- Department of Surgery, College of Medicine, University of Baghdad, Baghdad, Iraq
- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq
- Department of Surgery, College of Medicine, The University of Babylon, Hillah, Iraq,
- College of Medicine, Gulf Medical University, Ajman, United Arab Emirates,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
DOI:10.25259/SNI_433_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sadik K. Daily1, Mustafa Ismail2, Alzahraa A. Abdulmajeed1, Ameer M. Aynona3, Maliya Delawan4, Mostafa H. Algabri1, Samer S. Hoz5. A case series of gyrus rectus arteriovenous malformation: Clinical characteristics, angioarchitecture, microsurgical treatment, and outcome. 23-Jun-2023;14:219
How to cite this URL: Sadik K. Daily1, Mustafa Ismail2, Alzahraa A. Abdulmajeed1, Ameer M. Aynona3, Maliya Delawan4, Mostafa H. Algabri1, Samer S. Hoz5. A case series of gyrus rectus arteriovenous malformation: Clinical characteristics, angioarchitecture, microsurgical treatment, and outcome. 23-Jun-2023;14:219. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12373
Abstract
Background: Gyrus rectus arteriovenous malformation (AVM) is one of the intricate pathologies that can lead to gyrus rectus hematoma. However, there is a paucity of research on this topic. This case series aims to delineate the characteristics of gyrus rectus AVMs, their outcomes, and treatment strategies.
Methods: We enrolled five cases of gyrus rectus AVM that presented to the Neurosurgery Teaching Hospital in Baghdad, Iraq. Patients with the presence of gyrus rectus AVM were analyzed according to the demographic data, clinical status, radiological imaging, and outcome.
Results: Of the total cases enrolled, all five cases were ruptured at the presentation. Most of the AVMs had arterial feeders from the anterior cerebral artery (80%) and superficial venous drainage through the anterior third of the superior sagittal sinus occurred in four cases (80%). Two of the cases were classified as Spetzler-Martin grade 1 AVMs, two were grade 2, and one was grade 3. With regard to the modified Rankin Score (mRS), four of them had a score of 0 after observation for 30, 18, 26, and 12 months, respectively, while one patient had an mRS score of 1 after 28 months of observation. All five cases presented with seizure and were all treated by surgical resection.
Conclusion: To the best of our knowledge, this is the second report documenting the features of gyrus rectus AVMs and the first one from Iraq. Further, research into gyrus rectus AVMs is required to help better characterize and enhance our knowledge on the outcomes of such lesions.
Keywords: Arteriovenous malformation, Front-basal arteriovenous malformation, Front-basal hemorrhage, Gyrus rectus, Gyrus rectus arteriovenous malformation
INTRODUCTION
Arteriovenous malformation (AVM) is a congenital lesion consisting of an abnormal single or multiple direct connections between a combination of thin or dilated arteries and veins, classically appearing as a “bag of worms” on magnetic resonance imaging. They lead to arteriovenous shunting of blood and cause surrounding neural tissue to become nonfunctional or calcified, which may contribute to the development of seizures and another neurological phenomena.[
The gyrus rectus is part of Bormann’s area 11 and is considered to be the most anatomically constant cerebral gyri. Located medial to the olfactory sulcus at the frontobasal lobe in the anterior cranial fossa, it gets its arterial supply from the orbitofrontal artery, a branch of the anterior communicating artery. It has two groups of venous drainage: A superficial drain into the superior sagittal sinus (SSS) and a deep drain into the basal vein.[
MATERIALS AND METHODS
We enrolled five cases of gyrus rectus AVM that presented to the Neurosurgery Teaching Hospital, which were all ruptured at the time of presentation. Patients with the presence of gyrus rectus AVM were analyzed according to the demographic data, clinical status, radiological imaging, and outcome.
