- Department of Neurosurgery, Ehime University School of Medicine, Toon, Ehime, Japan.
DOI:10.25259/SNI_437_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Seiji Shigekawa, Akihiro Inoue, Yawara Nakamura, Daisuke Kohno, Masahiko Tagawa, Takeharu Kunieda. A rare case of spinal dural arteriovenous fistula mimicking malignant glioma of the medulla oblongata: Significance of cerebral angiography for accurate diagnosis of brain stem region. 12-Sep-2020;11:287
How to cite this URL: Seiji Shigekawa, Akihiro Inoue, Yawara Nakamura, Daisuke Kohno, Masahiko Tagawa, Takeharu Kunieda. A rare case of spinal dural arteriovenous fistula mimicking malignant glioma of the medulla oblongata: Significance of cerebral angiography for accurate diagnosis of brain stem region. 12-Sep-2020;11:287. Available from: https://surgicalneurologyint.com/surgicalint-articles/10253/
Abstract
Background: The findings of a hyperintense sign on T2-weighted imaging (T2-WI) and gadolinium (Gd) contrast enhancement on magnetic resonance imaging (MRI) of the brain stem suggest malignant glioma. However, this pathological condition is probably uncommon, and it may be unknown that a dural arteriovenous fistula (DAVF) can imitate this radiological pattern. In addition, it is extremely rare to be caused by a spinal DAVF. Here, a rare case of spinal DAVF that mimicked malignant glioma of the medulla oblongata is presented.
Case Description: A 56-year-old woman was admitted with a progressive gait disturbance, vertigo, and dysphasia. MRI showed a hyperintense signal in the medulla oblongata on fluid-attenuated inversion recovery (FLAIR) and moderate contrast enhancement on Gd-enhanced MRI. Interestingly, Gd-enhanced MRI demonstrated abnormal dilated veins around the brain stem and cervical spinal cord. Cerebral angiography showed spinal DAVF at the left C4/C5 vertebral foramen fed by the C5 radicular artery. The fistula drained into spinal perimedullary veins and flowed out