- Department of Neurosurgery, Evangelismos General Hospital, National and Kapodistrian University of Athens Medical School, Athens, Greece
- National and Kapodistrian University of Athens Medical School, Athens, Greece
Correspondence Address:
Georgios P. Skandalakis
Department of Neurosurgery, Evangelismos General Hospital, National and Kapodistrian University of Athens Medical School, Athens, Greece
DOI:10.4103/sni.sni_214_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Georgios P. Skandalakis, Stefanos Korfias, Aristotelis V. Kalyvas, Christos Anagnostopoulos, Damianos E. Sakas. A giant pseudoaneurysm of the occipital artery. 20-Nov-2017;8:281
How to cite this URL: Georgios P. Skandalakis, Stefanos Korfias, Aristotelis V. Kalyvas, Christos Anagnostopoulos, Damianos E. Sakas. A giant pseudoaneurysm of the occipital artery. 20-Nov-2017;8:281. Available from: http://surgicalneurologyint.com/surgicalint-articles/a-giant-pseudoaneurysm-of-the-occipital-artery/
Abstract
Background:Pseudoaneurysms of the occipital artery (OA) are extremely rare and can occur following head trauma or iatrogenic injury; OA anatomy seems to play a crucial role in their pathogenesis.
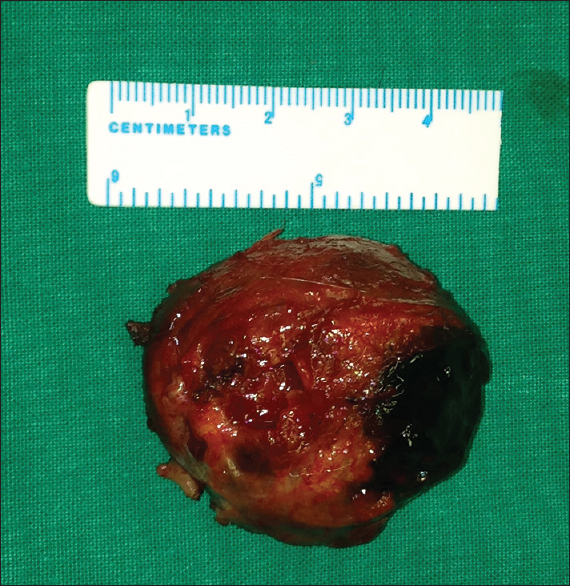
Case Description:This report describes the case of a 76-year-old patient with a giant OA pseudoaneurysm secondary to a head injury the patient had sustained 1 month earlier. After radiological confirmation via ultrasonography (US) and computed tomography angiography (CTA), the patient underwent surgery for resection of the lesion. An uneventful postoperative course with no recurrence was confirmed at 1 and 2-month follow-up visits.
Conclusions:Despite their rarity, pseudoaneurysms of the OA should be considered in the differential diagnosis of patients presenting with an occipital pulsatile mass. Prompt management reduces the risk of a serious hemorrhage. In our case, considering the size of the lesion, surgical resection seemed to be the only reasonable option.
Keywords: Giant pseudoaneurysm, head injury, occipital artery false aneurysm, occipital artery pseudoaneurysm, trauma
INTRODUCTION
Occipital artery (OA) pseudoaneurysms are extremely rare entities and can occur after blunt or penetrating trauma or iatrogenic injury. Clinical presentation may vary; however, the most typical is an enlarging, tender, pulsatile mass on the occipital region accompanied by ipsilateral occipital headache.[
CASE REPORT
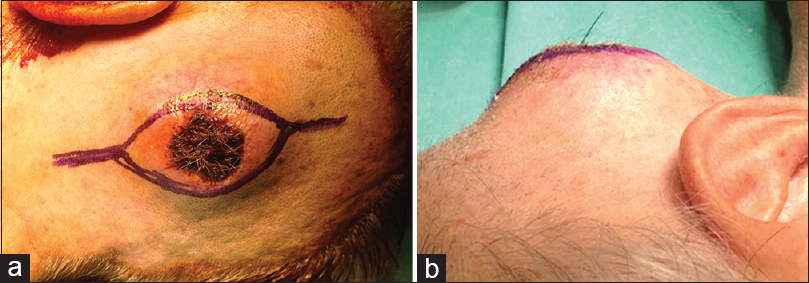
A 76-year-old male presented to the Emergency Department with a laceration on his left occipital region after a fall from standing height. The CT scan was negative for traumatic brain injury; the patient was sutured and discharged. One month later he presented again complaining of a constantly enlarging mass in his left occiput. Physical examination revealed a tender, pulsatile mass with central necrosis of the epidermis. The pulsation of the mass seized subsequent to compression of the OA proximal to the lesion. Neurological examination was normal.
