- Department of Neurosurgery, Clinical Research Institute, National Hospital Organization, Kyushu Medical Center, Iizuka, Japan
- Department of Neurosurgery, Shimonoseki Municipal Hospital, Shimonoseki, Yamaguchi, Japan
- Department of Neurosurgery, Aso Iizuka Hospital, Iizuka, Japan
- Department of Neurosurgery, Japanese Labour Health Welfare Organization, Kyushu Rosai Hospital, Fukuoka, Japan
Correspondence Address:
Nobuhiro Hata
Department of Neurosurgery, Clinical Research Institute, National Hospital Organization, Kyushu Medical Center, Iizuka, Japan
DOI:10.4103/2152-7806.170468
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fujioka Y, Hata N, Sangatsuda Y, Inoue D, Haga S, Nagata S. A case of metastatic brain tumor in the perfusion territory of superficial temporal artery-middle cerebral artery anastomosis. Surg Neurol Int 25-Nov-2015;6:
How to cite this URL: Fujioka Y, Hata N, Sangatsuda Y, Inoue D, Haga S, Nagata S. A case of metastatic brain tumor in the perfusion territory of superficial temporal artery-middle cerebral artery anastomosis. Surg Neurol Int 25-Nov-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/a-case-of-metastatic-brain-tumor-in-the-perfusion-territory-of/
Abstract
Background:We report a rare case of metastatic tumor in the perfusion territory of superficial temporal artery-middle cerebral artery (STA-MCA) anastomosis.
Case Description:A 63-year-old man, who had undergone left STA-MCA anastomosis in the treatment of occlusion of internal carotid artery 4 years ago, presented with a hyperintense lesion on T2-weighted image in the left frontal lobe, the perfusion territory of the prior bypass. Follow-up magnetic resonance imaging 1 month later showed enhanced tumor within the T2 hyperintense lesion. A total removal of the tumor through another craniotomy was performed. The pathologic diagnosis was metastatic carcinoma.
Conclusion:This is the first report of the metastatic carcinoma by seeding of tumor cells through STA-MCA bypass flow.
Keywords: Metastatic brain tumor, superficial temporal artery-middle cerebral artery anastomosis, N-isopropyl-p-[123I] iodoamphetamine single photon emission computed tomography
INTRODUCTION
Superficial temporal artery-middle cerebral artery (STA-MCA) anastomosis, is performed for symptomatic ischemic cerebrovascular disease with hemodynamic hypoperfusion. Although the clinical contribution of STA-MCA anastomosis is still controversial this operation has been widely performed, especially in Japan, for the purpose of increasing cerebral blood flow (CBF).[
CASE ILLUSTRATION
A 63-year-old man had undergone STA-MCA anastomosis for the treatment of left internal carotid artery (ICA) occlusion. He underwent annual follow-up magnetic resonance imaging (MRI) and single photon emission computed tomography (SPECT) after STA-MCA anastomosis.
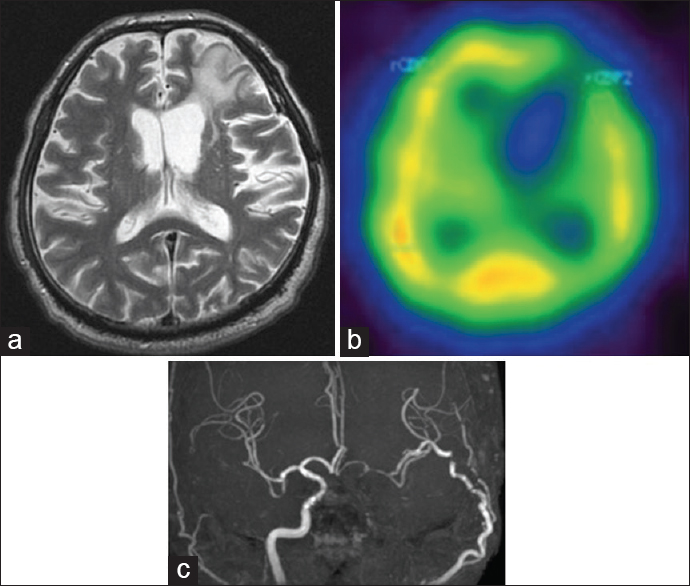
MRI performed at 4 years after the operation showed a newly-developed T2-hyperintense lesion in the perfusion territory of the bypass in the left frontal lobe [
