- Department of Neurosurgery, Hoan My ITO Dong Nai Hospital, Bien Hoa, Vietnam
- Department of Neurosurgery, Vinmec Central Park International Hospital, Hochiminh, Vietnam
- Department of Radiology, Hoan My ITO Dong Nai Hospital, Bien Hoa, Vietnam.
Correspondence Address:
Tri Duc Duy Tran, Department of Neurosurgery, Hoan My ITO Dong Nai Hospital, Bien Hoa, Vietnam.
DOI:10.25259/SNI_398_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tri Duc Duy Tran1, Phong Duc Vo1, Tri Van Truong2, Thi Duc Ho3. A case of neurosurgical treatment of thoracic dorsal arachnoid web. 16-Jun-2023;14:210
How to cite this URL: Tri Duc Duy Tran1, Phong Duc Vo1, Tri Van Truong2, Thi Duc Ho3. A case of neurosurgical treatment of thoracic dorsal arachnoid web. 16-Jun-2023;14:210. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12362
Abstract
Background: Dorsal arachnoid webs constitute abnormal formations of arachnoid that tend to occur in the upper thoracic spine and can lead to spinal cord displacement. Patients typically present with back pain, sensory disturbances, and weakness. It may also obstruct the cerebrospinal fluid (CSF) flow, leading to syringomyelia. In magnetic resonance (MR) studies, the “scalpel sign” is a classical finding, and it may also be accompanied by syringomyelia attributed to CSF flow. Definitive surgical resection is the mainstay of treatment.
Case Description: A 31-year-old male presented with mild weakness in the right leg and diffuse lower extremity sensory changes. The MR showed the typical “scalpel sign” at the T7 level consistent with diagnosing a spinal arachnoid web. He underwent a T6-T8 laminotomy for lysis of the web and decompression of the thoracic cord. Postoperatively, his symptoms improved markedly.
Conclusion: Surgical resection is the treatment of choice when an arachnoid web is documented on an MR and correlates with the patient’s clinical symptoms/signs.
Keywords: Laminotomy, Scalpel sign, Spinal arachnoid web, Syringomyelia, Thoracic dorsal arachnoid web
INTRODUCTION
The dorsal arachnoid web (DAW) is an abnormal thickening of arachnoid bands that cross the dorsal spinal cord.[
CASE REPORT
History and examination
