- Department of Neurosurgery, Shiraz University of Medical Sciences, Shiraz, Iran
- Department of Pathology, Shiraz University of Medical Sciences, Shiraz, Iran
- Department of Hematology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran.
Correspondence Address:
Majid Reza Farrokhi, Department of Neurosurgery, Shiraz University of Medical Sciences, Shiraz, Iran.
DOI:10.25259/SNI_332_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Seyed Reza Mousavi1, Sahand Mohammadzadeh2, Alireza Rezvani3, Hoseinali Khalili1, Mavlonov Jaloliddin Begijonovich1, Mohammadhadi Amirshahpari Motlagh1, Majid Reza Farrokhi1. A case report: Bilateral reconstruction of C2 lateral masses with expandable titanium cages following axis (C2) solitary plasmacytoma resection with 2-year follow-up. 23-Jun-2023;14:217
How to cite this URL: Seyed Reza Mousavi1, Sahand Mohammadzadeh2, Alireza Rezvani3, Hoseinali Khalili1, Mavlonov Jaloliddin Begijonovich1, Mohammadhadi Amirshahpari Motlagh1, Majid Reza Farrokhi1. A case report: Bilateral reconstruction of C2 lateral masses with expandable titanium cages following axis (C2) solitary plasmacytoma resection with 2-year follow-up. 23-Jun-2023;14:217. Available from: https://surgicalneurologyint.com/surgicalint-articles/12375/
Abstract
Background: Solitary plasmacytoma (SP) caused the collapse/destruction of the C2 vertebral body in a 78-year-old male. To provide sufficient posterior stabilization, the patient warranted lateral mass fusion to supplement the bilateral pedicle/screw rod instrumentation.
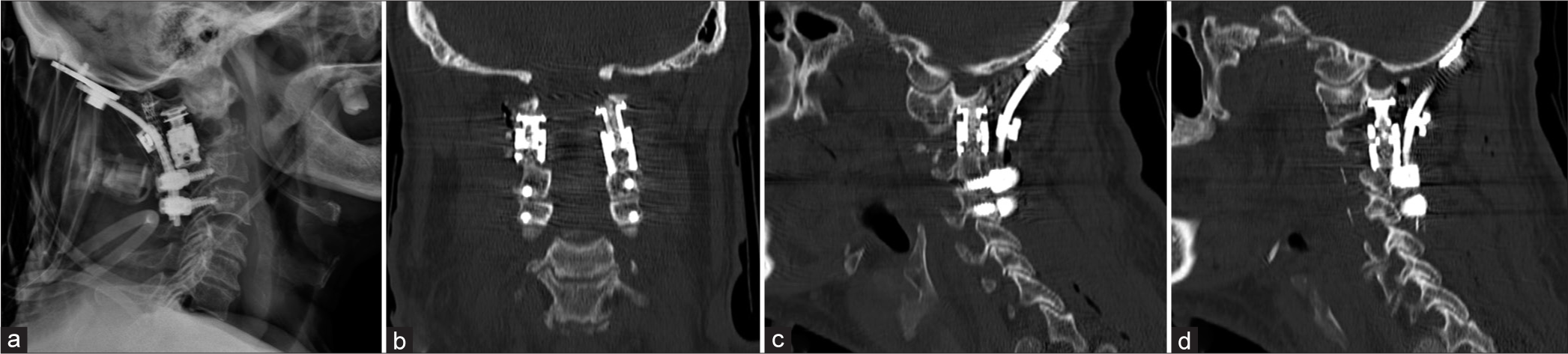
Case Description: A 78-year-old male presented with neck pain alone. X-rays, computed tomography, and magnetic resonance studies documented C2 vertebral collapse with the complete destruction of both lateral masses. The surgery required a laminectomy (i.e., bilateral lateral mass resection), plus placement of bilateral expandable titanium cages from C1 to C3 to supplement the screw/rod occipitocervical (O-C4) fixation. Adjuvant chemotherapy and radiotherapy were also administered. Two years later, the patient remained neurologically intact and radiographically had no evidence of tumor recurrence.
Conclusion: In patients with vertebral plasmacytomas and bilateral lateral mass destruction, posterior occipital-cervical C4 rod/screw fusions may warrant the additional bilateral placement of titanium expandable lateral mass cages from C1 to C3.
