- Department of Neurosurgery, National Institute of Neurology and Neurosurgery, Mexico City, Mexico.
Correspondence Address:
Marcos V. Sangrador-Deitos, Department of Neurosurgery, National Institute of Neurology and Neurosurgery, Mexico City, Mexico.
DOI:10.25259/SNI_473_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jorge Armando Lara-Olivas, Marcos V. Sangrador-Deitos, Rodolfo Villalobos-Díaz, Ricardo Marian-Magaña, Juan Luis Gomez-Amador. A rare case of a right infratentorial meningioma and a left giant posterior communicating thrombosed aneurysm. 08-Sep-2023;14:317
How to cite this URL: Jorge Armando Lara-Olivas, Marcos V. Sangrador-Deitos, Rodolfo Villalobos-Díaz, Ricardo Marian-Magaña, Juan Luis Gomez-Amador. A rare case of a right infratentorial meningioma and a left giant posterior communicating thrombosed aneurysm. 08-Sep-2023;14:317. Available from: https://surgicalneurologyint.com/surgicalint-articles/12540/
Abstract
Background: Giant intracranial aneurysms cause symptoms due to mass effect and can mimic other lesions in imaging studies. The coexistence of tumors and aneurysms is relatively rare, with meningiomas being the predominant tumors found in such cases. The relationship between these two entities is complex and represent a neurosurgical challenge.
Case Description: A 61-year-old woman presented with intermittent headache, vertigo, right peripheral facial palsy, hearing loss, and left hemiparesis. Magnetic resonance imaging revealed two lesions: a supratentorial paraclinoid lesion in the left frontotemporal region and a right infratentorial extra-axial mass, suggestive of a meningioma. The patient underwent a two-staged surgical intervention to address both lesions.
Conclusion: In this particular case, the lesions were located on different sides and in different cranial compartments, making it even rarer.
Keywords: Aneurysm, Concomitant, Giant, Meningioma
INTRODUCTION
The co-occurrence of tumors and aneurysms has been documented with an incidence rate of 0.7 to 7.0%. Meningiomas are the predominant tumors found in such cases.[
CASE REPORT
