- Department of Neurosurgery, Gold Coast University Hospital, Gold Coast, Queensland, Australia
Correspondence Address:
Dorian Pniel
Department of Neurosurgery, Gold Coast University Hospital, Gold Coast, Queensland, Australia
DOI:10.4103/sni.sni_75_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Dorian Pniel, Teresa K. Withers. A case of multiple nail gun injuries to the head and one to the heart. 01-Nov-2018;9:221
How to cite this URL: Dorian Pniel, Teresa K. Withers. A case of multiple nail gun injuries to the head and one to the heart. 01-Nov-2018;9:221. Available from: http://surgicalneurologyint.com/surgicalint-articles/9066/
Abstract
Background:Nail gun injuries, while uncommon, can present significant treatment challenges. Many are often caused by work-related accidents, they have also been seen in suicide attempts and assaults.
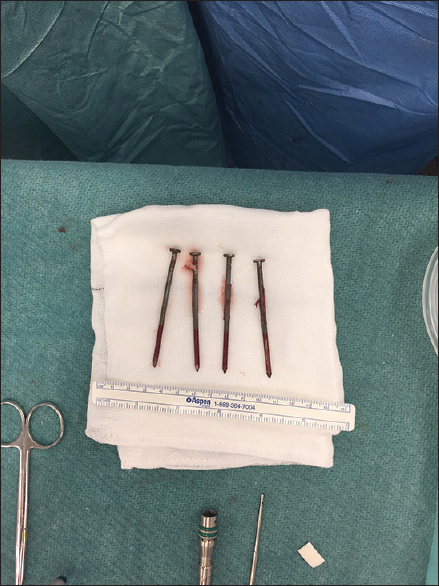
Case Description:A 53-year-old male was transferred from a peripheral hospital to a tertiary center after being found confused and with a left-sided weakness. Initial scans showed four nails penetrating the skull, with one additional nail in the pericardium. These all underwent surgical removal, and due to meticulous pre- and perioperative planning, the patient had a largely uneventful recovery.
Conclusion:The challenging nature of these injuries requires extensive workup prior to surgical decision-making in order to minimize potential complications.
Keywords: Angiography, nail gun, penetrating head injury
INTRODUCTION
Nail gun injuries to the head are being reported with increasing frequency. These injuries present a specific subset of challenges that exemplify the treatment of penetrating head injuries, and the importance of patient assessment as well as pre- and perioperative decision-making in order to achieve the best outcomes for patients. Due to the nature of nail gun injuries to the head, there are many known risks to patients, both in the acute phase as well as delayed complications. Careful planning and assessment is crucial in ensuring all eventualities are planned for, and that the possibility of unexpected issues is minimized. Our case illustrates the importance of multi-disciplinary care.
CASE HISTORY
A 53-year-old male was transferred to a peripheral hospital, initially confused with a glasgow coma score (GCS) of 14. He was moving all four limbs, but had 4/5 power of his left upper limb. He was noted to have a wound in the midline of his chest, three entry wounds right temporo-frontal, and one behind the right ear.
