- Department of Neurosurgery, King Abdullah Medical City, Makkah, Saudi Arabia
- Department of Radiology, King Abdullah Medical City, Makkah, Saudi Arabia
- Department of Medical Laboratory Administration/Microbiology Parasitology, King Abdullah Medical City, Makkah, Saudi Arabia
- Department of Infectious Disease, King Abdullah Medical City, Makkah, Saudi Arabia
- Department of Pathology, Umm Al-Qura University, Makkah, Saudi Arabia.
Correspondence Address:
Ahmed Adel Farag,Department of Neurosurgery, King Abdullah Medical City, Makkah, Saudi Arabia.
DOI:10.25259/SNI_70_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mubasher Ahmed1, Abdulaziz A. Basurrah1, Zaina Siraj Brinji2, Naseem Albargi2, Mona Abd EL-Fattah3, Omar Alnashiwaaty4, Mona Shadad Aljohani4, Alaa Alkhotani5, Ahmed Adel Farag1. A case report of an unusual cerebral hydatid cyst. 22-Mar-2024;15:99
How to cite this URL: Mubasher Ahmed1, Abdulaziz A. Basurrah1, Zaina Siraj Brinji2, Naseem Albargi2, Mona Abd EL-Fattah3, Omar Alnashiwaaty4, Mona Shadad Aljohani4, Alaa Alkhotani5, Ahmed Adel Farag1. A case report of an unusual cerebral hydatid cyst. 22-Mar-2024;15:99. Available from: https://surgicalneurologyint.com/surgicalint-articles/12814/
Abstract
Background: Intracranial hydatid cyst is an exceedingly uncommon condition. Typically, it manifests as hydatid cysts in the liver, lungs, kidney, and spleen. In this report, we present a rare case of a hydatid cyst located in the brain, exhibiting atypical radiological characteristics, and successfully treated with complete microsurgical excision.
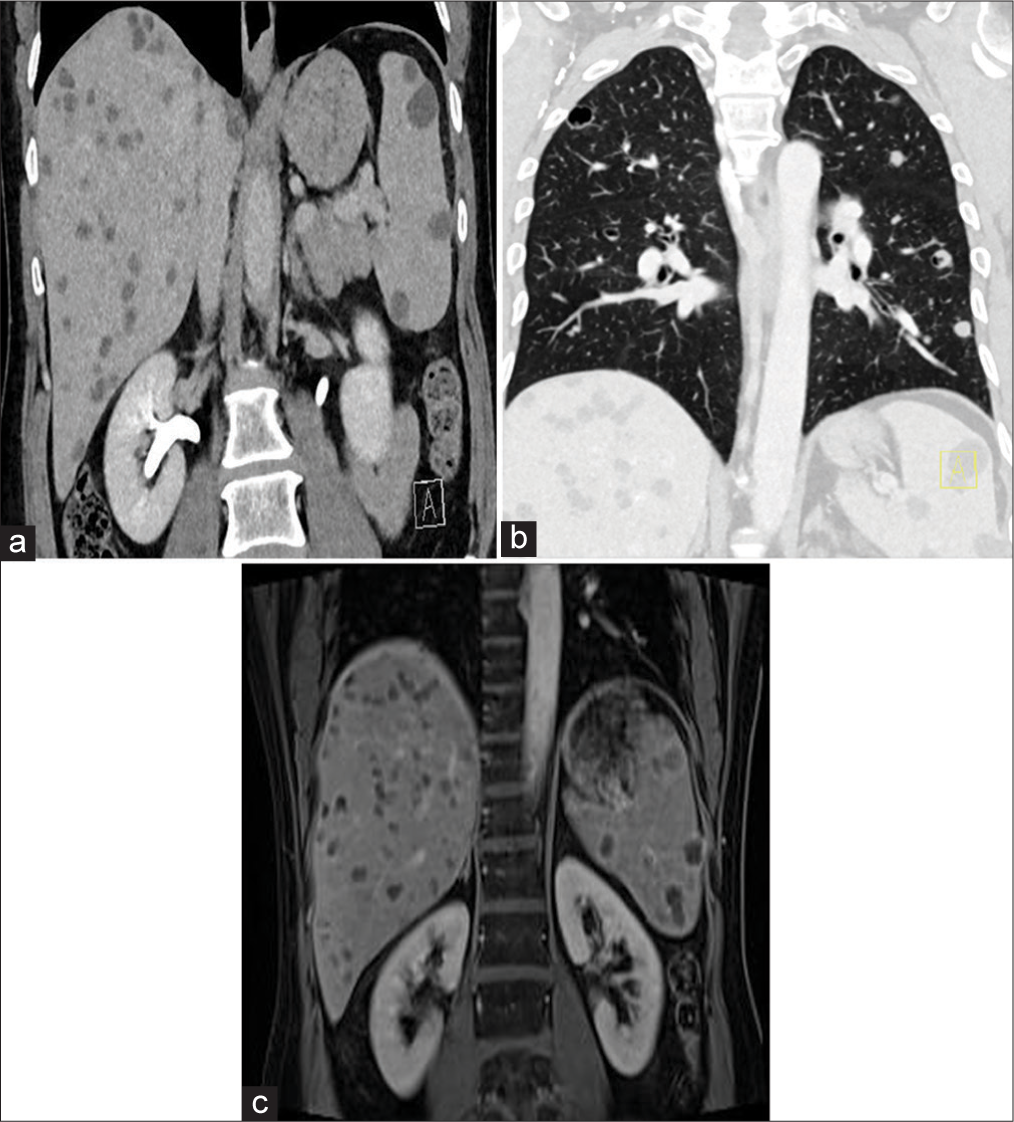
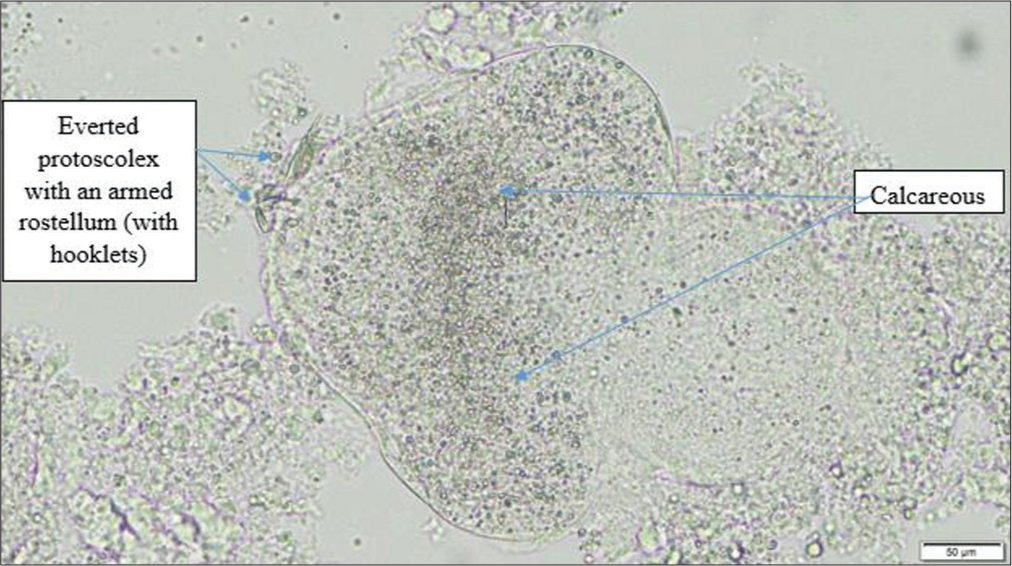
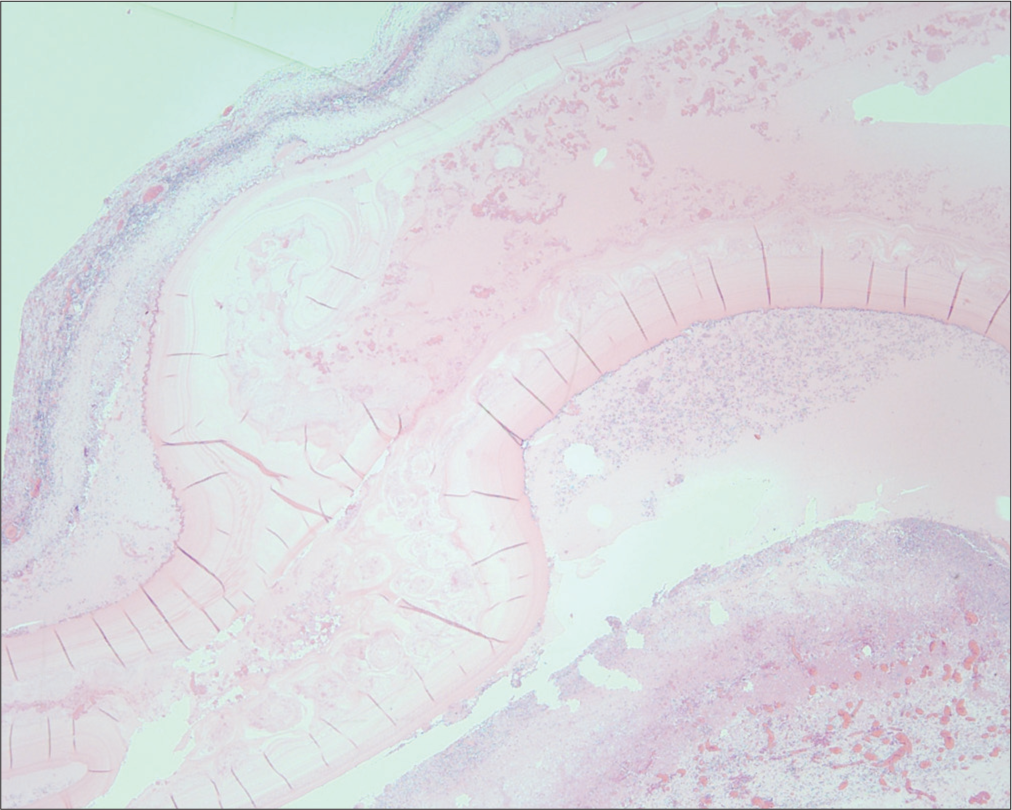
Case Description: A 45-year-old male, a former smoker, presented with a new-onset seizure. Brain imaging revealed a solitary, intra-axial, and cystic lesion with wall enhancement in the right temporal region. The cyst extended into the temporal horn of the right lateral ventricle, surrounded by mild edema. Differential diagnoses included brain metastasis, abscess, and tuberculoma. However, following computed tomography (CT) scans of the chest, abdomen, and pelvis (CAP) and serological tests, the provisional diagnosis included a hydatid cyst. The CT CAP showed diffuse non-specific cystic lesions of variable sizes in the liver and spleen, along with numerous bilateral pulmonary cysts. A right temporal craniotomy was performed, and the cyst was microsurgically excised without rupture. Microscopic and histopathological examination confirmed the presence of a hydatid cyst.
Conclusion: Intracranial hydatid cyst is an extremely rare condition and should always be considered a possible differential diagnosis in cases of cerebral cystic lesions. Hydrodissection is the preferred surgical method for resection; however, in atypical cases such as the one described here, meticulous dissection of the cyst capsule from the brain parenchyma may be successful with minimal risk of intraoperative rupture.