A 61-year-old woman presented with an 8-month history of intermittent headache, vertigo, right peripheral facial palsy, and left hemiparesis. Neurologic examination revealed right sensorineural hearing loss. Magnetic resonance imaging (MRI) revealed two lesions: a supratentorial paraclinoid lesion that occupied the left frontotemporal region and a right infratentorial solid extra axial mass, suggestive of a tentorial meningioma [
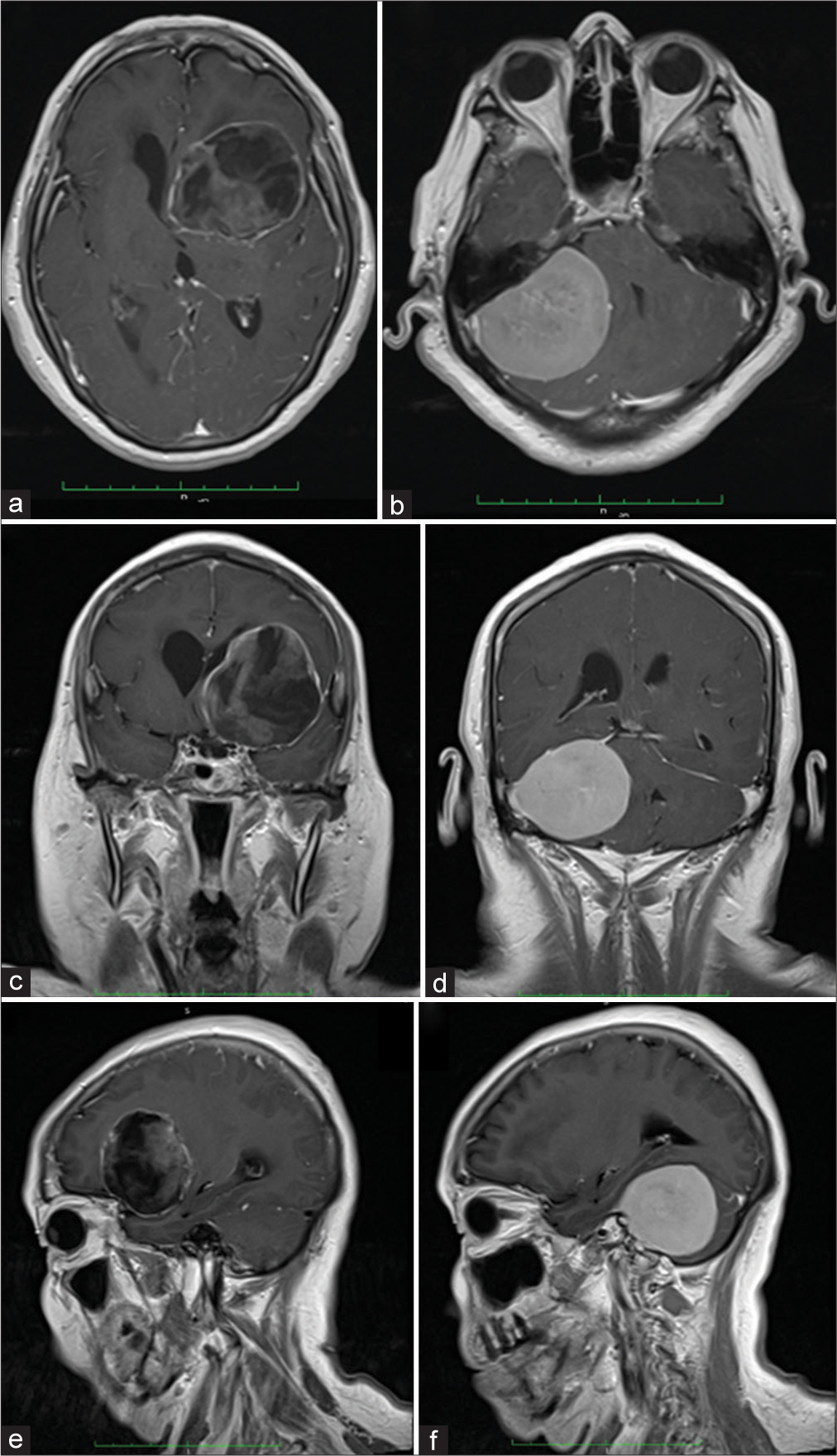
Figure 1:
T1 weighted image with contrast magnetic resonance imaging (MRI) (a) axial, (b) coronal, and (c) sagittal planes revealed a left sided frontal mass, with a heterogeneously enhancing central content along with a peripherally enhancing component. The lesion measured 48 × 60 × 55 mm in the rostro-caudal, dorso-ventral, and latero-lateral directions, respectively, and seems to be external to the brain parenchyma. It extends upward into the left lateral ventricle, exerting mass effect, and displacing it medially. The heterogeneously enhancing center is compatible with a flow void sign, which, when associated with an internal enhancement, is suggestive of partial lumen patency, in the context of a giant internal carotid artery (ICA) aneurysm. The peripheral enhancement is consistent with the aneurysmatic arterial wall. (d) Axial, (e) coronal, and (f) sagittal planes revealed a right sided, homogeneously enhancing solid extra axial mass, suggestive of a meningioma, arising from the lateral outer tentorial ring and extending downward to the infratentorial space and medially indenting the pons and right.
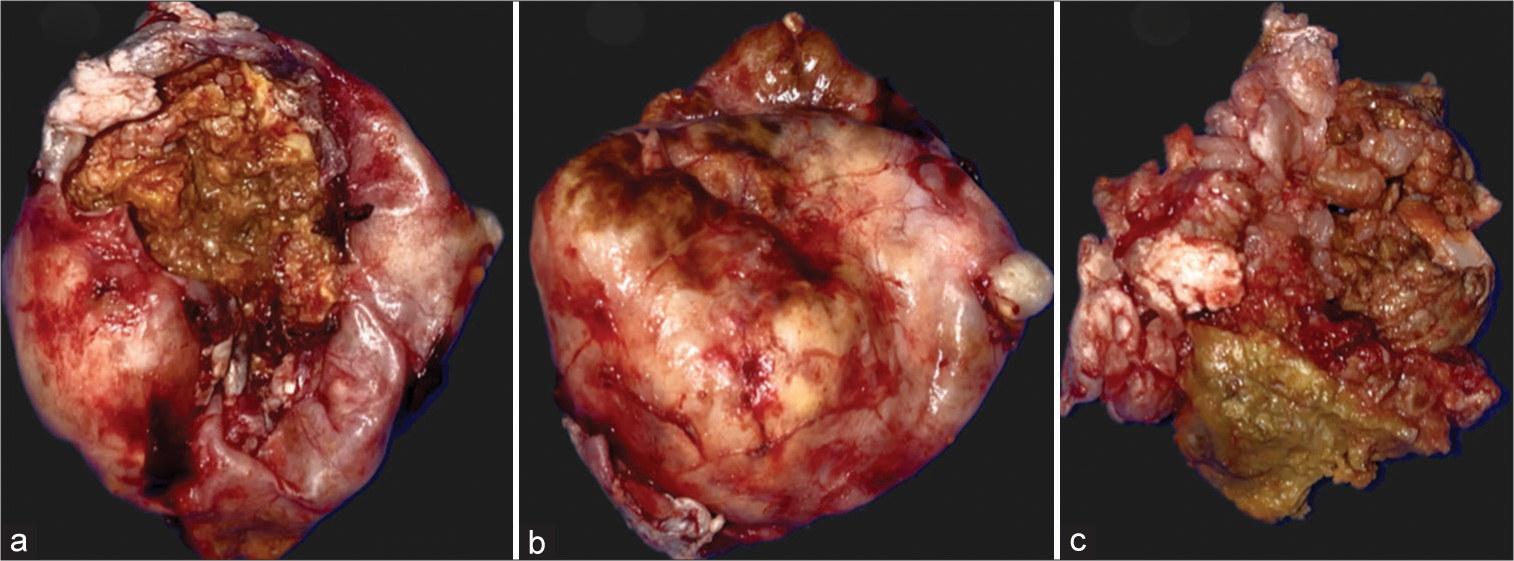
Figure 2:
Macroscopic findings. (a-c) An ovoid, extra-axial lesion was found with an adequate dissection plane firmly adhered to blood vessels at the level of the operculoinsular region of the Sylvian fissure. The lesion capsule was opened to access the contents, revealing solid, yellowish material suggestive of cholesterol deposits. Zones of old bleeding were found peripherally to the lesion. During the dissection of the peripheral blood vessel capsule, a solution of continuity of the left internal carotid artery communicating segment occurred, which was suggestive of an aneurysmal neck at that level. The resected lesion was suggestive of a thrombosed giant aneurysm, which ruptured the aneurysmal neck during dissection, despite being repaired with suture there was a high risk of thrombosis and/or extensive cerebral infarction.