A 31-year-old male patient began to experience numbness in his right leg in 2014. In 2016, it became somewhat atrophied, and by 2021, the patient was increasingly/persistently numb. On examination, he had a right leg with 4/5 motor strength and 3+ deep tendon reflexes at the Patellar and Achilles levels.
Imaging
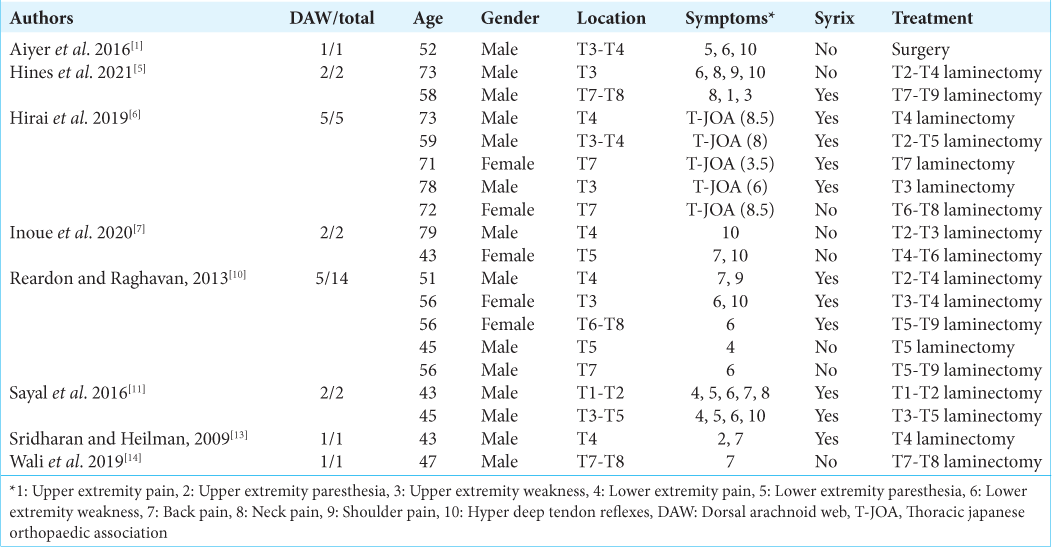
He underwent a thoracic magnetic resonance imaging (MRI) without contrast that showed spinal cord compression at the T7 level (i.e., cord displaced to the left on the axial images) due to a DAW. On the T2-weighted sagittal image, there was a sharp dorsal indentation of the spinal cord consistent with the positive “scalpel sign” [
Surgery
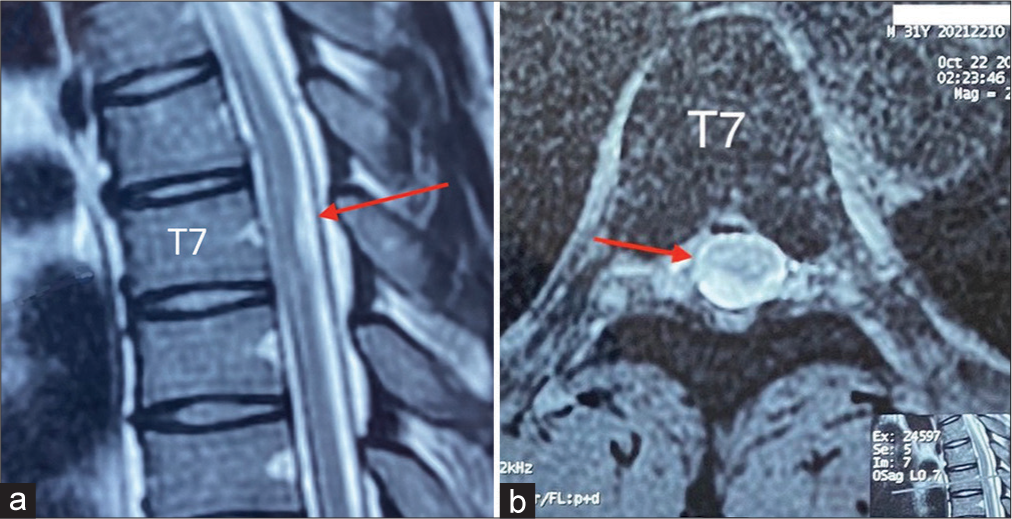
The patient underwent a T6-T8 laminectomy with preservation of the joints to avoid instability. The dura was exposed in the midline, and the arachnoid web (AW) was immediately visualized [
Postoperative course
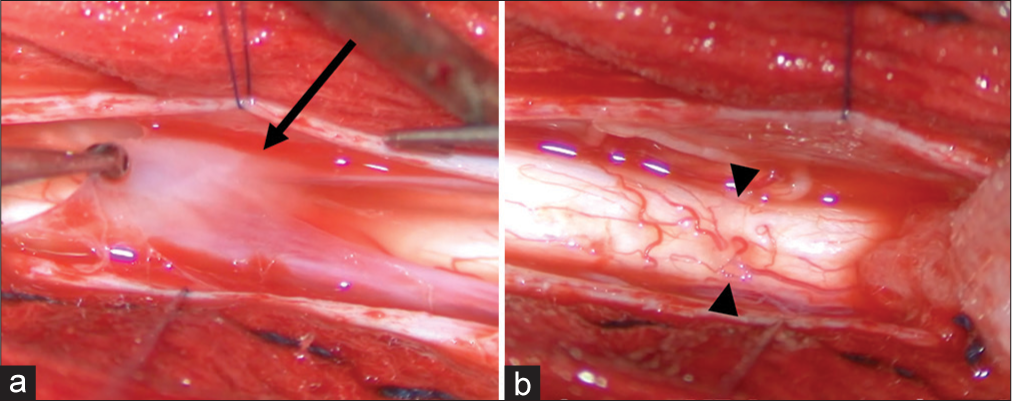
Postoperatively, the numbness in the right leg decreased significantly, and the right leg muscle strength also improved gradually. About 10 days after surgery, the incision healed well, and the patient walked with 5/5 muscle strength. The patient returned to work after 1 month. MRI 6 months after surgery showed that the scalpel sign had disappeared, and the spinal cord was no longer deviated [
DISCUSSION
Clinical presentations
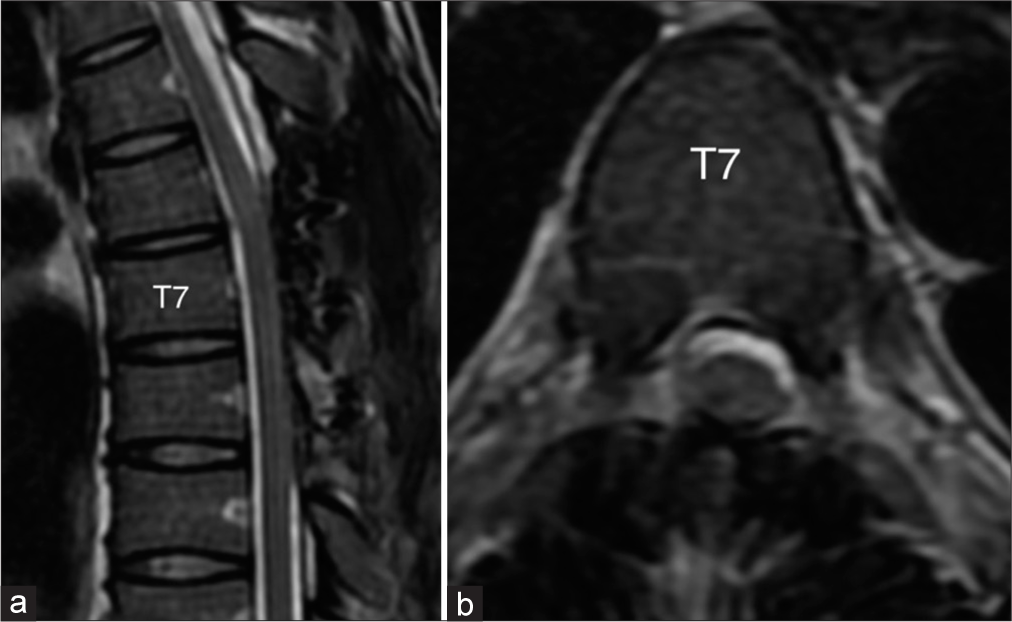
Patients with DAW typically present with: neurogenic back pain associated with myelopathy and/or radiculopathy, and potentially urinary incontinence. The physical examination frequently shows: motor deficits, hyperreflexia, sensory deficits, and cerebellar dysfunction.[
Pathophysiology
The mechanisms of AW formation remain unknown.[
Histology
According to Chang et al.,[
DAW location and syrinx formation
The DAW webs are usually dorsal to the spinal cord in the thoracic region and occasionally occur with accompanying syrinx formation.[
MR findings of DAW
MRI is the primary tool for diagnosing DAWs. However, it is not very sensitive due to the relatively thin size of the web compared to adjacent tissue.