Keywords: Brain hydatid cyst, Case report, Dowling technique, Echinococcus granulosus
INTRODUCTION
The incidence of intracranial hydatid disease represents 1–2% of all reported cases of hydatid disease.[
CASE DESCRIPTION
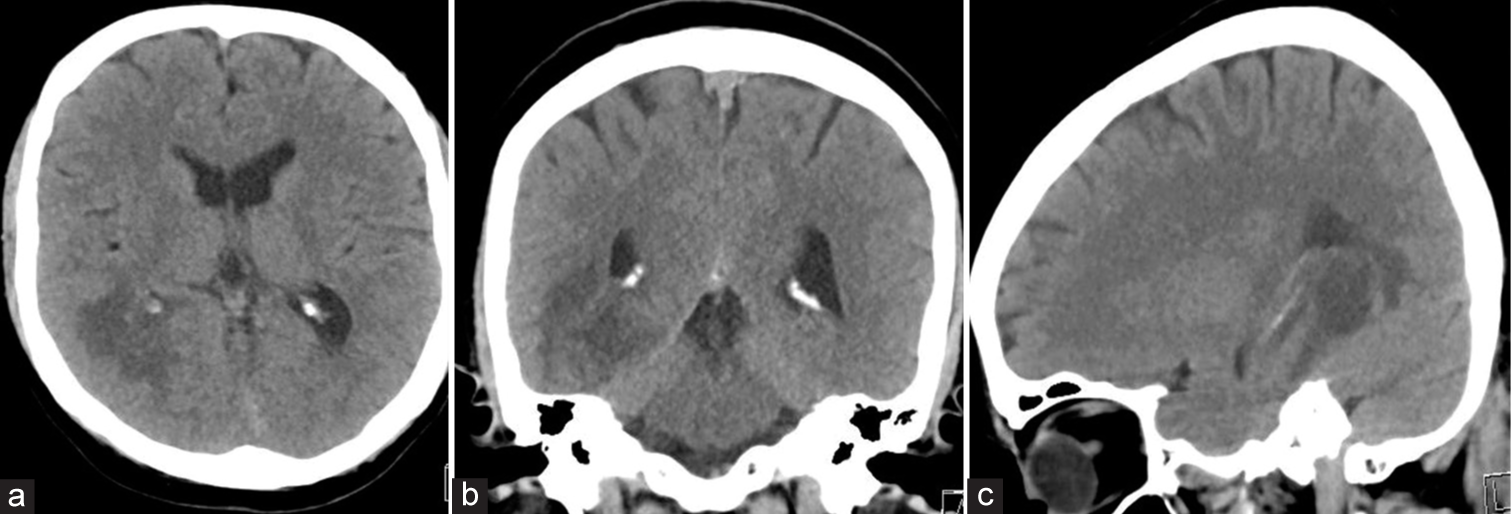
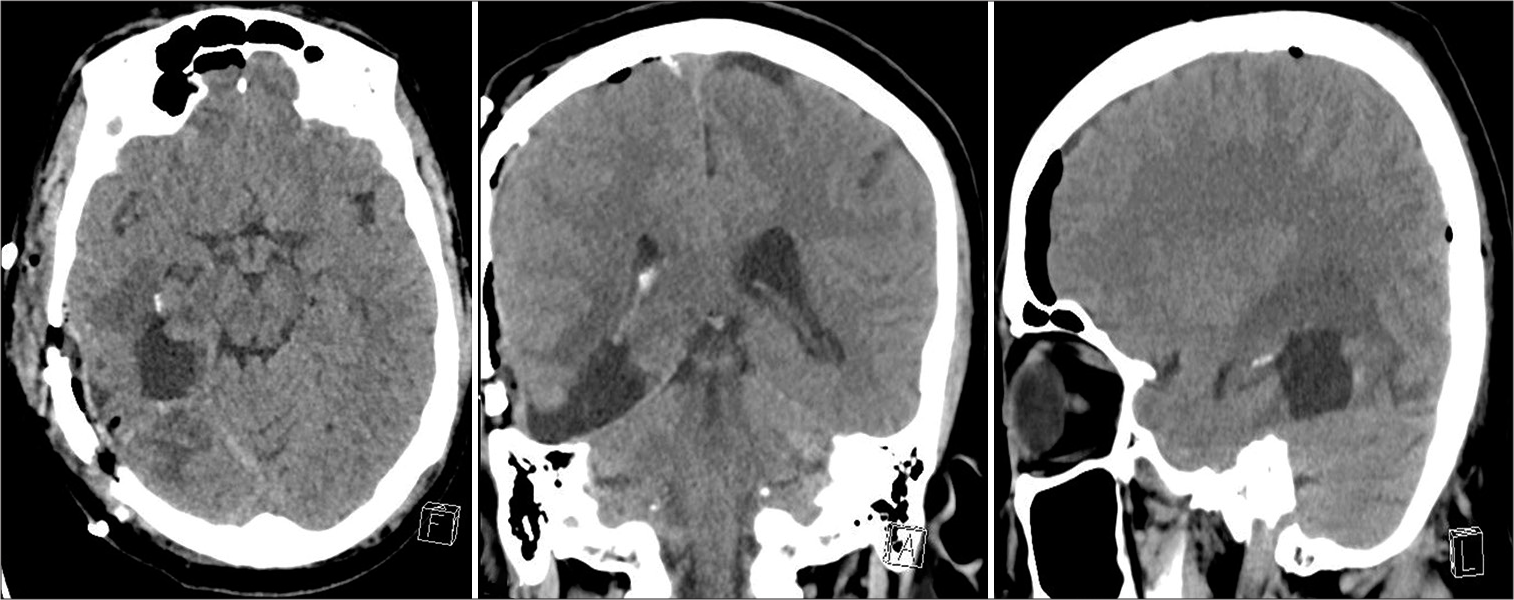
We present the case of a 45-year-old male with an Egyptian background and a history of smoking who was referred from another hospital due to headache, dizziness, and blurred vision. Brain imaging revealed a solitary cystic lesion in the right temporal region, extending into the temporal horn of the right lateral ventricle and surrounded by mild edema [
