- Department of Neurosurgery, Fundación Santa Fe de Bogotá, Bogotá, Colombia
- Department of Neurosurgery, Universidad Nacional de Colombia, Bogotá, Colombia
- Stroke and Cerebrovascular Center, Fundación Santa Fe de Bogota, Bogotá, Colombia
Correspondence Address:
Diego Gomez, Department of Neurosurgery, Fundación Santa Fe de Bogotá, Bogotá, Colombia.
DOI:10.25259/SNI_115_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Diego Gomez1, Luis Garcia Rairan2, Juan Andres Mejia3, Fernando Hakim1. A novel approach to addressing intercavernous sinus bleeding: Preoperative onyx embolization in the endoscopic endonasal approach for craniopharyngioma resection. 02-Aug-2024;15:270
How to cite this URL: Diego Gomez1, Luis Garcia Rairan2, Juan Andres Mejia3, Fernando Hakim1. A novel approach to addressing intercavernous sinus bleeding: Preoperative onyx embolization in the endoscopic endonasal approach for craniopharyngioma resection. 02-Aug-2024;15:270. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13026
Abstract
Background: Hemorrhage originating from the intercavernous sinuses during transsphenoidal approaches for skull base injury is a common occurrence, but it can be easily controlled. However, in specific cases, it may necessitate suspending the surgery or result in hemodynamic instability.
Case Description: We present the case of a 7-year-old female patient who underwent transsphenoidal endoscopic endonasal for craniopharyngioma resection. The patient’s parents gave consent for the procedure. During the procedure, significant intraoperative bleeding occurred, which was necessary to stop the resection. After the surgery, cerebral angiography was performed, which identified a prominent anterior intercavernous venous sinus as the source of the bleeding. A successful embolization using onyx was performed, leading to a satisfactory postoperative recovery without any complications. The patient then underwent a second surgical intervention for the resection of the craniopharyngioma through an endoscopic endonasal transsphenoidal approach. This procedure achieved a complete resection of the lesion without complications, and the patient experienced an adequate postoperative recovery.
Conclusion: The objective of this case is to describe a previously unreported technique involving onyx embolization for controlling prominent bleeding from the intercavernous sinus and as a presurgical embolization method to reduce the risk of bleeding during endoscopic endonasal surgery for resection of a craniopharyngioma.
Keywords: Bleeding, Embolization, Intercavernous sinus, Onyx
INTRODUCTION
The transsphenoidal approach is currently considered the preferred surgical treatment for sellar lesions (such as pituitary adenomas, craniopharyngiomas, meningiomas, and dysgerminomas) or some infradiaphragmatic lesions.[
Although microsurgery and endoscopy are considered minimally invasive during transsphenoidal approaches, they are still susceptible to causing cerebrospinal fluid leaks and vascular injury due to their proximity to large vessels such as the internal carotid artery.[
In situations where prominent intercavernous sinuses are evident (a group of venous channels encircling the pituitary gland and connecting both cavernous sinuses[
Addressing massive bleeding from the intercavernous sinuses presents a challenge in surgical practice, as there is currently no standard method for its management. Various techniques have been employed to control bleeding.[
This report aims to present a singular case of onyx embolization as a presurgical technique to reduce the risk of bleeding and manage profuse hemorrhage from the intercavernous sinuses during the endoscopic approach for craniopharyngioma resection.
CASE DESCRIPTION
The patient is a 7-year-old female with a history of craniopharyngioma who underwent transcranial surgery 7 months ago. Following the surgery, she developed hydrocephalus, necessitating the placement of a ventriculoperitoneal shunt. However, despite the intervention, the patient continued to experience persistent diabetes insipidus and hormonal imbalances in the pituitary axis. In addition, campimetric clippings consistent with bitemporal hemianopia were observed.
