- Department of Neurosurgery, University of Illinois at Chicago, Chicago, United States
- Department of Neurosurgery, Cerebrovascular Surgery and Interventions Center, Boston Children’s Hospital, Harvard Medical School, Boston, United States.
Correspondence Address:
Richard Bram, Department of Neurosurgery, University of Illinois at Chicago, Chicago, United States.
DOI:10.25259/SNI_950_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Richard Bram1, Jason L. Choi1, Alfred P. See2, Gursant S. Atwal1. A persistent trigeminal artery demonstrates cerebrovascular embryologic development. 03-Feb-2023;14:40
How to cite this URL: Richard Bram1, Jason L. Choi1, Alfred P. See2, Gursant S. Atwal1. A persistent trigeminal artery demonstrates cerebrovascular embryologic development. 03-Feb-2023;14:40. Available from: https://surgicalneurologyint.com/surgicalint-articles/12140/
Abstract
Background: Cerebrovascular embryologic development is characterized by the presence of four well-described carotid-vertebrobasilar (VB) anastomoses. As the fetal hindbrain matures and the VB system develops, these connections involute, yet some may persist into adulthood. The persistent primitive trigeminal artery (PPTA) is the most common of these anastomoses. In this report, we describe a unique variant of the PPTA and a four-way division of the VB circulation.
Case Description: A female in her 70s presented with a Fisher Grade 4 subarachnoid hemorrhage. Catheter angiography revealed a fetal origin of the left posterior cerebral artery (PCA) giving rise to a left P2 aneurysm which was coiled. A PPTA arose from the left internal carotid artery and supplied the distal basilar artery (BA) including the superior cerebellar arteries bilaterally and the right but not left PCA. The mid-BA was atretic and the anterior inferior cerebellar artery-posterior inferior cerebellar artery complexes were fed solely from the right vertebral artery.
Conclusion: Our patient’s cerebrovascular anatomy represents a unique variant of the PPTA not well described in the literature. This demonstrates how hemodynamic capture of the distal VB territory by a PPTA is sufficient to prevent fusion of the BA.
Keywords: Carotid-basilar anastomosis, Fetal intracranial artery, Persistent trigeminal artery, Trigeminal artery, Trigeminal