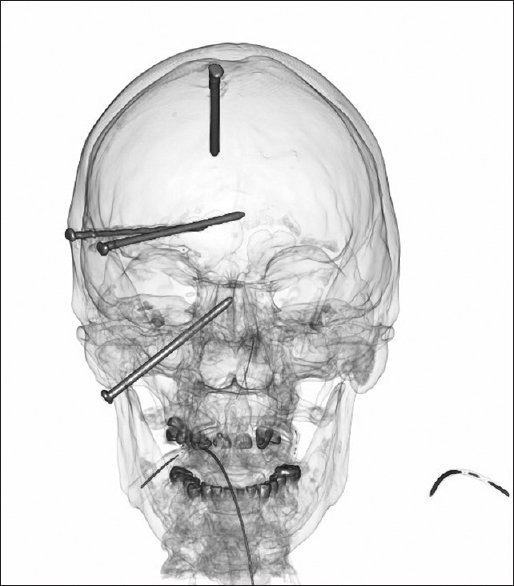
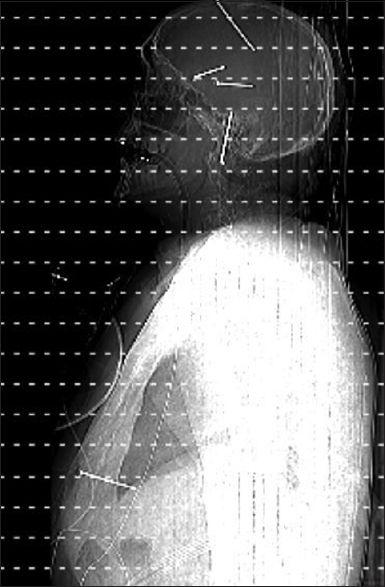
Imaging confirmed a nail through his pericardium, sitting beneath the left ventricle of his heart, with an associated hemopericardium. The scan also showed three nails in his right cerebral hemisphere, and a nail entering his brainstem through the right base of skull, with a small hematoma around the tip of the nail within the pons. He was hemodynamically stable [Figures
The patient was transferred to Gold Coast University Hospital. On arrival, he was taken to the operating theatre for removal of the pericardial nail. At operation, the nail had perforated the diaphragm, there was a pericardial hematoma, and the tip was seen to abut the heart causing superficial bruising. The nail was removed without incident, with the wound washed out and closed in layers over a pericardial drain [
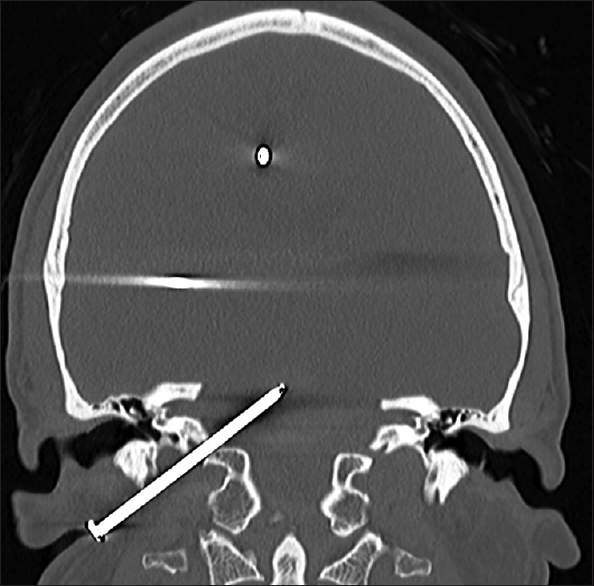
Subsequent computed tomography (CT) angiography showed an increase in the size of the pontine hematoma. The right middle cerebral artery appeared attenuated, and was thought to have an element of vasospasm, but otherwise the arterial vasculature was intact [
His sedation was lightened to assess his neurological status, which confirmed he could obey commands, spontaneously moved all four limbs, and had intact cranial nerves. The nail behind his right ear traversed his petrous temporal bone, it was unclear if it had penetrated the carotid artery or internal jugular vein [
Venography showed that the skull base nail had pierced the internal jugular vein. There was seen to be sufficient flow through the left transverse sinus to enable sacrifice of the right internal jugular vein if needed [
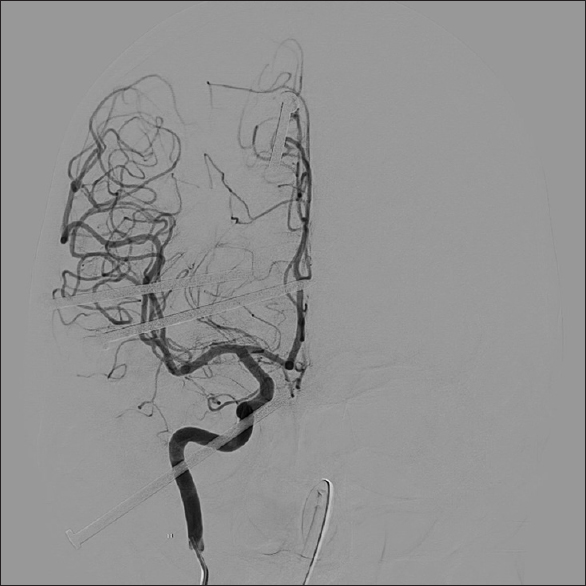
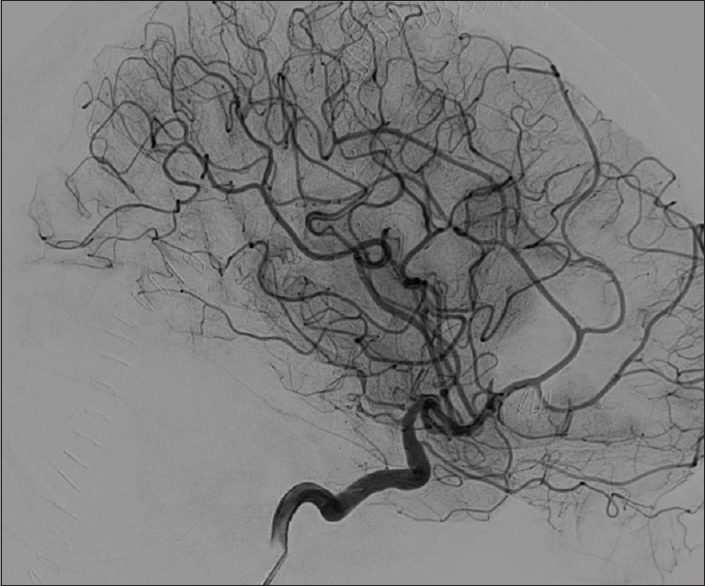
Angiography revealed that all four nails had entered the skull without causing any damage to the arterial vasculature. There was no pseudoaneurysm [
A consensus was reached to attempt balloon occlusion of the internal jugular vein prior to removal of the nails. The first two attempts were unsuccessful, as the rough surface of the nail punctured the balloons. The third attempt was successful, and a balloon was inflated in the right sigmoid sinus and left in-situ.