A brain magnetic resonance imaging study revealed a heterogeneous suprasellar lesion with solid and cystic components extending to the third ventricle, retrochiasmatic region, and posterior fossa [
Figure 1:
Brain magnetic resonance imaging. (a) Residual suprasellar lesion, characterized by both cystic and solid components, was identified. This lesion corresponds to a previously identified craniopharyngioma, which is causing compression of the chiasm, with a more pronounced effect on the right side. The dimensions of the lesion measure 1.3 cm × 2.1 cm × 1.8 cm.
During the procedure, effective control was established over a 400 cc bleed at the dural opening. However, the patient experienced cardiorespiratory arrest due to volume depletion. Resuscitation maneuvers were promptly initiated, and fluid resuscitation was administered until spontaneous circulation was restored. Subsequently, the patient was promptly transferred to the intensive care unit for further management. Despite these interventions, comprehensive resection of the tumor proved unattainable.
Following the stabilization of the patient’s condition, an angiographic study was conducted on the subsequent day, revealing the notable and patent presence of the anterior intercavernous venous sinus. Presurgical embolization utilizing onyx was undertaken in anticipation of a second surgical intervention, given the heightened risk of rebleeding associated with a subsequent transsphenoidal attempt to achieve complete tumor resection. Continuous monitoring of vital signs was rigorously maintained throughout the presurgical embolization procedure to identify any potential hemodynamic instabilities promptly.
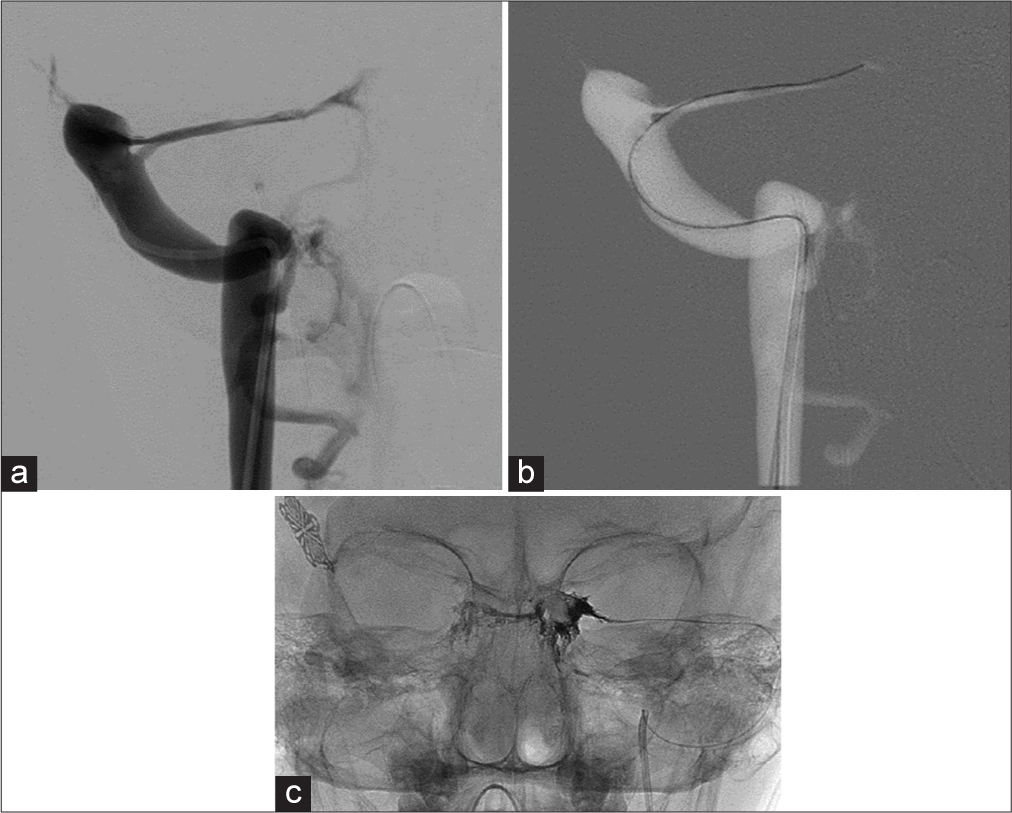
After the femoral vein puncture, supraselective catheterization of the bilateral superior petrosal sinuses was carried out, starting with the dominant side (left), utilizing a guiding catheter for support placed in the jugular gulf [
Figure 2:
Occlusion of a lesion in intracranial vessels through endovascular approach: bilateral vertebral artery (panangiography): (a) The jugular access is marked for injection from the left sigmoid sinus, where the superior petrosal sinus is identified. (b) Using a microcatheter and microguide, navigation is performed (c) from the superior petrosal sinus to the left cavernous sinus.
