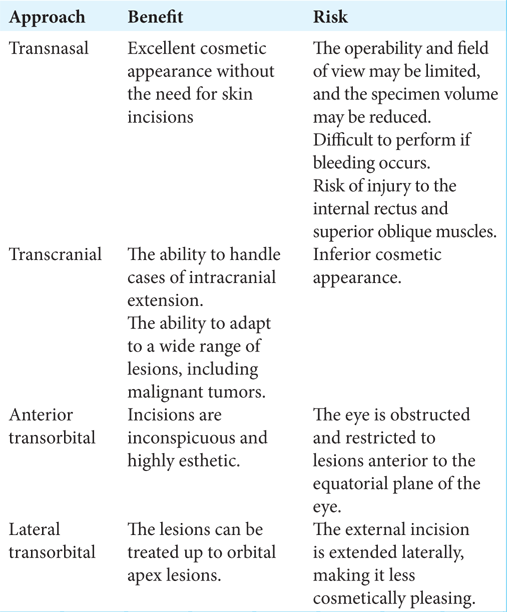
The following is a comparison of each approach from a different perspective. The advantages of the endoscopic transnasal approach are that it requires no skin incision and is highly esthetic. Its disadvantages include less operability, limited field of view, difficulty performing the procedure if bleeding occurs, and risk of injury to the medial rectus and superior oblique muscles [
In contrast, the transcranial approach should be considered for tumors that are located in the lateral and superior orbits, extend intracranially, and are intended for total resection. Recently, the total resection of intraorbital tumors has shown low complication rates.[
CONCLUSION
In addition to the transcranial and transorbital approaches, the endoscopic transnasal approach effectively treats intraorbital tumors. In particular, the endoscopic transnasal approach shows excellent safety and is minimally invasive in biopsy procedures for tumors located in the infraorbital region.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Amemiya T, Hayashida H, Dake Y. Metastatic orbital tumors in Japan: A review of the literature. Ophthalmic Epidemiol. 2002. 9: 35-47
2. Bleier BS, Castelnuovo P, Battaglia P, Turri-Zanoni M, Dallan I, Metson R. Endoscopic endonasal orbital cavernous hemangioma resection: Global experience in techniques and outcomes. Int Forum Allergy Rhinol. 2016. 6: 156-61
3. Castelnuovo P, Dallan I, Locatelli D, Battaglia P, Farneti P, Tomazic PV. Endoscopic transnasal intraorbital surgery: Our experience with 16 cases. Eur Arch Otorhinolaryngol. 2012. 269: 1929-35
4. Goto H. Symptoms, diagnosis and epidemiology or orbital tumor. Ophthalmology. 2022. 64: 33-9
5. Karaki M, Kobayashi R, Mori N. Removal of an orbital apex hemangioma using an endoscopic transethmoidal approach: Technical note. Neurosurgery. 2006. 59: ONSE159-60
6. Margalit N, Ezer H, Fliss DM, Naftaliev E, Nossek E, Kesler A. Orbital tumors treated using transcranial approaches: Surgical technique and neuroophthalmogical results in 41 patients. Neurosurg Focus. 2007. 23: E11
7. Paluzzi A, Gardner PA, Fernandez-Miranda JC, Tormenti MJ, Stefko ST, Snyderman CH. “Round-the-clock” surgical access to the orbit. J Neurol Surg B Skull Base. 2015. 76: 12-24
8. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: The 2002 Montgomery Lecture, part 1. Ophthalmology. 2004. 111: 997-1008
9. Shin M, Kondo K, Hanakita S, Suzukawa K, Kin T, Shojima M. Endoscopic transnasal approach for resection of locally aggressive tumors in the orbit. J Neurosurg. 2015. 123: 748-59
10. Sieskiewicz A, Lyson T, Mariak Z, Rogowski M. Endoscopic trans-nasal approach for biopsy of orbital tumours using image-guided neuro-navigation system. Acta Neurochir (Wien). 2008. 150: 441-5 discussion 445
11. Zhang X, Hua W, Quan K, Yu G, Du Z, Yang Z. Endoscopic endonasal intraconal approach for orbital tumor resection: Case series and systematic review. Front Oncol. 2022. 11: 780551
12. Zoli M, Sollini G, Milanese L, La Corte E, Rustici A, Guaraldi F. Endoscopic approaches to orbital lesions: Case series and systematic literature review. J Neurosurg. 2020. 134: 608-20