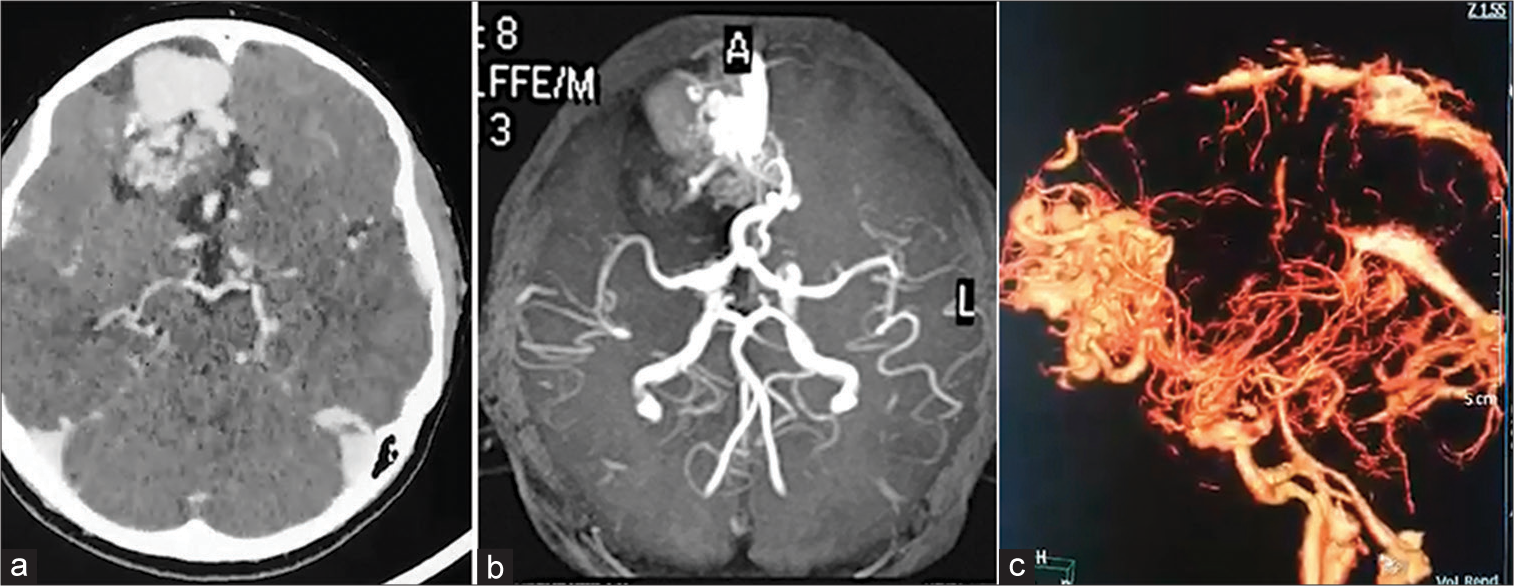
The parameters included were age, gender, Glasgow coma scale (GCS), seizure, and size of AVM in centimeters, whether the AVMs were ruptured or not at the time of presentation, computed tomography (CT) findings, arterial feeders, venous drainage, and method of treatment. The degree of disability of patients postoperative was assessed according to the modified Rankin score (mRS), where a score of 0 is given when there are no symptoms, (1) when there is no significant disability despite symptoms (able to carry out all usual duties and activities), (2) when there is a slight disability (unable to carry out all previous activities, but able to look after own affairs without assistance), (3) when there is a moderate disability (requiring some help, but able to walk without assistance), (4) when there is a moderately severe disability (unable to walk and attend to bodily needs without assistance), (5) when there is a severe disability (bedridden, incontinent, and requiring constant nursing care and attention), and (6) if the patient is dead. To estimate the mortality and morbidity of surgical resection, the AVMs were categorized according to the Spetzler-Martin (SM) AVM grading system, where the grade is equal to the sum of points in three categories: the size of nidus [(1) when it is small (<3 cm), (2) when it is medium (3–6 cm), and (3) when it is large (>6 cm)], location (0 when it is in a noneloquent site, and 1 when it is in an eloquent site), and venous drainage (0 when there are superficial veins, and 1 when there are deep veins), which are all demonstrated in