INTRODUCTION
The very first description of a persistent primitive trigeminal artery (PPTA) dates back to 1844 during an autopsy study by English anatomist and surgeon Richard Quain.[
CASE REPORT
History and examination
A female in her 70s with a history of hypertension and hyperlipidemia developed the sudden-onset of headache and slurred speech followed by unresponsiveness. Initial computed tomography (CT) imaging revealed a Fisher Grade 4 subarachnoid hemorrhage. There was prominent blood in the suprasellar, pre-pontine, and left perimesencephalic cisterns with an intraparenchymal component extending to the left thalamus, midbrain, and cerebellum. On transfer to our institution, her neurological examination was poor with evidence of a weak cough reflex and flexion of the lower extremities to painful stimulus.
Intervention and post-procedural course
After the placement of an external ventricular drain for the treatment of acute hydrocephalus, she underwent a diagnostic cerebral angiogram which revealed a multilobular left P2 aneurysm measuring 8.0 mm in maximum dimension [
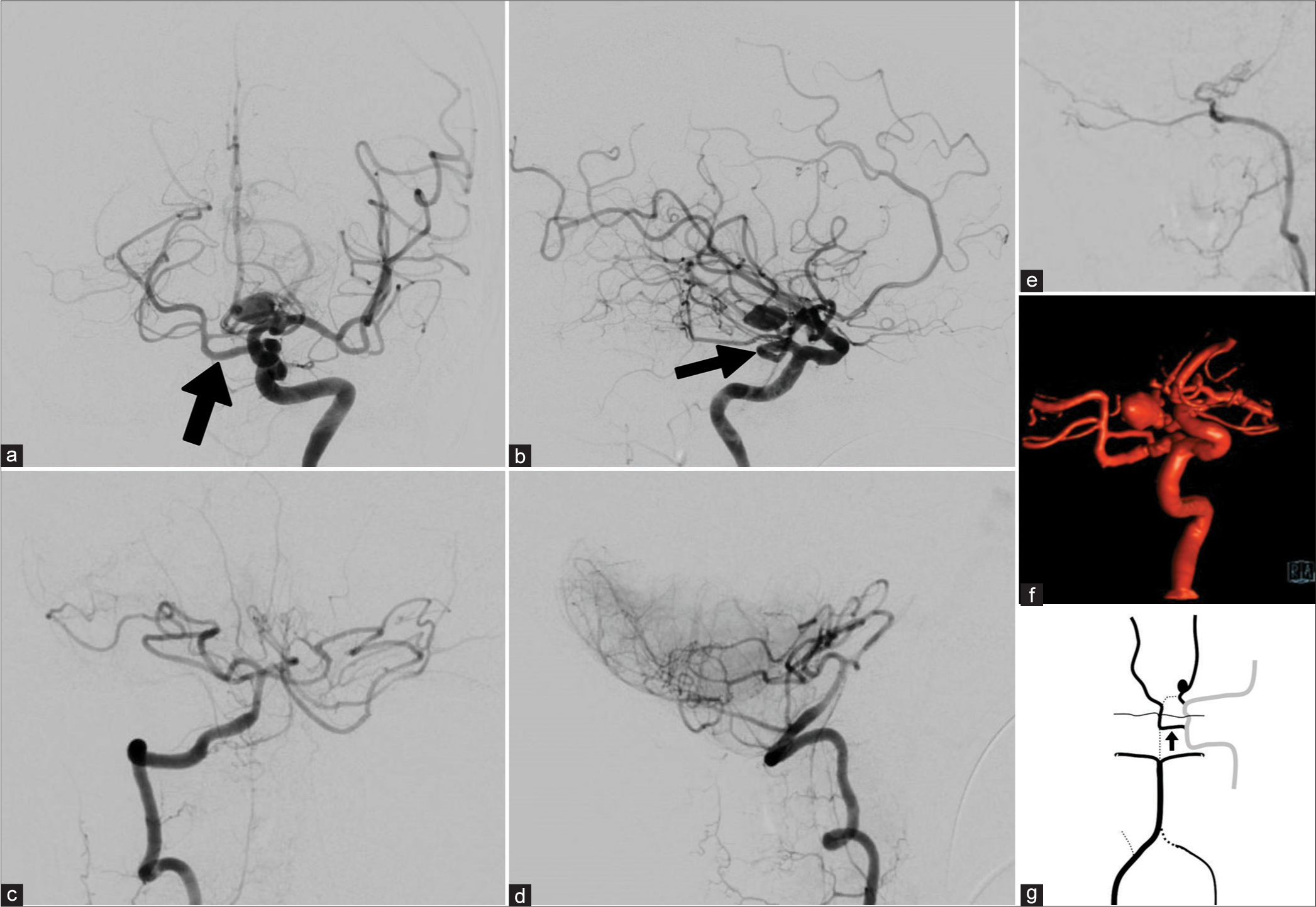
Figure 1:
(a) Anterior-Posterior (AP) left internal carotid artery (ICA) angiography demonstrates a persistent primitive trigeminal artery (PPTA) (black arrow) supplying the right posterior cerebral artery (PCA) and SCAs bilaterally. (b) Lateral left ICA angiography further demonstrates the PPTA (Black arrow) and a left P2 aneurysm. (c) AP right vertebral artery (VA) angiography demonstrates the proximal basilar trunk with anterior inferior cerebellar artery - posterior inferior cerebellar artery complexes bilaterally. (d) Lateral right VA angiography further demonstrates the blood supply to the caudal cerebellum. (e) Lateral left VA angiography demonstrates termination after the sulcus arteriosus as meningeal branches. (f) Reconstructed oblique left ICA 3-dimensional rotational angiography demonstrates a left fetal-type PCA giving rise to the P2 aneurysm. (g) Diagrammatic representation of the patient’s cerebrovascular system. Solid black lines represent blood vessels of the VB system while solid grey line represents the carotid circulation. Dotted black lines indicate a typical vessel that is absent. PPTA is indicated by black arrow.