Meningiomas are common and mostly benign tumors arising from the arachnoid cap cells, they represent 15% of all intracranial tumors and are more prevalent in aging women.[
The giant posterior communicating aneurysm was initially misdiagnosed as a cavernoma due to its popcorn-like appearance and a low-signal intensity rim on MRI. However, various substances such as methemoglobin, melanin, lipid, protein, calcium, iron, copper, and manganese can cause intrinsically high-signal intensity on T1 weighted image (T1WI).[
CONCLUSION
The etiology of coexisting meningiomas and intracranial aneurysms has been the subject of intensive investigation in which various hypotheses suggest that the enhanced regional blood flow resulting from the meningioma may promote aneurysm formation on the feeding artery, as the increased blood supply to the tumor leads to an augmented directional blood flow that generates hemodynamic stress on the cerebral arterial walls. Moreover, the pathogenesis of aneurysm formation may involve the action of signaling molecules secreted by the tumor, such as vascular endothelial growth factor and growth hormone-like estrogen.[
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Algburi HA, Sharma M, Ismail M, Albulaihed SA, AlGertani MR, Majeed SN. The coexistence of anterior communicating artery aneurysm and meningioma: A literature review and illustrative case. Surg Neurol Int. 2022. 13: 569
2. Barrows HS, Harter DH. Tentorial meningiomas. J Neurol Neurosurg Psychiatry. 1962. 25: 40-4
3. Belec L, Cesaro P, Brugieres P, Gray F. Tumor-simulating giant serpentine aneurysm of the posterior cerebral artery. Surg Neurol. 1988. 29: 210-5
4. Bose B, Northrup B, Osterholm J. Giant basilar artery aneurysm presenting as a third ventricular tumor. Neurosurgery. 1983. 13: 699-702
5. Colli BO, Assirati JA, Deriggi DJ, Neder L, Dos Santos AC, Carlotti CG. Tentorial meningiomas: Follow-up review. Neurosurg Rev. 2008. 31: 421-30 discussion 430
6. De Souza MR, Fagundes CF, Rabelo NN, Teixeira MJ, Figueiredo EG. Association between intracranial aneurysm and meningiomas: An integrative survival analysis with identification of prognostic factors. Clin Neurol Neurosurg. 2020. 198: 106128
7. Fischer BR, Palkovic S, Holling M, Niederstadt T, Jeibmann A, Wassmann H. Coexistence of cerebral aneurysm and meningioma--pure accident?. Clin Neurol Neurosurg. 2009. 111: 647-54
8. Ginat DT, Meyers SP. Intracranial lesions with high signal intensity on T1-weighted MR images: Differential diagnosis. Radiographics. 2012. 32: 499-516
9. Kim YH, Lee YJ, Han JH, Ahn S, Lee J, Kim JH. Association of intracranial aneurysms and meningiomas: A case-control study. J Neurosurg. 2015. 123: 357-61
10. Marosi C, Hassler M, Roessler K, Reni M, Sant M, Mazza E. Meningioma. Crit Rev Oncol Hematol. 2008. 67: 153-71
11. Pia HW, Obrador S, Martin JG. Association of brain tumours and arterial intracranial aneurysms. Acta Neurochir (Wien). 1972. 27: 189-204
12. Ploncard P. Differential diagnosis for posterior cerebral fossa meningiomas. Neurochirurgie. 1972. 18: 57-64
13. Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957. 20: 22-39
14. Smith KA, Kraus GE, Johnson BA, Spetzler RF. Giant posterior communicating artery aneurysm presenting as third ventricle mass with obstructive hydrocephalus: Case report. J Neurosurg. 1994. 81: 299-303
15. Tachikawa T, Adachi J, Nishikawa R, Matsutani M. An anterior ethmoidal artery aneurysm associated with an olfactory groove meningioma: Case illustration. J Neurosurg. 2002. 97: 1479
16. Yun TJ, Na DG, Kwon BJ, Rho HG, Park SH, Suh YL. A T1 hyperintense perilesional signal aids in the differentiation of a cavernous angioma from other hemorrhagic masses. AJNR Am J Neuroradiol. 2008. 29: 494-500