RESULTS
Of the total cases enrolled, all five cases were ruptured at the presentation. Three were male and two were female. Their age ranged from 14 to 28 years, with a mean age of 21 years. Four of the cases of gyrus rectus AVM had a medium-sized nidus, with three of them measuring 3 cm in size and one measuring 4 cm in size. Only one case was of small size, measuring 2 cm. All patients had ICH as demonstrated on the CT scan: Three of them presented with ICH in the right frontal area, while two of them had ICH in the left frontal area. Four (80%) of the AVMs had arterial feeders from the anterior cerebral artery and one had multiple arterial feeders from the anterior and middle cerebral artery. Four cases only had superficial venous drainage through the anterior third of the SSS with no deep venous drainage. However, one case had both deep drainage into the cavernous sinus and superficial drainage to the SSS. With regard to the SM scale, two cases were classified as grade 1 AVMs, two were grade 2, and one was grade 3. With regard to mRS, four of them had a score of 0 after observation for 30, 18, 26, and 12 months, respectively, while one patient had an mRS score of 1 after 28 months of observation. All five cases presented with seizure and were all treated by surgical resection. All these data are shown in
DISCUSSION
AVMs can be generally described as vascular developmental deformities consisting of tangles of convoluted arteries and veins that allow single or multiple direct connections and high-flow shunting without interfering with capillary beds.[