Video 1
Video 2
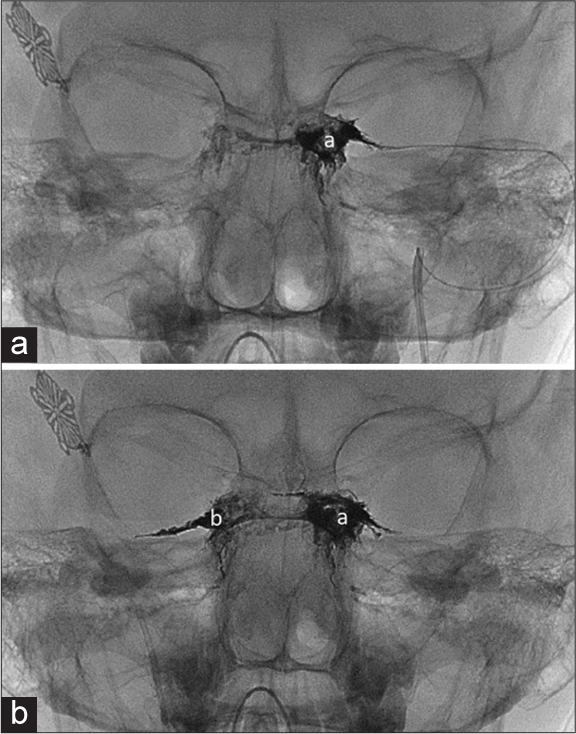
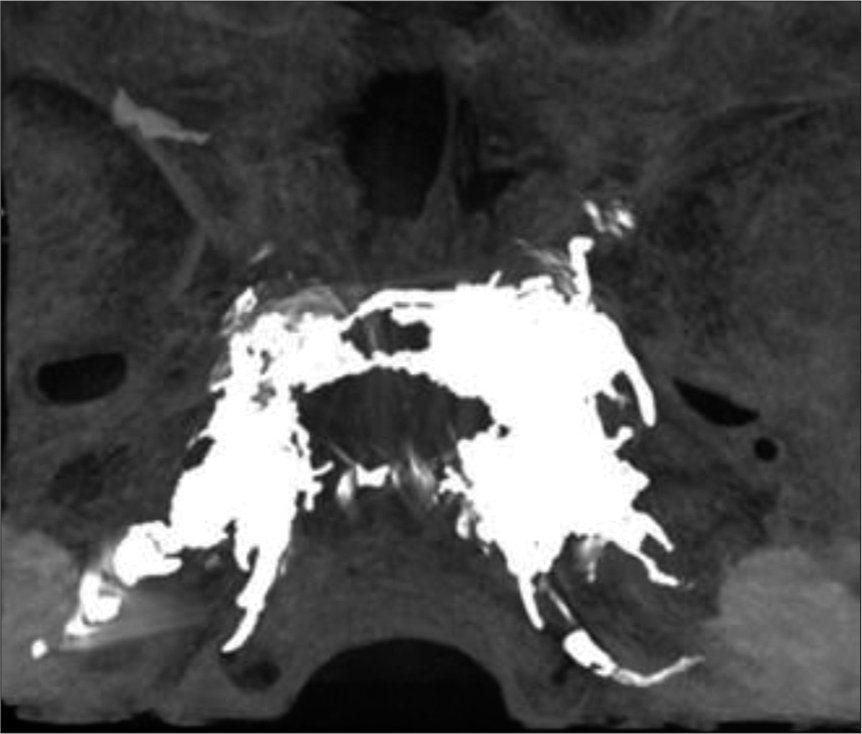
The arteriographic study confirmed appropriate arterial and venous phases, redirecting venous outflow toward bilateral pterygoid plexuses and bilateral superficial middle venous systems [
A second transnasal endoscopic procedure was conducted without bleeding, resulting in a complication-free complete resection of the craniopharyngioma [
Figure 5:
Brain magnetic resonance imaging: (a) A residual suprasellar lesion, characterized by both cystic and solid components, is consistent with a craniopharyngioma. Postsurgical changes are evident following a transsphenoidal approach for resection of the craniopharyngioma. (b) Subacute hematic remnants are observed in the surgical bed, with no evidence of lesions suggesting tumor residue.