Features of DAW on MR include a thick fibrous band of arachnoid tissue in a dorsal and extramedullary location accompanied by focal dorsal cord compression that yields the positive “scalpel sign”, pathognomonic for DAW.[
CINE — cardiac-gated phase-contrast cine-mode MR
The CINE MR may locate SAW and illustrate one-way CSF flow attributed to DAW.[
Myelogram findings of DAW
The utility of the computed tomography myelogram is based on the theory that DAW partially obstructs CSF outflow. However, the DAW may also be missed in these studies.
Time to diagnosis and treatment
Nisson et al.[
Outcomes of DAW
Several articles report on the effectiveness of surgery for DAW patients.[
CONCLUSION
The SAW is a rare disease characterized on MRI by the positive “scalpel sign.” For patients with significant myelopathy, operative decompression of the DAW is warranted.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aiyer R, El-Sherif Y, Voutsinas L. Dorsal thoracic arachnoid web presenting as neuropathic pain: ‘Scalpel’ sign found on MRI. Neuroradiol J. 2016. 29: 393-5
2. Ben Ali H, Hamilton P, Zygmunt S, Yakoub KM. Spinal arachnoid web-a review article. J Spine Surg. 2018. 4: 446-50
3. Chang HS, Nagai A, Oya S, Matsui T. Dorsal spinal arachnoid web diagnosed with the quantitative measurement of cerebrospinal fluid flow on magnetic resonance imaging. J Neurosurg Spine. 2014. 20: 227-33
4. Grewal SS, Pirris SM, Vibhute PG, Gupta V. Identification of arachnoid web with a relatively novel magnetic resonance imaging technique. Spine J. 2015. 15: 554-5
5. Hines T, Wang C, Duttlinger C, Thompson J, Watford K, Motley B. Thoracic dorsal arachnoid web with rapid onset of symptoms: A report of two cases and brief review of the literature. Surg Neurol Int. 2021. 12: 323
6. Hirai T, Taniyama T, Yoshii T, Mizuno K, Okamoto M, Inose H. Clinical outcomes of surgical treatment for arachnoid web: A case series. Spine Surg Relat Res. 2019. 3: 43-8
7. Inoue J, Miyakoshi N, Hongo M, Kobayashi T, Abe T, Kikuchi K. Diagnosis and surgical treatment of thoracic dorsal arachnoid web: A report of two cases. Case Rep Orthop. 2020. 2020: 8816598
8. Nada A, Mahdi E, Mahmoud E, Cousins J, Ahsan H, LeivaSalinas C. Multi-modality imaging evaluation of the dorsal arachnoid web. Neuroradiol J. 2020. 33: 508-16
9. Nisson PL, Hussain I, Härtl R, Kim S, Baaj AA. Arachnoid web of the spine: A systematic literature review. J Neurosurg Spine. 2019. 31: 175-84
10. Reardon MA, Raghavan P, Carpenter-Bailey K, Mukherjee S, Smith JS, Matsumoto JA. Dorsal thoracic arachnoid web and the “scalpel sign”: A distinct clinical-radiologic entity. AJNR Am J Neuroradiol. 2013. 34: 1104-10
11. Sayal PP, Zafar A, Carroll TA. Syringomyelia secondary to “occult” dorsal arachnoid webs: Report of two cases with review of literature. J Craniovertebr Junction Spine. 2016. 7: 101-4
12. Schultz R, Steven A, Wessell A, Fischbein N, Sansur CA, Gandhi D. Differentiation of idiopathic spinal cord herniation from dorsal arachnoid webs on MRI and CT myelography. J Neurosurg Spine. 2017. 26: 754-9
13. Sridharan A, Heilman CB. Transverse dorsal arachnoid web and syringomyelia: Case report. Neurosurgery. 2009. 65: E216-7 discussion E217
14. Wali AR, Birk HS, Martin J, Santiago-Dieppa DR, Ciacci J. Neurosurgical management of a thoracic dorsal arachnoid web: Case illustration. Cureus. 2019. 11: e4945