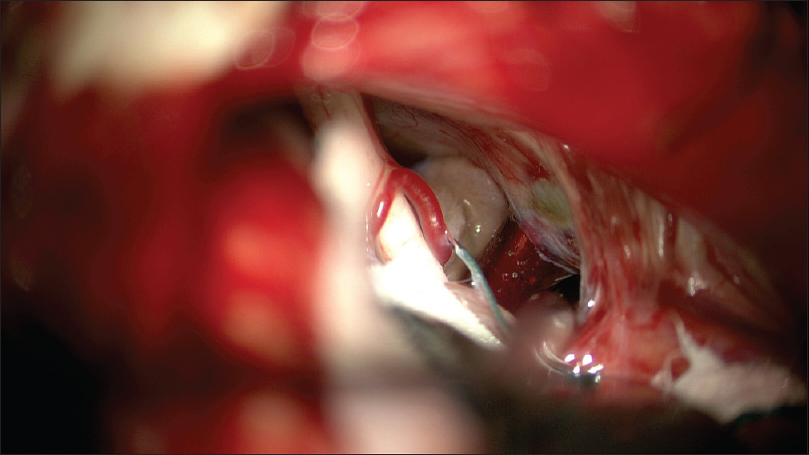
The skull base nail was to be removed first under direct visualization. Using a retrosigmoid approach, the nail was seen emerging into the cerebellar-pontine angle, missing the VIIth/VIIIth nerve complex, arteries, and then piercing the anterior brain stem [
The nail was extracted in a controlled manner by a second surgeon, under direct visualization. Removal required significant force, with some torsion. With the aid of direct observation, it was possible to confirm no new hemorrhage during extraction, and that vital structures could be protected. The defects in the brain stem and petrous temporal bone left by the nail were covered with floseal and surgicell. Standard closure was achieved.
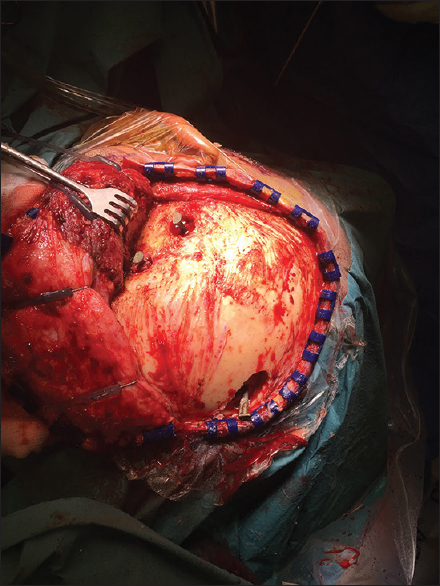
For the remaining nails, a trauma craniotomy flap was utilized in case urgent conversion to trauma craniotomy was required. A burr hole was drilled around the two temporal nails. Using gentle traction, the nails were removed. Gentle wash confirmed no hemorrhage or brain swelling. Lastly, the nail adjacent to the superior sagittal sinus was approached via a larger burr hole exposing the adjacent sinus, so packing of the sinus could be achieved if it had been breached. The nail was extracted with direct visualization. Bone cement was used for these defects, followed by standard closure [Figures
The patient underwent immediate postoperative angiography, which demonstrated no contrast extravasation once the balloon was deflated. A truncation defect was seen in the anterior branch of the right M2, and further imaging showed a small ischemic infarction nearby. There was no new hemorrhage. The patient was transferred back to intensive care [Figures
Postoperative recovery was uneventful and the only deficit documented was a subtle left hemiparesis. He was discharged to a rehabilitation unit.