AVMs can be ruptured or unruptured at the time of presentation. Intracerebral and subarachnoid hemorrhage are the most common clinical presentations for anterior cranial fossa AVMs.[
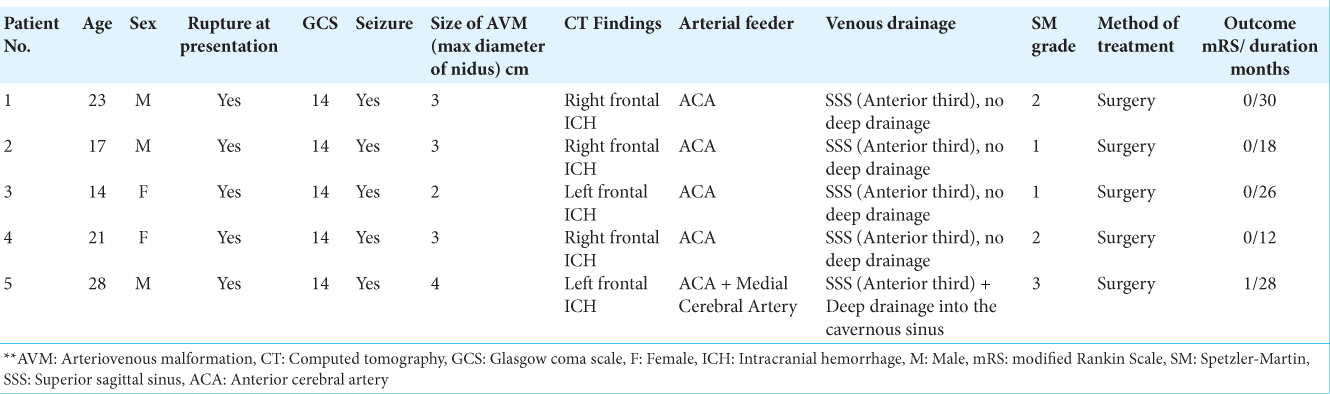
Figure 1:
(a) Computed tomography (CT) scan of the head (axial view) showing right intracerebral hemorrhage (ICH) in the frontal lobe within the rectus gyrus with no signs of subarachnoid hemorrhage. (b) CT angiography of the head (axial view) showing the circle of Willis with a tuft of vessels in the right gyrus rectus. (c) CT angiography of the head (axial view) showing a tuft of vessels with ICH in the right gyrus rectus in the frontal lobe.
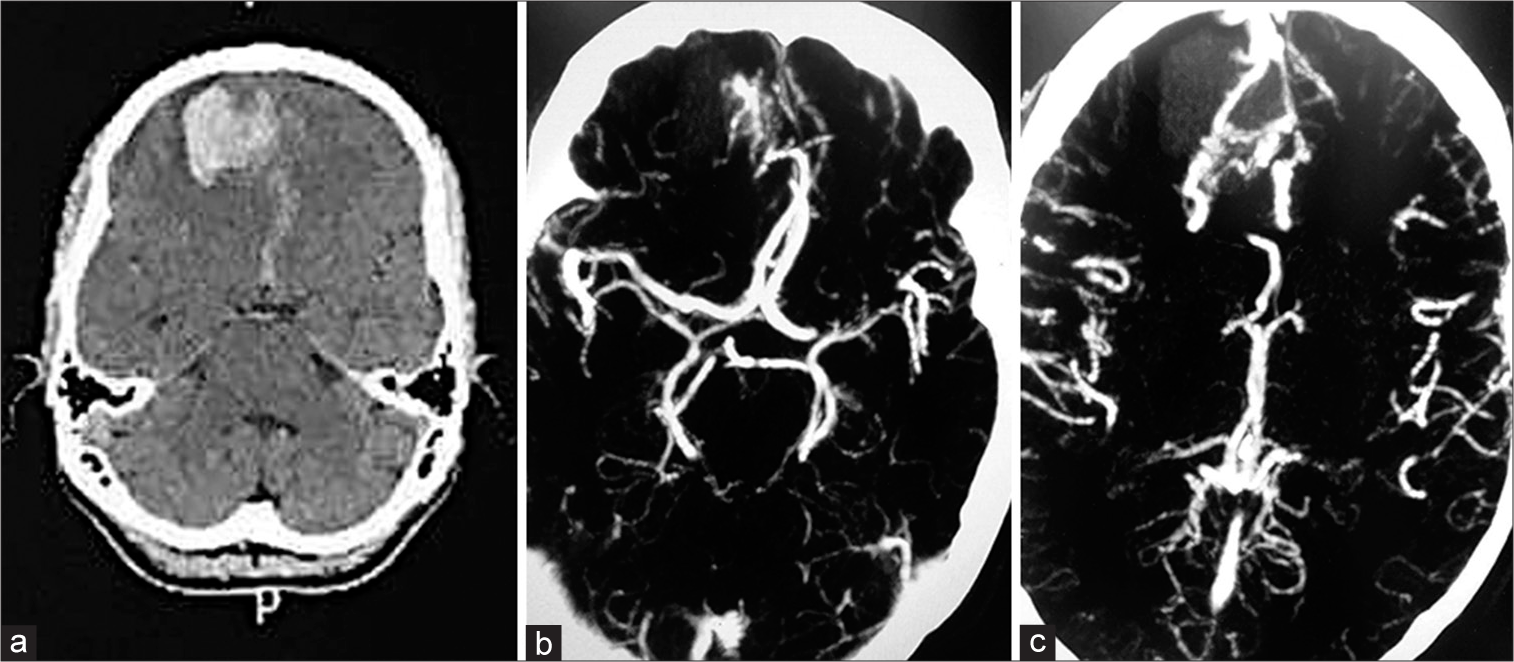
Figure 2:
(a) Computed tomography (CT) scan of the head (axial view) showing left intracerebral hemorrhage in the frontal lobe within the rectus gyrus with no signs of subarachnoid hemorrhage. (b) CT angiography of the head (axial view) showing a tuft of vessels in the left rectus gyrus. (c) 3D-constructed angiography showing an arteriovenous malformation with multiple feeders from the anterior circulation.
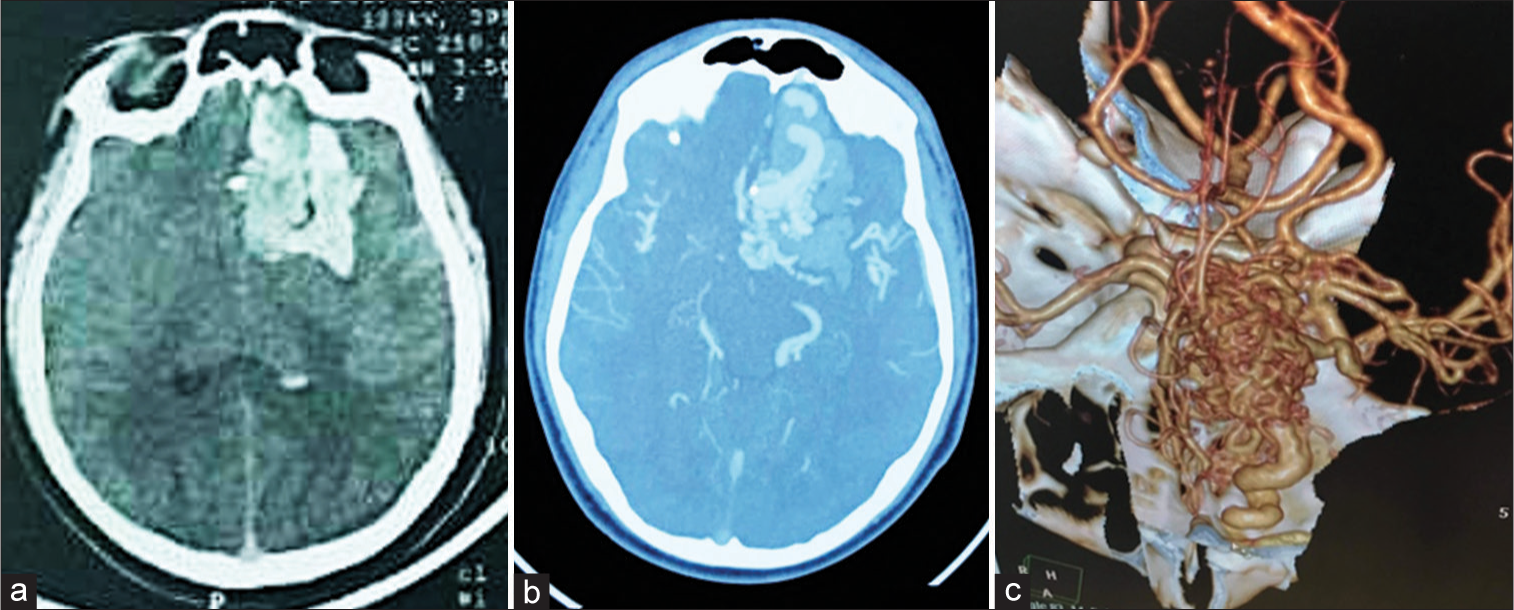
Figure 3:
(a) Computed tomography (CT) scan (axial view) showing right intracerebral hemorrhage in the frontal lobe within the rectus gyrus with no signs of subarachnoid hemorrhage. (b) CT angiography of the head (axial view) showing a tuft of vessels in the right rectus gyrus. (c) 3D-constructed angiography showing an arteriovenous malformation with multiple feeders from the anterior circulation in the frontal lobe.