DISCUSSION
The intercavernous sinuses play a crucial role in connecting the cavernous sinuses. They can generally be classified into three categories: the anterior intercavernous sinus (AIS), the posterior intercavernous sinus (PIS), and the inferior intercavernous sinus, with their arrangement varying significantly. Among them, the AIS is believed to be the most prevalent.[
Large intercavernous sinuses can lead to profuse bleeding, which can complicate visualization during surgery and have been associated with venous air embolism in transsphenoidal surgery.[
During transsphenoidal surgery, the occurrence of profuse bleeding from the intercavernous sinuses has prompted the exploration of various measures to contain it. For instance, Salimi et al.[
Various hemostatic techniques have been employed to manage massive hemorrhage from the intercavernous sinuses. These methods include focal compression, direct suture, bipolar electrocautery,[
Onyx is a nonadhesive liquid medium composed of ethylenevinyl-alcohol copolymer, dimethyl sulfoxide, and tantalum. Unlike cyanoacrylates, onyx belongs to the category of copolymers, which are characterized by having a more plastic state. Since its introduction, onyx has demonstrated both efficacy and safety for endovascular embolization of cerebral vascular malformations.[
One of its advantages is its ability to minimize catheter fixation to the vascular pedicle, allowing for a controlled and gradual injection of the embolic material.[
The unique characteristics of the low-resistance system associated with the cavernous sinuses render them susceptible to occlusion by embolic fluids such as onyx, facilitating maximal filling of available spaces. However, caution is warranted during onyx embolization in cavernous sinuses due to the potential for hemodynamic instability arising from the trigeminal cardiac reflex, one of the nerves housed within the cavernous sinus. This reflex is triggered by stimulation of the trigeminal nerve along its course, leading to cardiac disturbances such as bradycardia, asystole, and hypotension.[
Stimulation around the sensory division of the fifth cranial nerve initiates signals transmitted to the sensory nucleus of the trigeminal nerve through the Gasserian ganglion. The afferent pathway continues through short internuncial nerve fibers in the reticular formation, connecting with the efferent pathway in the motor nucleus of the vagus nerve. Consequently, the reflex predominantly induces negative cardiovascular effects through the activation of vagus nerve depressor fibers that terminate in the myocardium.[
In the current case, notable hemodynamic instability was not observed during presurgical embolization since the cavernous sinus was not directly targeted; however, pressure fluctuations within the cavernous sinuses could potentially impact the trigeminal cardiac reflex. Therefore, diligent monitoring of heart rate and blood pressure is imperative, with prompt intervention warranted for any hemodynamic changes to prevent potential asystole.[
In terms of surgical management, onyx occlusion proves to be more advantageous than using coils, as the presence of endovascular coils can lead to significant complications during the surgical procedure. In this context, onyx leverages the principle of resistance to attain a uniform distribution of the embolic fluid within the venous vascular lumen. Coils, employed for proximal occlusion, fall short of ensuring comprehensive occlusion. Should a subsequent procedure be contemplated, these coils may pose challenges in the transnasal resection of the tumor.