Figure 1
(a) The initial T2-weighted magnetic resonance image showed a hyperintense area in the left frontal lobe. (b) N-isopropyl-p-[123I] iodoamphetamine single photon emission computed tomography revealed the lesion as a perfusion defect area (c) magnetic resonance angiography described patency of the bypass graft
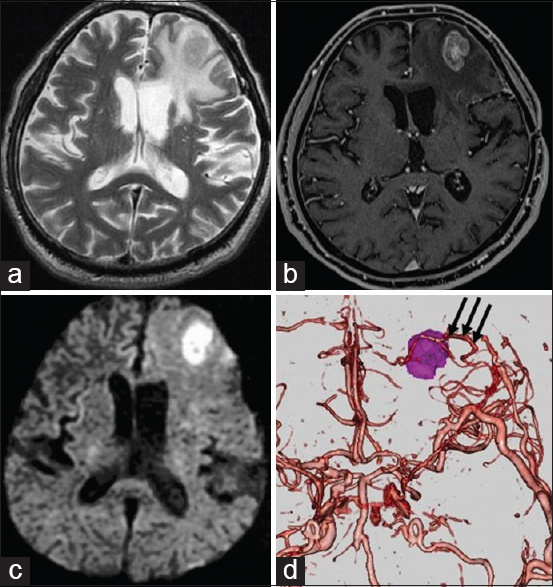
Figure 2
(a) The follow-up T2-weighted image demonstrated a newly-developed mass in the enlarged high intensity lesion of the left frontal lobe. (b) Gadolinium-enhanced magnetic resonance image showed an enhancement effect of the mass. (c) The lesion appeared hyperintense on diffusion-weighted image. (d) Three-dimensional computed tomography-angiography exhibited the bypass flow (arrow) perfusing around the lesion
DISCUSSION
STA-MCA anastomosis is performed for symptomatic ischemic cerebrovascular disease with hemodynamic hypoperfusion for the purpose of increasing CBF in the perfusion territory. As reported for various metastatic neoplasms within meningioma,[
In general, metastases occur preferentially at gray-white matter junctions and the vascular border zone (watershed) regions (62–64%), which are formed by the terminal capillary beds of cerebral arteries.[
In the present case, the metastatic tumor was initially misdiagnosed as brain infarction because of the clinical history of cerebral ischemic disease and their radiographic similarities, hyperintense on T2-weighted image, and cold spot on 123I-IMP SPECT. Finally, we obtained the accurate diagnosis through detection of radiographic changes on a follow-up MRI. 123I-IMP SPECT is widely used for measuring regional CBF in the diagnosis of cerebral ischemia.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Amin-Hanjani S, Butler WE, Ogilvy CS, Carter BS, Barker FG. Extracranial-intracranial bypass in the treatment of occlusive cerebrovascular disease and intracranial aneurysms in the United States between 1992 and 2001: A population-based study. J Neurosurg. 2005. 103: 794-804
2. Akiyama Y, Moritake K, Yamasaki T, Kimura Y, Kaneko A, Yamamoto Y. The diagnostic value of 123I-IMP SPECT in non-Hodgkin's lymphoma of the central nervous system. J Nucl Med. 2000. 41: 1777-83
3. . Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. The EC/IC Bypass Study Group. N Engl J Med. 1985. 313: 1191-200
4. Hayashida K, Nishimura T, Imakita S, Uehara T, Nakamura M, Tsuchiya T. Change of accumulation and filling pattern in evolution of cerebral infarction with I-123 IMP brain SPECT. Neuroradiology. 1991. 33: 9-14
5. Hwang TL, Close TP, Grego JM, Brannon WL, Gonzales F. Predilection of brain metastasis in gray and white matter junction and vascular border zones. Cancer. 1996. 77: 1551-5
6. Powers WJ, Clarke WR, Grubb RL, Videen TO, Adams HP, Derdeyn CP. COSS Investigators. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: The Carotid Occlusion Surgery Study randomized trial. JAMA. 2011. 306: 1983-92
7. Smith TW, Wang SY, Schoene WC. Malignant carcinoid tumor metastatic to a meningioma. Cancer. 1981. 47: 1872-7