retrograde at the cortical vein of the posterior cranial fossa. Therefore, surgical disconnection of the spinal DAVF was performed by a posterior approach. The patient’s postoperative course was uneventful. Cerebral angiography showed complete disappearance of the DAVF, with marked reductions of the hyperintense sign of the medulla oblongata on FLAIR.
Conclusion: This important case illustrates MRI findings mimicking brain stem glioma. In cases with the hyperintense sign-on T2-WI associated with contrast enhancement suspicious of brainstem glioma, careful checking for perimedullary abnormal vessels and additional cerebral angiography should be performed.
Keywords: Cerebral angiography, Lower cranial nerve palsy, Mimicking medulla oblongata glioma, Spinal dural arteriovenous fistula, Venous congestion
INTRODUCTION
Accurate diagnosis of the brain stem or cervical spinal cord lesions is very difficult on routine magnetic resonance imaging (MRI).[
CASE DESCRIPTION
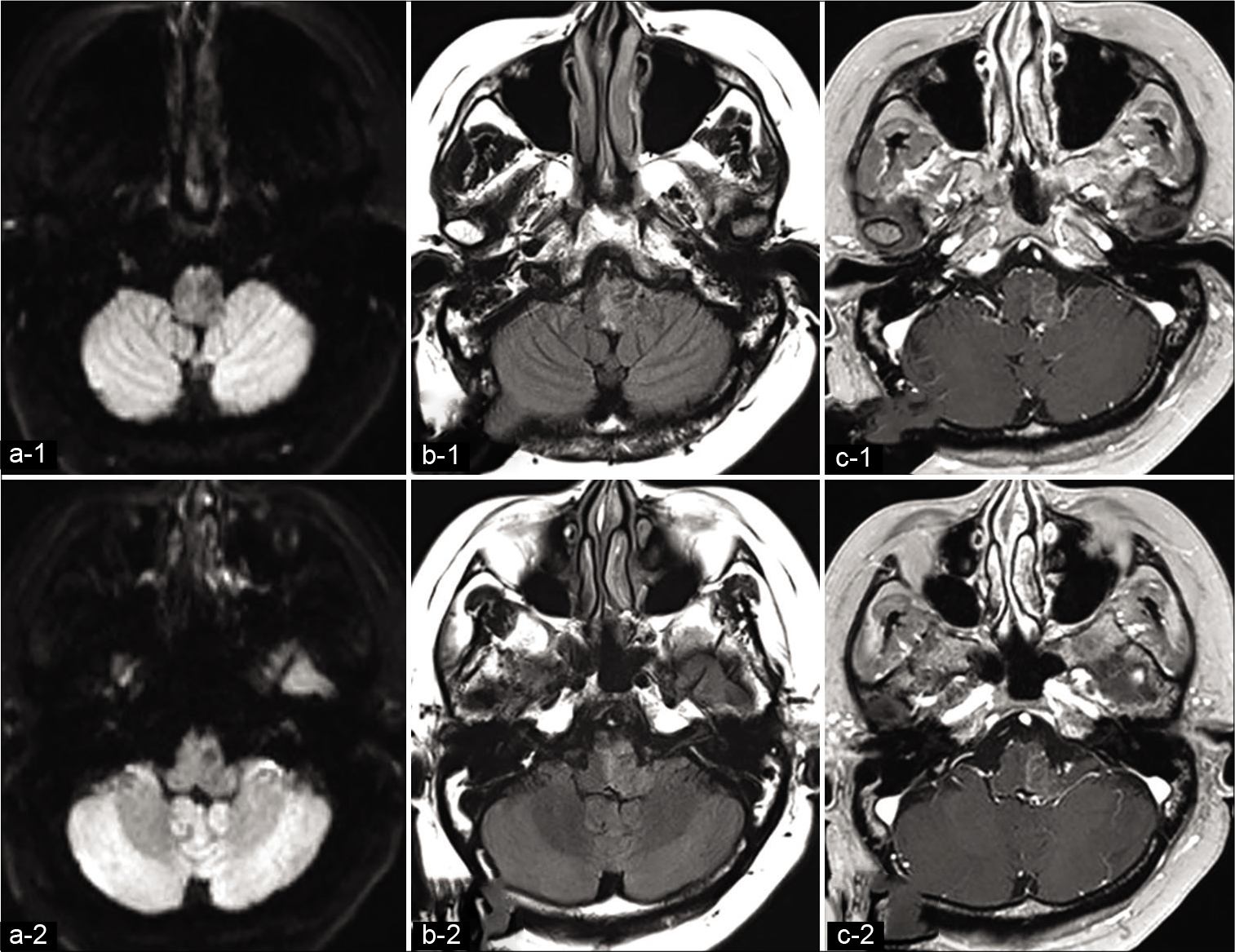
A 56-year-old woman with a 2-month history of nausea and progressive gait disturbance visited our department after experiencing gradual worsening of swallowing difficulty over a 2-week period. On admission, she complained of severe nausea and truncal ataxia, and she had left glossopharyngeal and vagal nerve palsies. MRI of the brain showed hypointensity on diffusion-weighted imaging (DWI) and hyperintensity on fluid-attenuated inversion recovery (FLAIR) of the medulla oblongata and cerebellar peduncle. Gadolinium (Gd) administration showed moderate enhancement mainly within the medulla oblongata [
Figure 1:
Preoperative axial magnetic resonance imaging. (a) Diffusion-weighted image (DWI), (b) fluid attenuated inversion recovery (FLAIR), and (c) gadolinium (Gd)-enhanced T1-weighted images showing a lesion in the medulla oblongata. The lesion is hypointense on DWI hyperintense on FLAIR and shows moderate enhancement on Gd administration.
