- Department of Neurosurgery, Centro Hospitalar Lisboa Norte, Lisbon, Portugal
- Department of Pathology, Centro Hospitalar Lisboa Norte, Lisbon, Portugal
Correspondence Address:
Edson Oliveira
Department of Neurosurgery, Centro Hospitalar Lisboa Norte, Lisbon, Portugal
DOI:10.4103/2152-7806.194517
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Edson Oliveira, José Pedro Lavrador, Joaquim Teixeira, Alexandra Pignatelli, Sérgio Livraghi. A purely extradural lumbar nerve root cavernoma mimicking acute myeloid leukemia recurrence: Case report and literature review. 21-Nov-2016;7:
How to cite this URL: Edson Oliveira, José Pedro Lavrador, Joaquim Teixeira, Alexandra Pignatelli, Sérgio Livraghi. A purely extradural lumbar nerve root cavernoma mimicking acute myeloid leukemia recurrence: Case report and literature review. 21-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/a-purely-extradural-lumbar-nerve-root-cavernoma-mimicking-acute-myeloid-leukemia-recurrence-case-report-and-literature-review/
Abstract
Background:Myeloid sarcoma (MS) is a malignant tumor that usually occurs concomitantly with or following acute myeloid leukemia (AML). Cavernomas are benign congenital malformations that are unusual in the spine and exceedingly rare in pure extradural locations.
Case Description:We report a 73-year-old female with a previous medical history of AML in remission for 3 years who presented with symptoms of low back pain and right lower extremity radiculopathy. A magnetic resonance scan showed an extradural, foraminal lesion centered at the L2 level involving the right L2 nerve root. In view of the history of AML, this lesion was potentially considered MS, a form of AML relapse. Surgery consisting of a right L1 and L2 hemilaminectomy facilitated gross total resection of the purely extradural lesion the proved histologically to be a cavernoma.
Conclusion:In patients with a history of leukemia, MS must be considered in the differential diagnosis for any epidural or nerve root lesion that appears following treatment. Although rare, cavernomas must be considered among the differential diagnoses for epidural nerve root lesions in the setting of AML.
Keywords: Acute myeloid leukemia, extradural cavernoma, lumbar nerve root, lumbar spine, myeloid sarcoma
INTRODUCTION
Myeloid sarcoma (MS: Chloroma) is a malignant tumor caused by extramedullary proliferation of myeloblasts or immature myeloid cells.[
Cavernomas, benign vascular malformations/hemangiomas, usually arise from the vertebral bodies themselves, extending in an exophytic fashion into the extradural space.[
The real incidence of spinal cavernomas is unknown and in most series it represents 5% to 12% of spinal vascular abnormalities.[
The authors report a purely extradural right-sided L2 lumbar cavernoma presenting in a 73-year-old female with low back pain and right lower extremity radiculopathy. With a history of AML, the primary differential diagnosis was myeloid sarcoma (MS) rather than cavernoma. Following gross total cavernoma resection, the patient was cured.