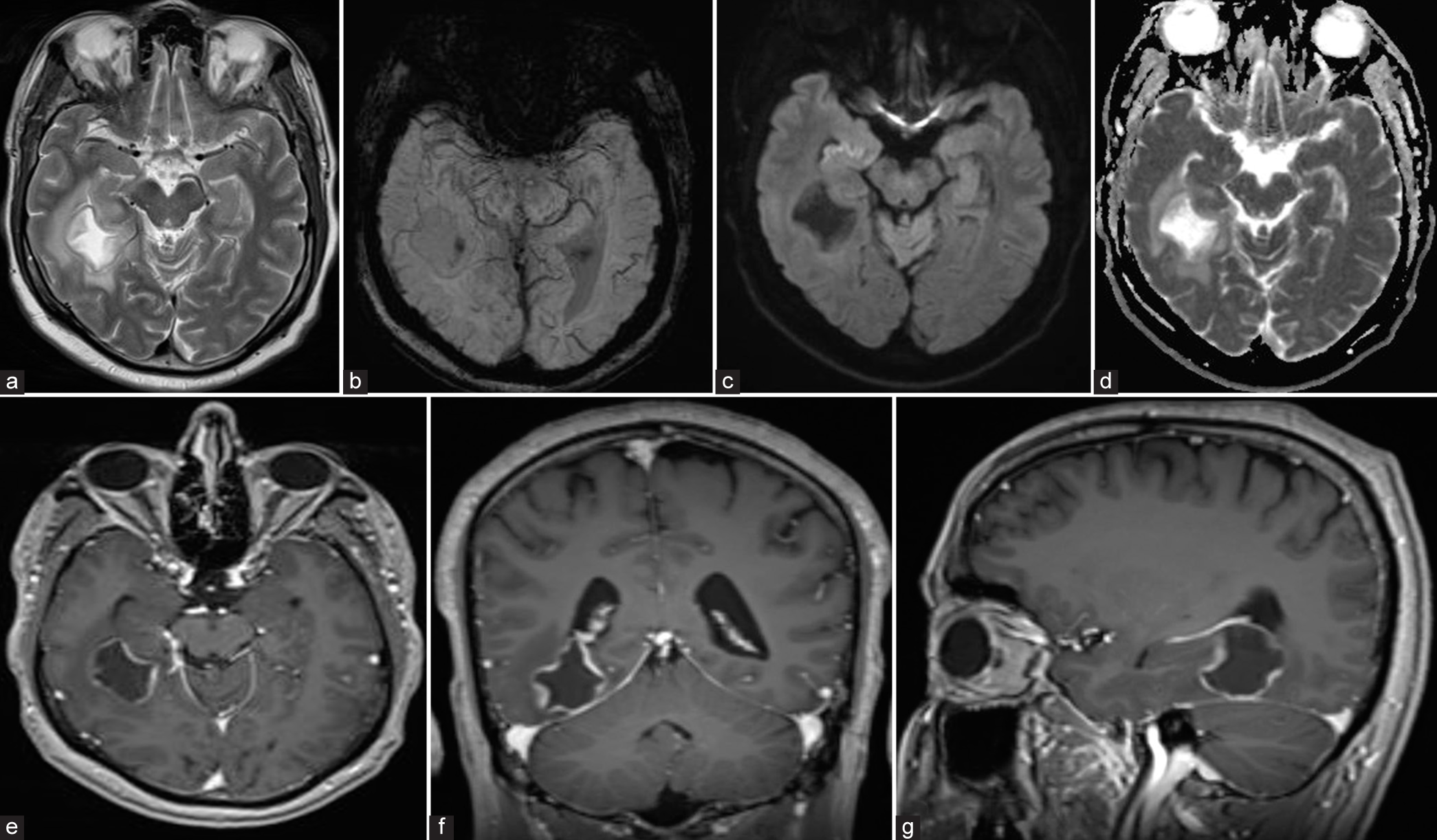
Figure 2:
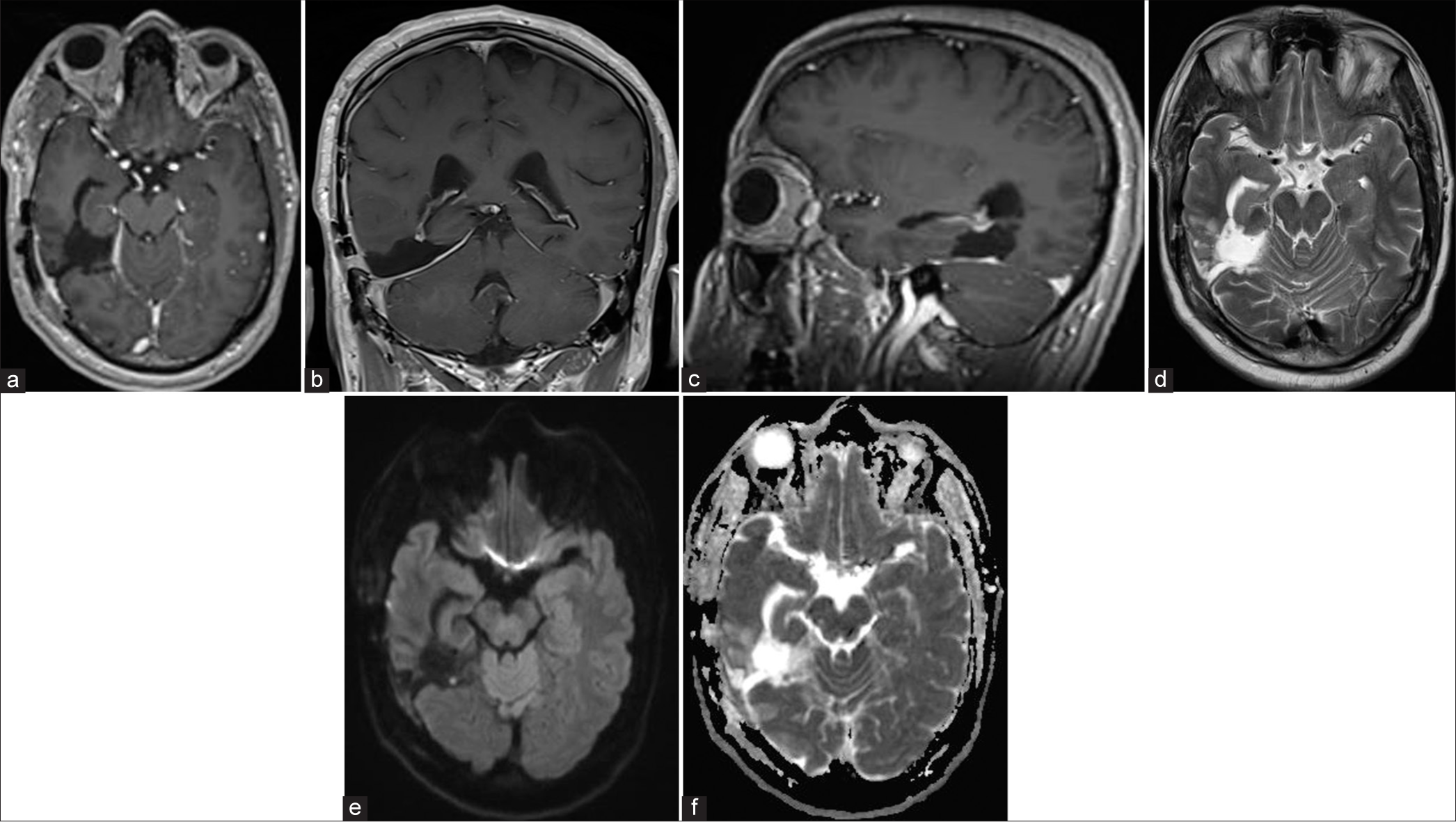
Magnetic resonance imaging brain (a) axial T2, (b) gradient echo, (c) diffusion-weighted imaging, (d) apparent diffusion co-efficient, (e) axial T1 postcontrast, (f) coronal T1 postcontrast, and (g) sagittal T1 postcontrast images showed an intra-axial cystic lesion in the right posterior temporal lobe with enhanced smooth undulating margins and marked surrounding vasogenic edema causing compressive mass effect on the temporal horn of right lateral ventricle, demonstrate high T2/fluid-attenuated inversion recovery, iso on T1 with peripheral wall enhancement, however, no significant restricted diffusion or blooming artifacts, approximately measuring 3.4 × 2.6 cm in anterior-posterior and transverse (AP and Ts) diameters. The rest of the brain parenchyma shows normal signal intensity with preserved gray-white matter differentiation.
Figure 8:
A follow-up magnetic resonance imaging brain done after 3 months (a) axial T1 postcontrast, (b) coronal T1 postcontrast, (c) sagittal T1 postcontrast, (d) axial T2, (e) Diffusion-weighted imaging, and (f) apparent diffusion co-efficient showed complete resection of the lesion with no evidence of recurrence.
DISCUSSION
Intracranial hydatid cysts can be classified as primary or secondary.[
Magnetic resonance (MR) and CT scans of the brain characteristically show a spherical, well-defined, and non-enhancing cystic lesion without peripheral edema.[
Surprisingly, the radiological finding of our case was atypical; it showed cystic wall enhancement and perilesional edema, which is unusual for a brain hydatid cyst. Moreover, it was reported as a ruptured hydatid cyst leading to an inflammatory reaction of the surrounding brain tissue, causing edema.