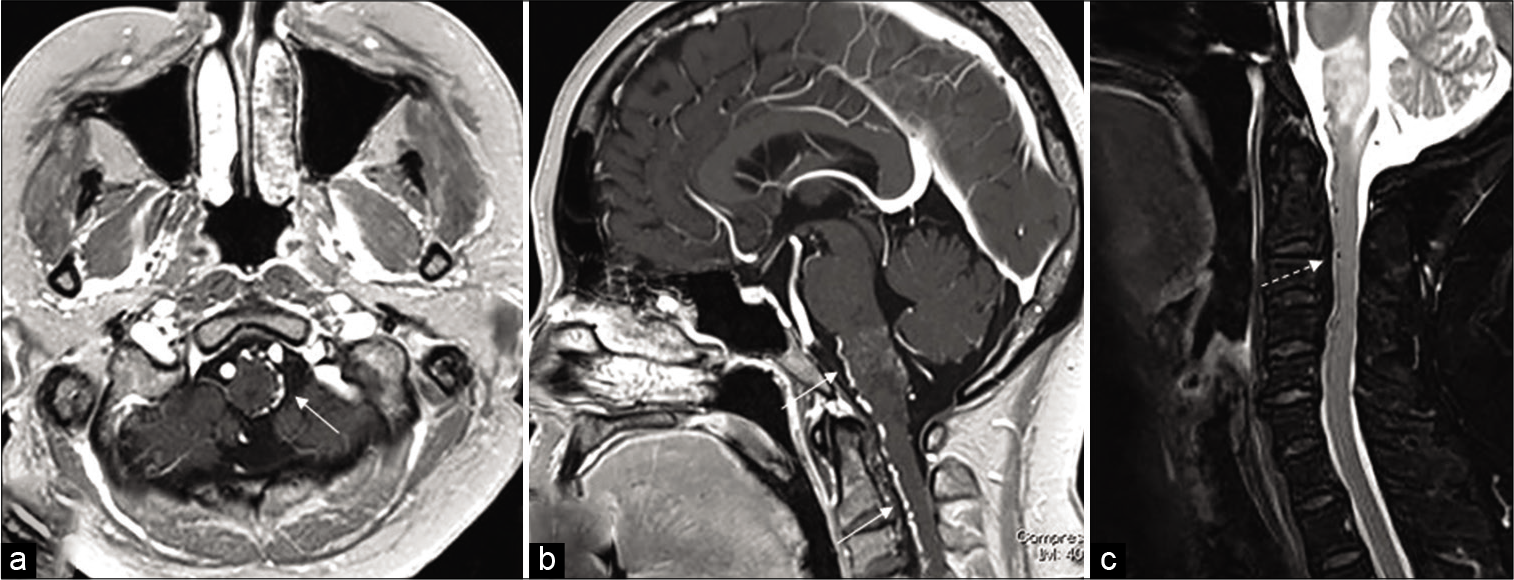
Figure 2:
Gadolinium (Gd)-enhanced T1-weighted MRI (a: axial and b: sagittal) clearly showing abnormal dilated veins around the brain stem and in front of the cervical spinal cord (white arrow). T2-weighted sagittal image showing hyperintensity of the medulla and an abnormal signal flow void extending to the cervical portion of the spinal cord (white dashed arrow) (c).
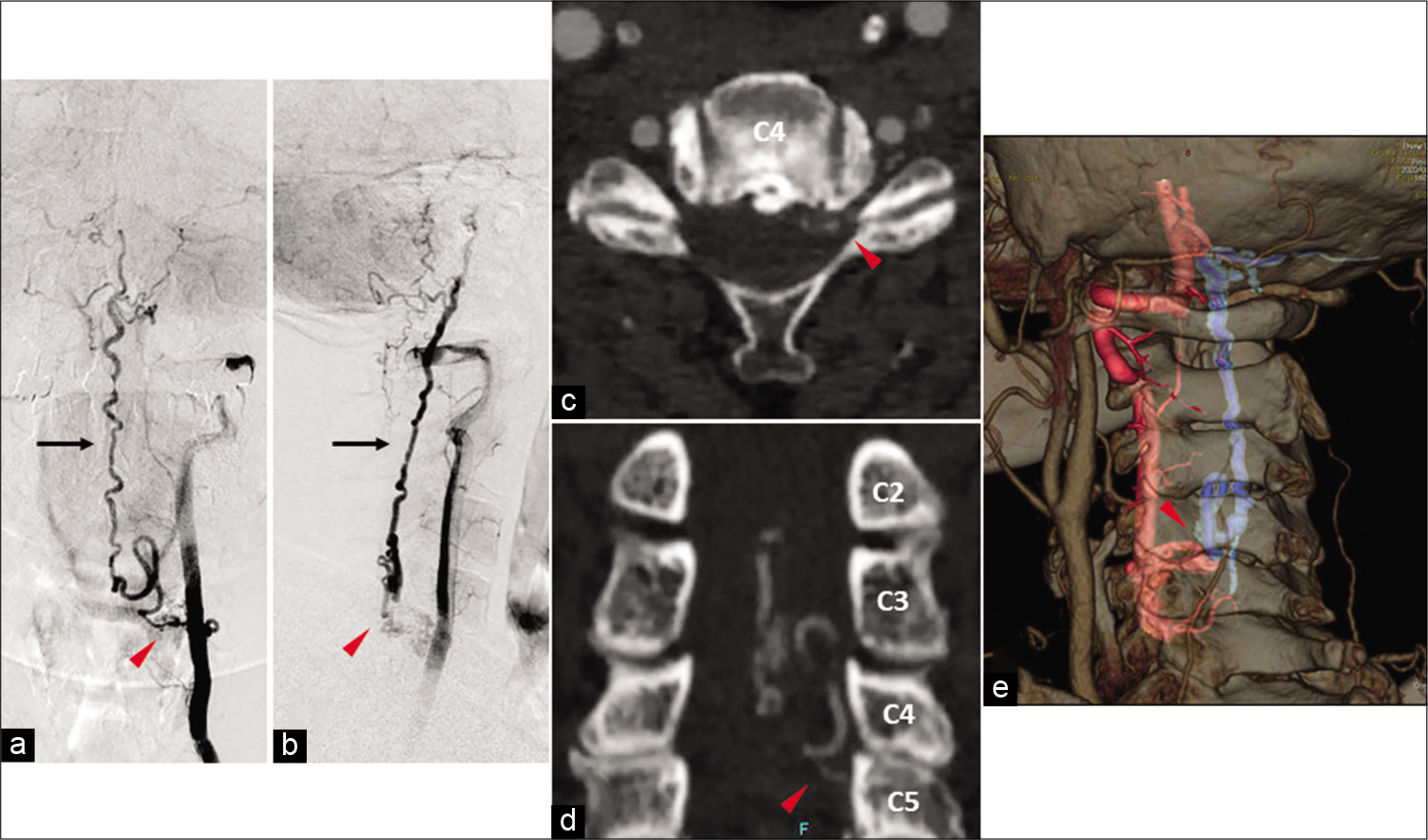
Figure 3:
Left vertebral artery angiographic findings. (a) Anteroposterior view and (b) lateral view showing a spinal dural arteriovenous fistula (red arrowhead) supplied by the C5 radicular artery arising from the left vertebral artery draining into the spinal perimedullary veins (black bald arrow) reaching the cortical vein localized along the left aspect of the medulla oblongata. Computed tomography three-dimensional fusion digital subtraction angiography demonstrating the exact location of the arterio-venous shunt point (red arrowhead). (c) Axial view, (d) coronal view, and (e) reconstruction fusion model (red blood vessels are arteries and blue are draining veins)
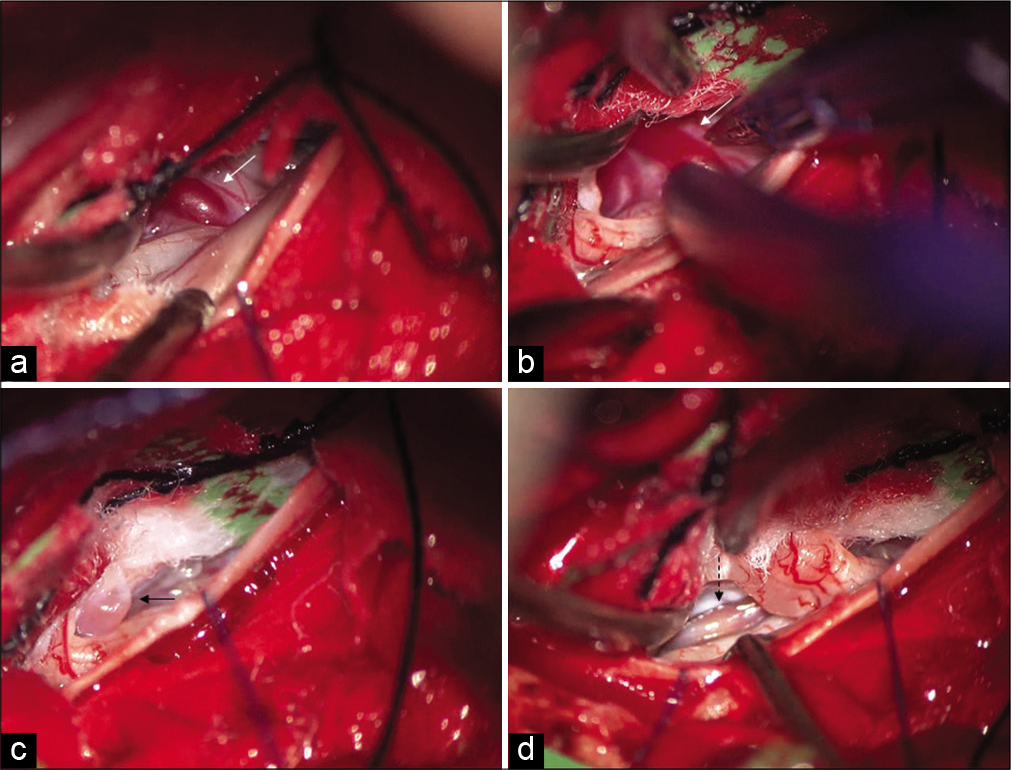
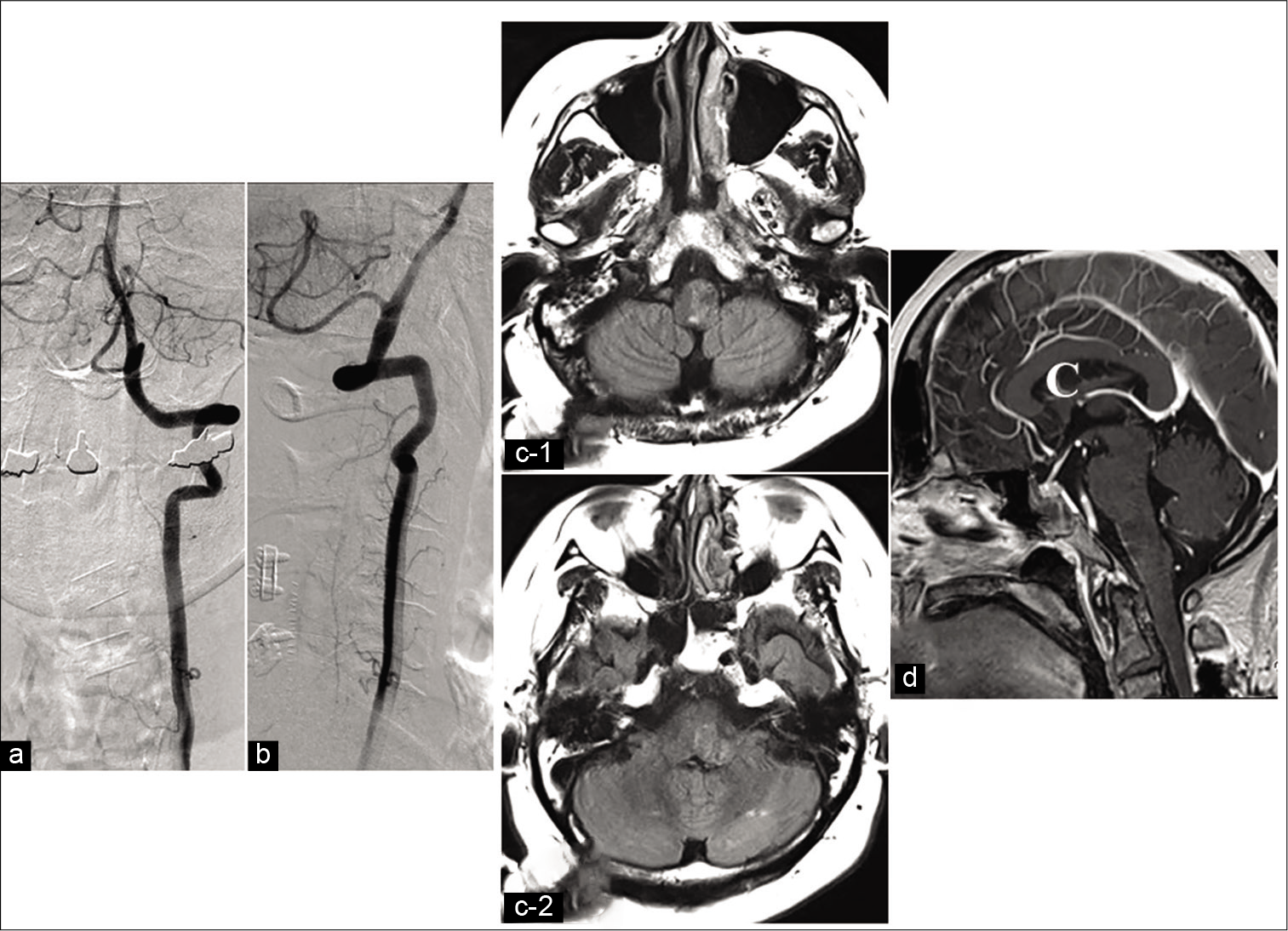
Figure 4:
Intraoperative views (opening of the dura mater, left side), showing the shunt location and the single draining vein (white arrow) (a and b), which is disconnected with bipolar coagulation (black arrow: disconnected vein) (c). The draining vein is degenerated with shunt disconnection (black dashed arrow) (d).