DISCUSSION
Embryologic origins
In 1948, Dorcas Hager Padget described the stages of cerebrovascular embryologic development in her publication titled “The development of the cranial arteries in the human embryo.”[
Classifications
As neuroimaging capabilities developed, multiple PPTA subtypes have been identified and characterized. The earliest angiographic classification was documented by Saltzman in 1959.[
Weon et al. proposed a more comprehensive classification based on MRA studies in a large cohort of patients.[
Significance of basilar artery hypoplasia
In the case of vascular territory capture by a PPTA, less hemodynamic demand is placed on the BA proximal to the site of anastomosis. To this end, many PPTAs have been found in conjunction with basilar hypoplasia with a rate of approximately 42%.[
Association with cerebral aneurysms
A PPTA has been described in the context of several pathologies including cerebral aneurysms, carotid-cavernous fistulae, moyamoya disease, and trigeminal neuralgia among others. While early reports have cited a higher prevalence of cerebral aneurysms in patients with a PPTA, more recent literature has suggested this finding to be the result of selection bias.[
Relevance to present case
Within the scope of current classification schemes, the present case most closely resembles a combination of a Saltzman type one and two. This particular variant is now more accurately described as a Weon Type 3 PPTA. The frequency of severe basilar hypoplasia commonly seen in this subset of PPTA is illustrative of the functional importance of the anterior circulation. A completely atretic BA, however, has yet to be well documented in the literature. Although configurations of the larger and more functionally important posterior circulation arteries have been well-studied, this is not the case with other branches of the VB system.
As the functional contribution of the vertebral arteries and proximal BA decreases, an array of anatomic variations in the posterior circulation may be seen.[
CONCLUSION
The rarity of basilar segmentation is illustrative of the sequential stages of embryological development. As Hager Padget originally described, the regression of the primitive carotid-VB anastomoses occurs in an early embryonic stage before the stochastic capture of vascular territories by the posterior circulation. Our case demonstrates how a PPTA can provide robust hemodynamic competition leading to incomplete fusion of the BA. The combination of a fetal origin of the PCA, a PPTA, isolated bilateral AICA-PICA complexes demonstrates a four-way division of a standard VB arterial network. We therefore find an example of adult anatomy representing the development of cranial arteries in the human embryo.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ali S, Radaideh MM, Shaibani A, Russell EJ, Walker MT. Persistent trigeminal artery terminating in the posterior inferior cerebellar artery: Case report. Neurosurgery. 2008. 62: E746-8
2. Brzegowy K, Pękala PA, Zarzecki MP, Pekala JR, Roy J, Aziz HM. Prevalence and clinical implications of the primitive trigeminal artery and its variants: A meta-analysis. World Neurosurg. 2020. 133: e401-11
3. Cloft HJ, Razack N, Kallmes DF. Prevalence of cerebral aneurysms in patients with persistent primitive trigeminal artery. J Neurosurg. 1999. 90: 865-7
4. George AE, Lin JP, Morantz RA. Intracranial aneurysm on a persistent primitive trigeminal artery. Case report. J Neurosurg. 1971. 35: 601-4
5. Lasjaunias P, Berenstein A, Lasjaunias P, Berenstein A, editors. The internal maxillary system. Surgical Neuroangiography. New York: Springer-Verlag; 1987. p. 33-121
6. O’uchi E, O’uchi T. Persistent primitive trigeminal arteries (PTA) and its variant (PTAV): Analysis of 103 cases detected in 16,415 cases of MRA over 3 years. Neuroradiology. 2010. 52: 1111-9
7. Padget DH. The development of the cranial arteries in the human embryo. Contrib Embryol Carnegie Inst. 1948. 32: 205-62
8. Quain R. The anatomy of the arteries of the human body, with its applications to pathology and operative surgery, in lithographic drawings, with practical commentaries. Prov Med Surg J. 1840. 1: 203
9. Salas E, Ziyal IM, Sekhar LN, Wright DC. Persistent trigeminal artery: An anatomic study. Neurosurgery. 1998. 43: 557-61 discussion 561-2
10. Saltzman GF. Patent primitive trigeminal artery studied by cerebral angiography. Acta Radiol. 1959. 51: 329-36
11. Uchino A, Saito N, Okada Y, Kozawa E, Mizukoshi W, Inoue K. Persistent trigeminal artery and its variants on MR angiography. Surg Radiol Anat. 2012. 34: 271-6
12. Vasović L, Jovanović I, Ugrenović S, Vlajković S, Jovanović P, Stojanović V. Trigeminal artery: A review of normal and pathological features. Childs Nerv Syst. 2012. 28: 33-46
13. Weon YC, Choi SH, Hwang JC, Shin SH, Kwon WJ, Kang BS. Classification of persistent primitive trigeminal artery (PPTA): A reconsideration based on MRA. Acta Radiol. 2011. 52: 1043-51