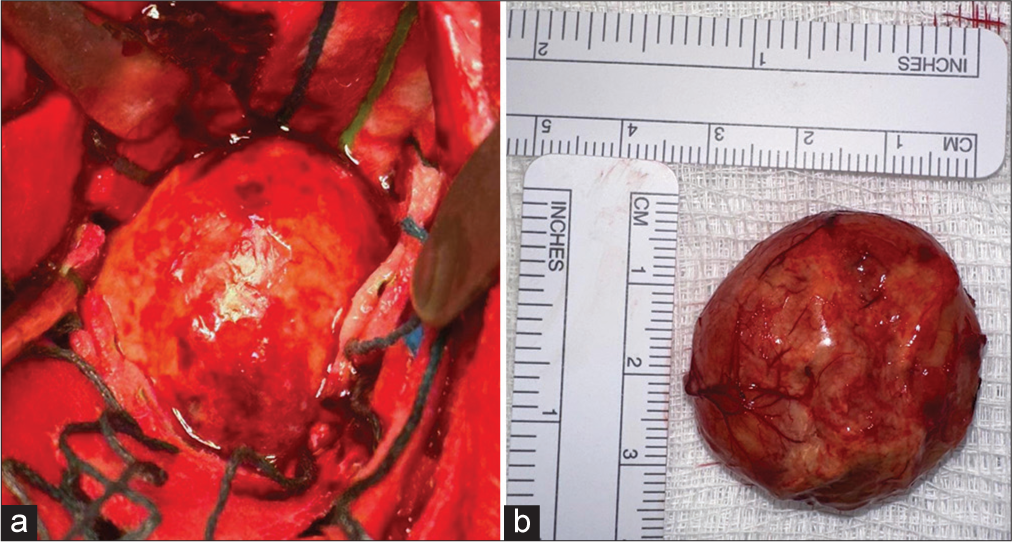
Surgical excision without rupture is the preferred treatment approach to prevent recurrence and anaphylactic reactions. The Dowling-Orlando technique is frequently employed for this purpose. Nevertheless, in our particular case, we carefully separated the cyst capsule from the brain parenchyma through precise dissection. This was necessary because the cyst was situated deep within the brain, extending into the lateral ventricle, and its capsule was thick, opaque, and firmly attached to the surrounding brain tissue. Medical treatment with albendazole and praziquantel can be considered, particularly in recurrent cases or when rupture occurs during surgery.[
CONCLUSION
Neurosurgeons have to bear in mind hydatid cysts when evaluating cystic lesions in the brain. In atypical cases, surgical techniques may vary, and careful dissection of the cyst capsule from the brain parenchyma can be successful with minimal risk of intraoperative rupture.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Altas M, Serarslan Y, Davran R, Evirgen O, Aras M, Yilmaz N. The Dowling-Orlando technique in a giant primary cerebral hydatid cyst: A case report. Neurol Neurochir Pol. 2010. 44: 304-7
2. Arana Iniguez R, Vinken PJ, Bruyn GW, editors. Echinococcus Infection of the nervous system. Hand book of clinical neurology, part III. Amsterdam: Elsevier/North Holland Biomedical Press; 1978. p. 175-208
3. Binesh F, Mehrabanian M, Navabii H. Primary brain hydatosis. BMJ Case Rep. 2011. 2011: bcr0620103099
4. Bükte Y, Kemaloglu S, Nazaroglu H, Ozkan U, Ceviz A, Simsek M. Cerebral hydatid disease: CT and MR imaging findings. Swiss Med Wkly. 2004. 134: 459-67
5. Coates R, von Sinner W, Rahm B. MR imaging of an intracerebral hydatid cyst. AJNR Am J Neuroradiol. 1990. 11: 1249-50
6. Erashin Y, Muthuer S, Guzelbag E. Intracranial hydatid cysts in children. Neurosurgery. 1993. 33: 219-25
7. Gök H, Başkurt O. Giant primary intracranial hydatid cyst in child with hemiparesis. World Neurosurg. 2019. 129: 404-6
8. Karak PK, Mittal M, Bhatia S, Mukhopadhyay S, Berry M. Isolated cerebral hydatid cyst with pathognomonic CT sign. Neuroradiology. 1992. 34: 9-10
9. Kohli A, Gupta RK, Poptani H, Roy R. In vivo proton magnetic resonance spectroscopy in a case of intracranial hydatid cyst. Neurology. 1995. 45: 562-4
10. Nurchi G, Floris F, Montaldo C, Mastio F, Peltz T, Coraddu M. Multiple cerebral hydatid disease: Case report with magnetic resonance imaging study. Neurosurgery. 1992. 30: 436-8
11. Singounas EG, Leventis AS, Sakas DE, Hadley DM, Lampadarios DA, Karvounis PC. Successful treatment of intracerebral hydatid cysts with albendazole: Case report and review of the literature. Neurosurgery. 1992. 31: 571-4
12. Todorov T, Vutova K, Petkov D, Balkanski G. Albendazole treatment of multiple cerebral hydatid cysts: Case report. Trans R Soc Trop Med Hyg. 1988. 82: 150-2






Mona Abd El Fattah
Posted March 23, 2024, 2:32 am
Excellent highly integrated work with high impact