Figure 5:
Left vertebral artery angiographic findings. (a) Anteroposterior view and (b) lateral view demonstrating complete disappearance of the dural arteriovenous fistula. Postoperative MRI shows marked reductions of the hyperintense sign of the medulla oblongata on fluid- attenuated inversion recovery (c) and the disappearance of the atypical perimedullary vein on gadolinium-enhanced T1-WI (d).
The clinical study of the above-mentioned case report was approved by the Ethics Committee for Clinical Research of Ehime University Hospital, and informed consent was obtained from the patient before initiating the study.
DISCUSSION
The precise diagnosis of the brain stem and cervical cord lesions is often difficult in the field of neurosurgery.[
It is commonly accepted that a hyperintense sign-on T2-WI or FLAIR and T1 contrast enhancement of Gd on MRI of the brain stem and cervical cord is mainly related to malignant gliomas.[
Making the diagnosis of spinal or intracranial DAVF can be very difficult because the usual MRI protocol can miss an abnormal dilated vessel, and because its appearance can mimic that of a neoplasm at its initial presentation.[
DAVFs.[
In the previous reports, intracranial DAVF in the posterior cranial fossa has often been reported as the cause of signal changes on T2-WI and of Gd enhancement in this part.[
CONCLUSION
A rare case of spinal DAVF identified by recognizing venous congestion of the medulla oblongata mimicking a malignant glial tumor was presented. This is an extremely important case report that describes MRI findings mimicking brain stem glioma. In cases with the hyperintense sign-on T2-WI associated with contrast enhancement suspicious of brainstem glioma, a careful check for perimedullary abnormal vessel dilatation and additional cerebral angiography should be mandatory.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Batista MN, Barreto MM, Cavaguti RF, Zanetti G, Marchiori E. Pulmonary artery sarcoma mimicking chronic pulmonary thromboembolism. Radiol Bras. 2015. 4: 333-4
2. Bernard F, Lemée JM, Faguer R, Fournier HD. Lessons to be remembered from a dural arteriovenous fistula mimicking medulla and high cervical cord glioma. World Neurosurg. 2018. 113: 312-5
3. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A. Cerebral dural arteriovenous fistulas: Clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995. 194: 671-80
4. Guzmán-De-Villoria JA, Ferreiro-Argüelles C, Fernández-García P. Differential diagnosis of T2 hyperintense brainstem lesions: Part 2. Diffuse lesions. Semin Ultrasound CT MR. 2010. 31: 260-74
5. Haryu S, Endo T, Sato K, Inoue T, Takahashi A, Tominaga T. Cognard type V intracranial dural arteriovenous shunt: Case reports and literature review with special consideration of the pattern of spinal venous drainage. Neurosurgery. 2014. 74: E135-42
6. Le Guennec L, Leclercq D, Szatmary Z, Idbaih A, Reyes-Botero G, Delattre JY. Dural arteriovenous fistula mimicking a brainstem glioma. J Neuroimaging. 2015. 25: 1053-5
7. Roelz R, van Velthoven V, Reinacher P, Coenen VA, Mader I, Urbach H. Unilateral contrast-enhancing pontomedullary lesion due to an intracranial dural arteriovenous fistula with perimedullary spinal venous drainage: The exception that proves the rule. J Neurosurg. 2015. 123: 1534-9
8. Satoh M, Kuriyama M, Fujiwara T, Tokunaga K, Sugiu K. Brain stem ischemia from intracranial dural arteriovenous fistula: Case report. Surg Neurol. 2005. 64: 341-5
9. Uchino A, Kato A, Kuroda Y, Shimokawa S, Kudo S. Pontine venous congestion caused by dural carotid-cavernous fistula: Report of two cases. Eur Radiol. 1997. 7: 405-8
10. Wu Q, Wang HD, Shin YS, Zhang X. Brainstem congestion due to dural ateriovenous fistula at the craniocervical junction. J Korean Neurosurg Soc. 2014. 55: 152-5