An illustrative case highlights the successful utilization of onyx for presurgical embolization, effectively reducing the risk of bleeding and managing profuse hemorrhage from the intercavernous sinus without any associated complications.
CONCLUSION
The onyx embolization technique can be considered safe and effective in managing profuse bleeding from the intercavernous sinus and for presurgical embolization to reduce the risk of bleeding during transsphenoidal approaches. However, further prospective studies are necessary to assess the effectiveness of this technique comprehensively.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Videos available on:
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Crowley RW, Ducruet AF, Kalani MY, Kim LJ, Albuquerque FC, McDougall CG. Neurological morbidity and mortality associated with the endovascular treatment of cerebral arteriovenous malformations before and during the Onyx era. J Neurosurg. 2015. 122: 1492-7
2. Hide T, Yano S, Shinojima N, Kuratsu JI. Usefulness of the indocyanine green fluorescence endoscope in endonasal transsphenoidal surgery. J Neurosurg. 2015. 122: 1185-92
3. Hofstetter C, Anand VK, Schwartz TH. Endoscopic transsphenoidal pituitary surgery. Oper Tech Otolayngol Head Neck Surg. 2011. 22: 206-14
4. Hong Y, Chen S, Guo S, Yu J, Wu Q, Zhang J. A new technique for management of intercavernous sinus bleeding with titanium clips in transsphenoidal surgery. Neurol India. 2010. 58: 847-51
5. Jalaly J, Dalfino J, Mousa SA. Onyx® in the management of cranial arteriovenous malformations. Expert Rev Med Devices. 2013. 10: 453-9
6. Kosty J, Peterson R, Miriyala S, Banks T, Kandregula S, Dossani R. An anatomic assessment of the intercavernous sinuses and review of the literature. J Neurol Surg B Skull Base. 2022. 84: 266-71
7. Lapi D, Scuri R, Colantuoni A. Trigeminal cardiac reflex and cerebral blood flow regulation. Front Neurosci. 2016. 10: 221561
8. Li K, Zhang J, Wang XS, Ye X, Zhao YL. A systematic review of effects and complications after transsphenoidal pituitary surgery: Endoscopic versus microscopic approach. Minim Invasive Ther Allied Technol. 2019. 29: 317-25
9. Orozco LD, Buciuc RF, Parent AD. Endovascular embolization of prominent intercavernous sinuses for successful transsphenoidal resection of cushing microadenoma: Case report. Neurosurgery. 2012. 71: 204-8
10. Salimi A, Sharifi G, Bahrani H, Mohajerani SA, Jafari A, Safari F. Dexmedetomidine could enhance surgical satisfaction in Trans-sphenoidal resection of pituitary adenoma. J Neurosurg Sci. 2017. 61: 46-52
11. Schaller B, Cornelius JF, Prabhakar H, Koerbel A, Gnanalingham K, Sandu N. The trigemino-cardiac reflex: An update of the current knowledge. J Neurosurg Anesthesiol. 2009. 21: 187-95
12. Tian C, Wang X, Wang X, Xiong W. Letter: An imaginary hemostasis device for sinus bleeding during transsphenoidal surgery. Neurosurgery. 2015. 78: E160-1
13. Vollherbst DF, Chapot R, Bendszus M, Möhlenbruch MA. Glue, onyx, squid or PHIL? liquid embolic agents for the embolization of cerebral arteriovenous malformations and Dural arteriovenous fistulas. Clin Neuroradiol. 2022. 32: 25-38
14. Wahl L, Lockwood JD, Keet K, Henry BM, Gielecki J, Iwanaga J. The inferior intercavernous sinus: An anatomical study with application to trans-sphenoidal approaches to the pituitary gland. Clin Neurol Neurosurg. 2020. 196: 106000
15. Yamada S, Fukuhara N, Oyama K, Takeshita A, Takeuchi Y, Ito J. Surgical outcome in 90 patients with craniopharyngioma: An evaluation of transsphenoidal surgery. World Neurosurg. 2010. 74: 320-30