Around 30% of patients with AVM have been reported to present with a seizure at initial diagnosis, making it the second most common presentation of AVM. In the study by Tong et al., 20.9% of the patients had seizures as the initial presentation.[
The anterior cerebral arteries, medial cerebral arteries, and posterior cerebral arteries are common superficial arterial feeders for cortical AVMs of the anterior cranial fossa, while deep feeder arteries for cortical AVMs include the lenticulostriate artery and the anterior and posterior choroidal arteries.[
Hartmann et al. followed up on 115 patients after AVM hemorrhage with neurological assessment and found that 47% of them had no neurological deficit with an Rankin score (RS) of 0, 7% were assigned an RS score of 4 or 5 after initial or subsequent bleeding, and 37% remained independent in their daily activity with an RS of 1.[
Surgical resection is indicated when the AVM is complicated by hemorrhage and is the treatment of choice for AVMs in the anterior cranial fossa due to its high efficacy and low postoperative morbidity.[
Limitations
One of the major limitations of this study is that we have a very limited number of patients. However, we intended to highlight this location of AVM as potentially different and perhaps a special form of AVM. We suggest that future studies may include international collaboration to allow for the recruitment of more cases to have a better understanding of the characteristics of gyrus rectus AVM.
CONCLUSION
Our study offers rare insight into the characteristics of frontobasal AVMs, which is an important pathology that can lead to the development of GRH. To the best of our knowledge, this is the second report documenting the features of gyrus rectus AVMs and the first one from Iraq. The study identified the presence of gender predilection, seizure, and rupture at presentation among the enrolled patients. We also identified the GCS, location of the AVM, SM grade, and mRS of the patients, in addition to describing the arterial supply and venous drainage of each of the cases. Further, research into gyrus rectus AVMs is required to help better characterize and enhance our knowledge on the outcomes of such lesions.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abumiya T, Kamiyama H, Murata J, Nunomura M, Chono Y, Kobayashi N. Dural arteriovenous malformation with uncommon draining veins in the anterior fossa. Case report. Neurol Med Chir (Tokyo). 1987. 27: 1195-200
2. Bioh S, Nakagawa H, Arita N, Fujiwara M. Dural arteriovenous malformation in the anterior fossa. Case report. Neurol Med Chir (Tokyo). 1981. 21: 131-4
3. Choi JH, Mohr JP. Brain arteriovenous malformations in adults. Lancet Neurol. 2005. 4: 299-308
4. Dănăilă L. Microsurgical treatment of the interhemispheric arteriovenous malformations. Chirurgia (Bucur). 2012. 107: 701-14
5. Ding D, Starke RM, Quigg M, Yen CP, Przybylowski CJ, Dodson BK. Cerebral arteriovenous malformations and epilepsy, Part 1: Predictors of seizure presentation. World Neurosurg. 2015. 84: 645-52
6. Fleetwood IG, Steinberg GK. Arteriovenous malformations. Lancet. 2002. 359: 863-73
7. Garcin B, Houdart E, Porcher R, Manchon E, Saint-Maurice JP, Bresson D. Epileptic seizures at initial presentation in patients with brain arteriovenous malformation. Neurology. 2012. 78: 626-31
8. Ghossoub M, Nataf F, Merienne L, Devaux B, Turak B, Roux FX. Characteristics of epileptic seizures associated with cerebral arteriovenous malformations. Neurochirurgie. 2001. 47: 168-76