Keywords: Case report, Lateral mass, Solitary plasmacytoma, Spinal reconstruction, Titanium expandable cage
INTRODUCTION
Novel approaches are available for lateral mass reconstruction following vertebral destruction attributed to a tumor, trauma, or iatrogenic injuries.[
PRESENTATION OF CASE
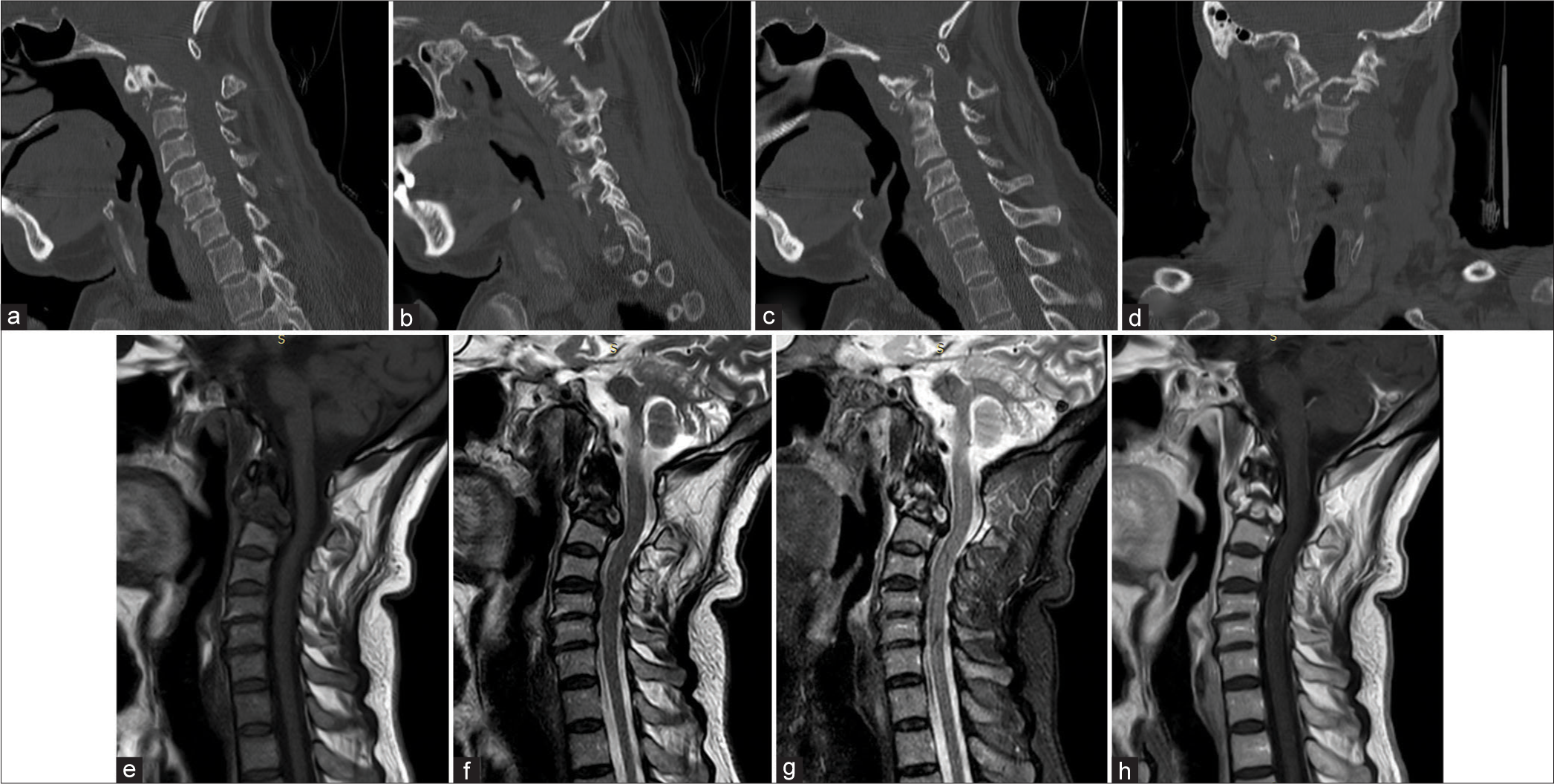
A 78-year-old male presented with 2 months of neck pain and a positive left-sided Hoffman’s sign. The computed tomography (CT) showed a single lytic C2 hypodense bone lesion. On the magnetic resonance (MR), the lesion was markedly enhanced with gadolinium. The angiogram showed the vertebral artery (VA) was encased bilaterally at the C2 level [
Adjuvant therapies and 2-year follow-up
Adjuvant therapies were included in the study: a bone marrow aspiration/biopsy, total spine diffusion-weighted MR imaging, immunoelectrophoresis, and free kappa and lambda light chain assessment. As the free kappa assay showed an increase without other systemic involvement, a course of radiation therapy (RT) (without systemic treatment) was administered following which the free kappa assay normalized. Notably, thrombocytosis occurred despite local tumor control, and a JAK2 mutation was documented. The patient, who was 78-years-old (i.e., above age 65), was therefore additionally placed on both hydroxyurea and aspirin to avoid hypercoagulation. Two years later, the patient was asymptomatic, the cervical construct remained stable, and platelet levels were normal [
Figure 4:
Follow-up X-rays after 2 months (a: Anteroposterior, b: Lateral). 6-month postoperative magnetic resonance imaging showed no compression on the dural sac in the (c) Short tau inversion recovery and (d) T2-weighted sequences. Computed tomography scan 2-year postoperation (e: Right, f: Left parasagittal, and g: Coronal).
DISCUSSION
As pathology of the lateral masses of C1-C2 can be destabilizing, special attention has recently been given to the reconstruction of the lateral masses/facet joints at this level.[
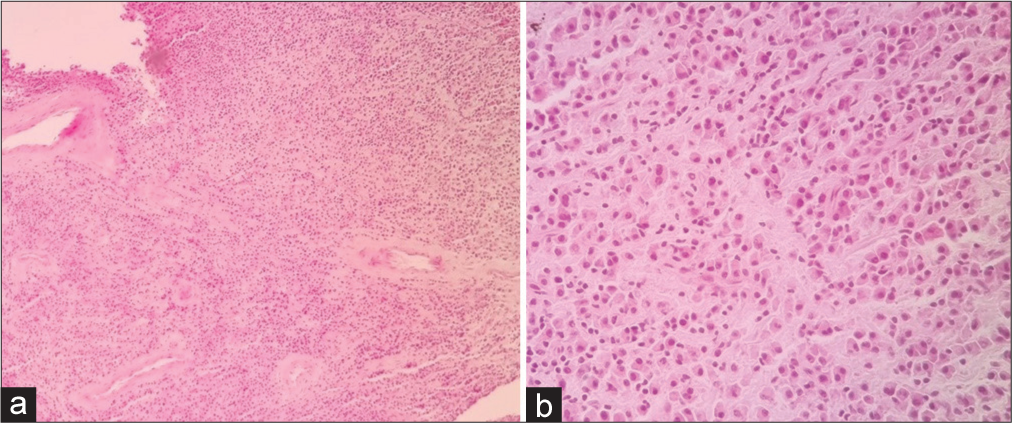
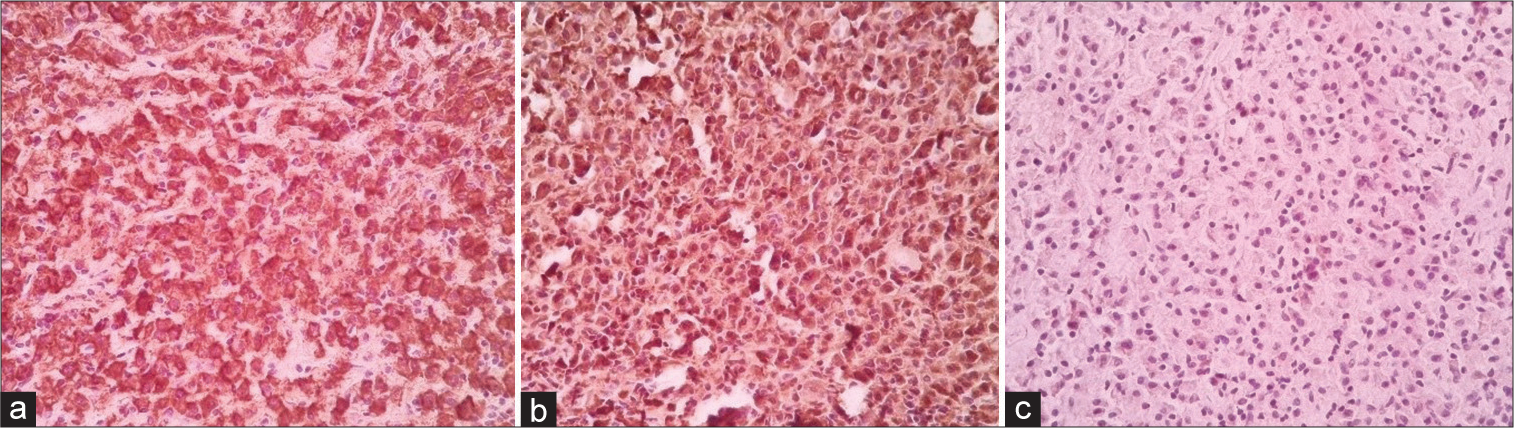
Pathology/histology; Final diagnosis kappa monocytic plasmacytoma
Our final histological diagnosis was Kappa monocytic plasmacytoma. The histology revealed sheets of neoplastic cells composed predominantly of plasma cells, the majority of which showed abundant eosinophilic cytoplasm, eccentrically placed nuclei, mild nuclear atypia, and binucleation [
CONCLUSION
A 78-year-old male’s X-rays, CT, and MR documented C2 vertebral collapse with the complete destruction of both lateral masses due to a biopsy-proven plasmacytoma. He was successfully managed with a C2 laminectomy/ partial vertebrectomy, C1-C3 bilateral lateral mass/cage reconstruction, and occipital-C4 screw/rod fusion along with adjuvant radiation/chemotherapies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chung JY, Do Kim J, Park GH, Jung ST, Lee KB. Occipitocervical reconstruction through direct lateral and posterior approach for the treatment of primary osteosarcoma in the atlas: A case report. Spine. 2012. 37: E126-32