DISCUSSION
The major pertinent points include the preoperative care and assessment, the pre- and postoperative imaging, the technical aspects of the patient's surgical management, and the decision-making regarding the order of procedures and treatment.
The literature surrounding the management of nail gun injuries to the head and chest is sparse, and consists largely of case reports. There are few case reports of nail gun injuries to multiple sites, predominantly the head and chest. A somewhat similar case was described in a case report from Japan published in 1995.[
On initial admission, the history surrounding the injury was unclear. As such, a full trauma CT was used to identify the potential injuries. On initial survey, the entry sites for the cranial nails were difficult to identify.
The first priority regarding treatment of the patient was managing the nail lodged within the pericardium. Given that the patient had sustained the injury an unknown period of time prior to presentation, it was felt that this nail posed the greatest immediate risk to life, and so had to be removed first. The increased size of the pontine hemorrhage post-cardiac surgery raised questions as to the patient's clinical state. As such, decisions regarding further management were withheld until the patient was reassessed following his cardiac surgery, in order to see if his situation was salvageable.
The location of the cranial nails was concerning for vascular injury. Cerebral digital subtraction angiography was utilized to assess the vascular anatomy prior to surgery. Without this approach, the injury to the patient's internal jugular vein could have been missed, and the odds of catastrophic bleeding intraoperatively would have been significantly higher and difficult to control. The temporal nails missed the major arteries of the sylvian fissure. The final nail abutted the sagittal sinus but injury could occur during extraction.
On postoperative imaging, there was a new truncation defect to the anterior M2 branch, but no extravasation of contrast. This was thought to be due to thrombosis.
A multi-site approach was utilized to remove the nail within the brain stem. The surgical team was able to achieve direct vision of the nail, and identify key structures. As the nail was removed, direct vision was maintained in order to assess for any hemorrhage and ensure the trajectory of removal was completely linear, without damaging the nearby structures. Due to the rough tip of the nails, damage could occur not only from penetration, but also upon removal, requiring thoughtful planning and gentle extraction.
A trauma flap was performed for removal of the other nails in order to allow expedient conversion to craniotomy if complications occurred. Due to careful hemostasis intraoperatively, the balloon occlusion of the internal jugular vein was able to be successfully removed postoperatively.
The general indications for surgery following a penetrating injury to the brain are: removal of foreign material; reduction in mass effect due to foreign material and/or hematoma; and debridement of unviable or infected tissue.[
CONCLUSION
Nail gun injuries to the brain, while uncommon, exemplify the treatment principles of penetrating injuries. Due to the nature of the injuries, a holistic and multi-disciplinary approach needs to be considered in order to minimize the risk of secondary injury. Specifically, use of appropriate imaging in the form of CT and digital subtraction angiography is crucial in ensuring appropriate surgical planning can be performed, and that vascular damage can be accounted for and controlled in order to reduce the risk of peri- and postoperative bleeding. As many of these injuries are low-velocity, patients may present lucid, with a normal GCS, as the damage can often be local only. While surgical debridement should be aimed to be minimal, use of direct vision in eloquent areas is important in reducing the risk of further damage, and careful planning is crucial in order to maintain patients' neurological states.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Anon . Surgical Management of Penetrating Brain Injury. J Trauma. 2001. p.
2. Bayston R, de Louvois J, Brown EM, Johnston RA, Lees P, Pople IK. Use of antibiotics in penetrating craniocerebral injuries.“Infection in Neurosurgery” Working Party of British Society for Antimicrobial Chemotherapy. Lancet. 2000. 355: 1813-7
3. Gordon DS. Surgery of violence. V. Missile wounds of the head and spine. Br Med J. 1975. 1: 614-6
4. Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock. 2011. 4: 395-402
5. Luo W, Liu H, Hao S, Zhang Y, Li J, Liu B. Penetrating brain injury caused by nail guns: Two case reports and a review of the literature. Brain Inj. 2012. 26: 1756-62
6. Rosenfeld JV. Gunshot injury to the head and spine. J Clin Neurosci. 2002. 9: 9-16
7. Sasaoka Y, Kamada K, Matumoto M, Ueda Y, Iwasaka T, Hukushima T. Penetrating injury of the head, neck and chest by a nail-gun: A case report. No Shinkei Geka. 1995. 23: 1099-104