9. Gliemroth J, Nowak G, Arnold H. Dural arteriovenous malformation in the anterior cranial fossa. Clin Neurol Neurosurg. 1999. 101: 37-43
10. Hartmann A, Mast H, Mohr JP, Koennecke HC, Osipov A, Pile-Spellman J. Morbidity of intracranial hemorrhage in patients with cerebral arteriovenous malformation. Stroke. 1998. 29: 931-4
11. Ishikawa T, Houkin K, Tokuda K, Kawaguchi S, Kashiwaba T. Development of anterior cranial fossa dural arteriovenous malformation following head trauma. Case report. J Neurosurg. 1997. 86: 291-3
12. Ismail M, Elamin O, Al-Ageely TA, Algburi HA, Sharma M, Aljuboori Z. Rectus gyrus hematoma: An overview. Surg Neurol Int. 2022. 13: 558
13. Kaplan SS, Ogilvy CS, Crowell RM. Incidentally discovered arteriovenous malformation of the anterior fossa dura. Br J Neurosurg. 1994. 8: 755-9
14. Kareem ZM, Arnaout MM, Al-Baidar RA, Al-Sharshahi ZF, Hoz SS. Neurosurgery-cases and reviews. Management. 2021. 4: 5
15. Kobayashi H, Hayashi M, Noguchi Y, Tsuji T, Handa Y, Caner HH. Dural arteriovenous malformations in the anterior cranial fossa. Surg Neurol. 1988. 30: 396-401
16. Li M, Jiang P, Wu J, Guo R, Deng X, Cao Y. Altered brain structural networks in patients with brain arteriovenous malformations located in Broca’s Area. Neural Plast. 2020. 2020: 8886803
17. Martin NA, King WA, Wilson CB, Nutik S, Carter LP, Spetzler RF. Management of dural arteriovenous malformations of the anterior cranial fossa. J Neurosurg. 1990. 72: 692-7
18. Melamed I, Merkin V, Korn A, Nash M. The supraorbital approach: An alternative to traditional exposure for the surgical management of anterior fossa and parasellar pathology. Minim Invasive Neurosurg. 2005. 48: 259-63
19. Morcos JJ, Heros RC, Carter LP, Spetzler RF, editors. Supratentorial arteriovenous malformations. Neurovascular Surgery. New York: McGraw-Hill; 1995. p. 979-1004
20. Piepgras DG, Sundt TM, Ragoowansi AT, Stevens L. Seizure outcome in patients with surgically treated cerebral arteriovenous malformations. J Neurosurg. 1993. 78: 5-11
21. Ramos A, Chaddad-Neto F, Joaquim AF, Campos-Filho JM, Mattos JP, Ribas GC. The microsurgical anatomy of the gyrus rectus area and its neurosurgical implications. Arq Neuropsiquiatr. 2009. 67: 90-5
22. Rapacki TF, Brantley MJ, Furlow JT, Geyer CA, Toro VE, George ED. Heterogeneity of cerebral cavernous hemangiomas diagnosed by MR imaging. J Comput Assist Tomogr. 1990. 14: 18-25
23. Stapf C, Mohr JP, Pile-Spellman J, Solomon RA, Sacco RL, Connolly ES. Epidemiology and natural history of arteriovenous malformations. Neurosurg Focus. 2001. 11: e1
24. Tong X, Wu J, Lin F, Cao Y, Zhao Y, Ning B. The effect of age, sex, and lesion location on initial presentation in patients with brain arteriovenous malformations. World Neurosurg. 2016. 87: 598-606
25. Valli D, Zhao X, Belykh E, Sun Q, Lawton MT, Preul MC. Partial gyrus rectus resection as a technique to improve the exposure to the anterior communicating artery complex through the junctional triangle: A quantitative study. J Neurol Surg B Skull Base. 2021. 82: e211-6
26. White DV, Sincoff EH, Abdulrauf SI. Anterior ethmoidal artery: Microsurgical anatomy and technical considerations. Neurosurgery. 2005. 56: 406-10
27. Winckler C, Magezi D, Croquelois A. Restricted left gyrus rectus haemorrhage with unusual frontal syndrome presentation. Eur Neurol. 2011. 65: 129
28. Woo HH, Jafar JJ. Management of cortical arteriovenous malformations. Contemp Neurosurg. 2000. 22: 1-9
29. Xu K, Ji T, Li C, Yu J. Current status of endovascular treatment for dural arteriovenous fistulae in the anterior cranial fossa: A systematic literature review. Int J Med Sci. 2019. 16: 203-11