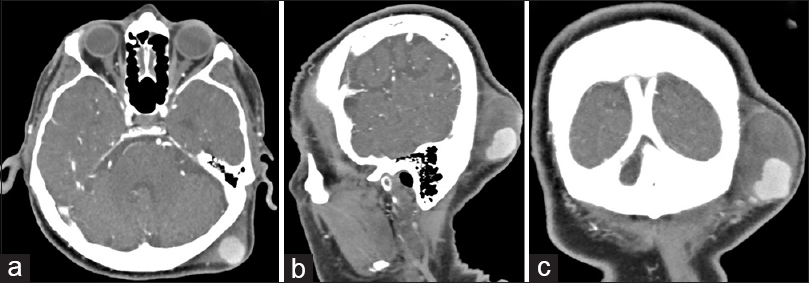
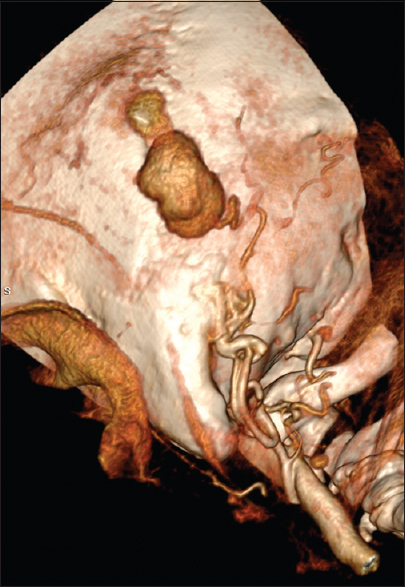
Doppler ultrasound was performed to confirm the presence of a pseudoaneurysm, demonstrating a subcutaneous anechoic mass to the left lateral border of the occipital bone with a high intrinsic arterial flow. Subsequently, the patient underwent CTA, which demonstrated the anatomic continuity of the mass with the left OA. Furthermore, a large isodense mass around the hyperdense enhancement was revealed, indicating the surrounding thrombus [
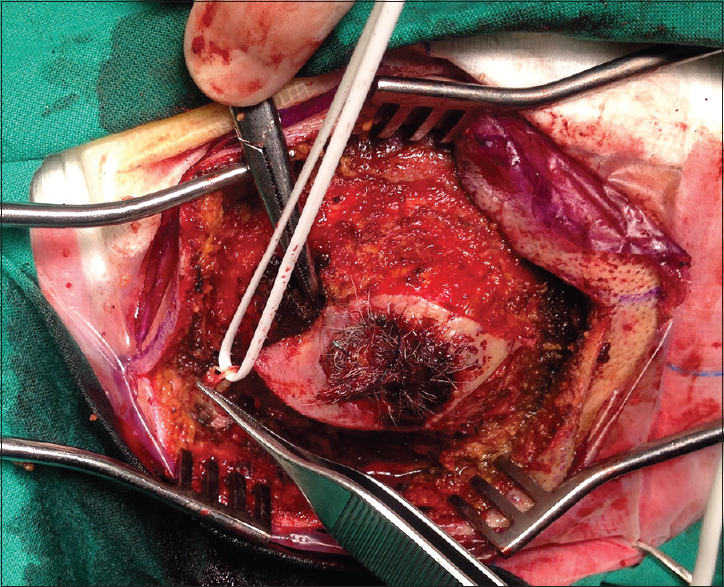
The pathological examination revealed hyalinization of the arterial wall and a focally disrupted intima and media, which were consistent with the diagnosis of a pseudoaneurysm. The patient was discharged the next day. An uneventful wound healing with no recurrence were confirmed at 1 and 2-month follow-up visits. An informed consent for publication of this case report was obtained from the patient.
DISCUSSION
Pseudoaneurysms are characterized by a defect of the blood vessel wall and by direct communication with the endovascular blood flow. Their wall is formed by adventitia or perivascular tissue or a thrombus.[
Most OA pseudoaneurysms are diagnosed in patients with a history of head trauma.[
Regarding treatment, surgical or endovascular means are advocated.[
CONCLUSION
This manuscript presents the successful surgical resection of the largest (71 × 61 × 43 mm) OA pseudoaneurysm published in the literature highlighting the importance of the diagnosis and surgical treatment. The etiology of the OA pseudoaneurysm development among published cases is also discussed, stressing the role of OA anatomy on their pathogenesis as the subgaleal part of the occipital artery, located above the level of the superior nuchal line, is the most vulnerable to injury. OA pseudoaneurysms are extremely rare and data comparing the optimal diagnostic and treatment modalities are lacking. Nevertheless, pseudoaneurysms of the OA should always be considered in the differential diagnosis of pulsatile masses of the occipital region and should promptly be managed to reduce the risk of hemorrhage while alleviating pain.
Financial support and sponsorship
Nil.
Conflicts of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval: For this type of study informed consent was signed and obtained from the patient.
References
1. Alvernia JE, Fraser K, Lanzino G. The occipital artery: A microanatomical study. Neurosurgery. 2006. 58: ONS114-
2. Anan M, Kamida T, Abe T, Fujiki M. Traumatic Aneurysm of the Occipital Artery. Neurosurg Quart. 2008. 18: 221-2
3. Changa AR, Meleis AM, Bassani L. Delayed Occipital Artery Pseudoaneurysm Following Blunt Force Trauma. World Neurosurg. 2016. 89: 732.e731-2.e736
4. Chaudhry NS, Gaynor BG, Hussain S, Dernbach PD, Aziz-Sultan MA. Etiology and Treatment Modalities of Occipital Artery Aneurysms. World Neurosurg. 2017. p.
5. Kumar V, Abbas AK, Fausto N, Aster JC.editorsRobbins and Cotran pathologic basis of disease. Elsevier Health Sciences; 2014. p.
6. Patel M, Tchelepi H, Rice DH. Traumatic pseudoaneurysm of the occipital artery: Case report and review of the literature. Ear Nose Throat J. 2008. 87: E7-12
7. Srinivasan VM, Karas PJ, Sen AN, Fridley JS, Chen SR, Gopinath SP. Occipital Artery Pseudoaneurysm After Posterior Fossa Craniotomy. World Neurosurg. 2017. 98: 868.e861-868.e864
8. Tambasco N, Hamam M, Castrioto C, Calabresi P, Rossi A. Occipital pseudoaneurysm as a complication of extension channel placement for DBS in Parkinson's disease. Mov Disord. 2007. 22: 1834-6