2. Clarke MJ, Zadnik PL, Groves ML, Sciubba DM, Witham TF, Bydon A. Fusion following lateral mass reconstruction in the cervical spine. J Neurosurg Spine. 2015. 22: 139-50
3. Jian Q, Liu Z, Duan W, Guan J, Jian F, Chen Z. Reconstruction of the cervical lateral mass using 3-dimensional-printed prostheses. Neurospine. 2022. 19: 202-11
4. Jian Q, Liu Z, Duan W, Jian F, Bo X, Chen Z. Biomechanical evaluation of subaxial lateral mass prothesis: A finite element analysis study. Comput Methods Biomech Biomed Eng. 2022. 25: 1870-8
5. Jian Q, Liu Z, Duan W, Jian F, Chen Z. Subaxial lateral mass prosthesis for posterior reconstruction of cervical spine. J Neurol Surg A Cent Eur Neurosurg. 2022. p.
6. Mousavi R, Farrokhi MR, Eghbal K, Safaee J, Dehghanian AR. Reconstruction of C1 lateral mass with an expandable cage in addition to vertebral artery preservation: Presenting two cases. Br J Neurosurg. 2021. p. 1-6
7. Ohana N, Rouvio O, Nalbandyan K, Sheinis D, Benharroch D. Classification of solitary plasmacytoma, is it more intricate than presently suggested? A commentary. J Cancer. 2018. 9: 3894-7
8. Peciu-Florianu I, Viswanathan GC, Barges-Coll J, Castillo-Velázquez GA, Zambelli PY, Duff JM. Bilateral C-1 lateral mass reconstruction following radical resection of a giant osteoblastoma of the atlas: Case report. J Neurosurg Spine. 2017. 26: 307-12
9. Pham A, Mahindra A. Solitary plasmacytoma: A review of diagnosis and management. Curr Hematol Malig Rep. 2019. 14: 63-9
10. Stephens BH, Wright NM. Reconstruction of the C-1 lateral mass with a titanium expandable cage after resection of eosinophilic granuloma in an adult patient. J Neurosurg Spine. 2017. 26: 252-6