CASE PRESENTATION
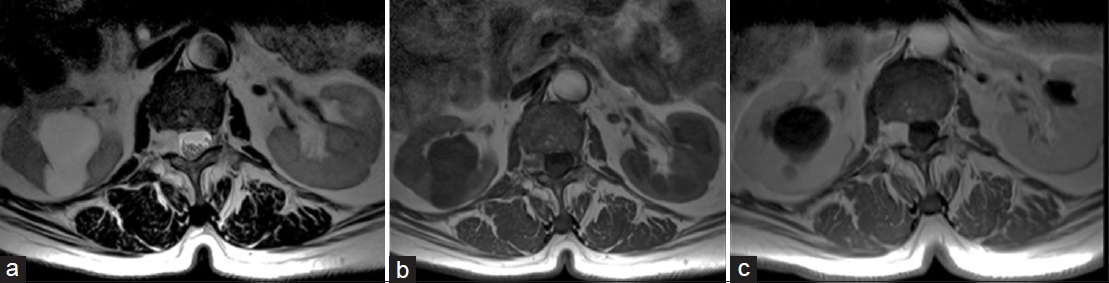
A 73-year-old female presented with several weeks of low back pain and a right L2 radiculopathy. Three years ago, she had AML that was now in remission. When the magnetic resonance imaging (MRI) showed an extradural, right-sided L2 foraminal lesion, the primary differential diagnosis was MS [
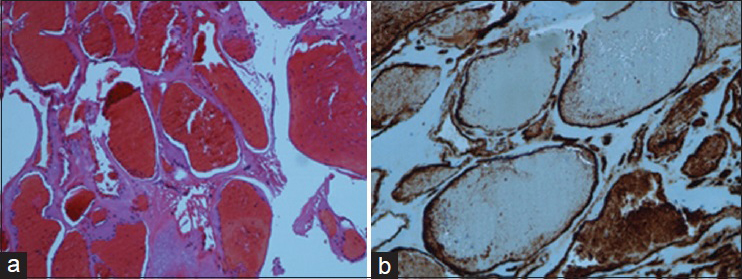
Surgery, consisting of a L1 and L2 right-sided hemilaminectomy revealed a brown, rubber lesion consistent with chronic blood involving the L2 nerve root and extending into the neural foramen (e.g., foramen of L2-L3). The lesion was completely removed with complete preservation of the L2 root. Histologically, the lesion proved to be a cavernoma. After 24 months of follow-up, the patient is asymptomatic and has no evidence of recurrence on control MRI.
DISCUSSION
Cavernomas are vascular lesions associated with recurrent hemorrhages, thrombosis, recanalization, tissue organization, and cyst formation; typically, they and do not regress spontaneously.[
In this case, the MRI showed a lesion involving the right L2 nerve root that was isointense in T1-weighted, hyperintense in T2-weighted with strong homogeneous contrast enhancement; there was no clear evidence of intralesional hemorrhage or ring enhancement.
Purely extradural cavernomas in direct contact with nerve roots are exceedingly rare. For the reported cases, all were isointense on T1 and hyperintense on T2 studies, while similarly demonstrating homogenous contrast enhancement;[
Histologically, cavernomas show irregularly dilated blood vessels lined by flat endothelium and with walls of varying thickness. CD34 immunostaining highlighted endothelial cells [
CONCLUSION
The authors described an extradural L2 lumbar nerve root cavernoma that occurred in a 73-year-old female 3 years following treatment (in remission) for AML. Rather than being an anticipated AML-related MS, it proved to be a benign cavernoma that was successfully excised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Appiah CA, Knuckley NW, Robbins PD. Extradural spinal cavernous hemangioma: Case report and review of the literature. J Clin Neurosci. 2001. 8: 176-9
2. Alexandros D, Heinz-Hermann H, Harald B, Hubertus M. A rare case of extradural lumbar root cavernoma. Eur Spine J. 2011. 20: S348-9
3. Carlier R, Engerand S, Lamer S, Vallee C, Bussel B, Polivka M. Foraminal epidural extra osseous cavernous hemangioma of the cervical spine. Spine. 2000. 25: 629-31
4. Caruso G, Galarza M, Borghesi I, Pozzati E, Vitale M. Acute presentation of spinal epidural cavernous angiomas: Case report. Neurosurgery. 2007. 60: E575-6
5. Khalatbari M, Abbassioun K, Amirjmsshidi A. Solitary spinal epidural cavernous angioma: Report of nine surgically treated cases and review of the literature. Eur Spine J. 2013. 22: 542-7
6. Kivelev J, Niemela M, Hernesniemi J. Outcome after microsurgery in 14 patients with spinal cavernomas and review of the literature. J Neurosurg Spine. 2010. 13: 524-34
7. Santoro A, Piccirilli M, Bristot R, di Norcia V, Salvati M, Delfini R. Extradural spinal cavernous angiomas: Report of seven cases. Neurosurg Ver. 2005. 28: 313-9
8. Smith TR, Slimac N, McClendon J, Fessller RG. Low back pain and lumbar radiculopathy as harbingers of acute myeloid leukemia recurrence in a patient with myeloid sarcoma. J Clin Neurosci. 2012. 19: 1140-1