- Department of Neurosurgery and Ear, Nose and Throat Diseases, Division of Neurosurgery, Medical University of Varna, Varna, Bulgaria.
Correspondence Address:
Mustafa Ali, Department of Neurosurgery and Ear, Nose and Throat Diseases, Division of Neurosurgery, Medical University of Varna, Varna, Bulgaria.
DOI:10.25259/SNI_762_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mustafa Ali, Yavor Enchev. A rare cause of low back pain in adolescence – Bertolotti syndrome: A case report. 27-Oct-2023;14:383
How to cite this URL: Mustafa Ali, Yavor Enchev. A rare cause of low back pain in adolescence – Bertolotti syndrome: A case report. 27-Oct-2023;14:383. Available from: https://surgicalneurologyint.com/surgicalint-articles/12611/
Abstract
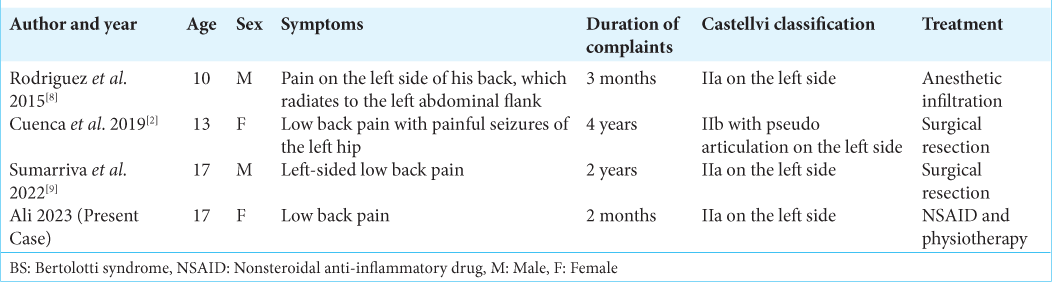
Background: Bertolotti syndrome (BS) is defined as a congenital anomaly of the spine that includes sacralization of the lowest lumbar vertebra or lumbarization of the first sacral vertebra (i.e., lumbosacral transitional vertebra- LSTV) and the pain associated with this condition. The incidence of BS in adolescence is rare; we found only three such case reports of patients under the age of 18 in the literature, here will add a fourth.
Case Description: A 17-year-old female presented with a 2-month history of low back pain exacerbated by physical activity. Her neurological examination was normal, except for pain elicited when applying pressure over the sacroiliac joints bilaterally, and over the spinous process of the L5 vertebra. The computed tomography scan documented BS: (i.e., LSTV – Castellvi classification: Type IIa on the left side). She was successfully treated with nonsteroidal anti-inflammatory drugs (NSAIDs) alone.
Conclusion: Here, we report a 17-year-old female who was symptomatic from BS and was successfully treated with NSAIDs.
Keywords: Bertolotti syndrome, Low back pain, Lumbarization, Lumbosacral transitional vertebra, Sacralization
INTRODUCTION
Bertolotti syndrome (BS) is defined as a congenital anomaly of the distal lumbar spine; specifically, sacralization of L5 vertebra or lumbarization of S1 vertebra (i.e., lumbosacral transitional vertebra – LSTV) and the pain associated with LSTV.[
CASE REPORT
A 17-year-old female presented with a 2-month history of low back pain (LBP) exacerbated with activity. Her only finding on the neurological examination was focal pain over the sacroiliac joints bilaterally and over the spinous process of the L5 vertebra. The CT demonstrated findings consistent with the diagnosis of BS: a pseudoarticulation on the left between the TP of the L5 vertebra, sacral ala, and ilium (i.e., Castellvi classification: Type IIa [
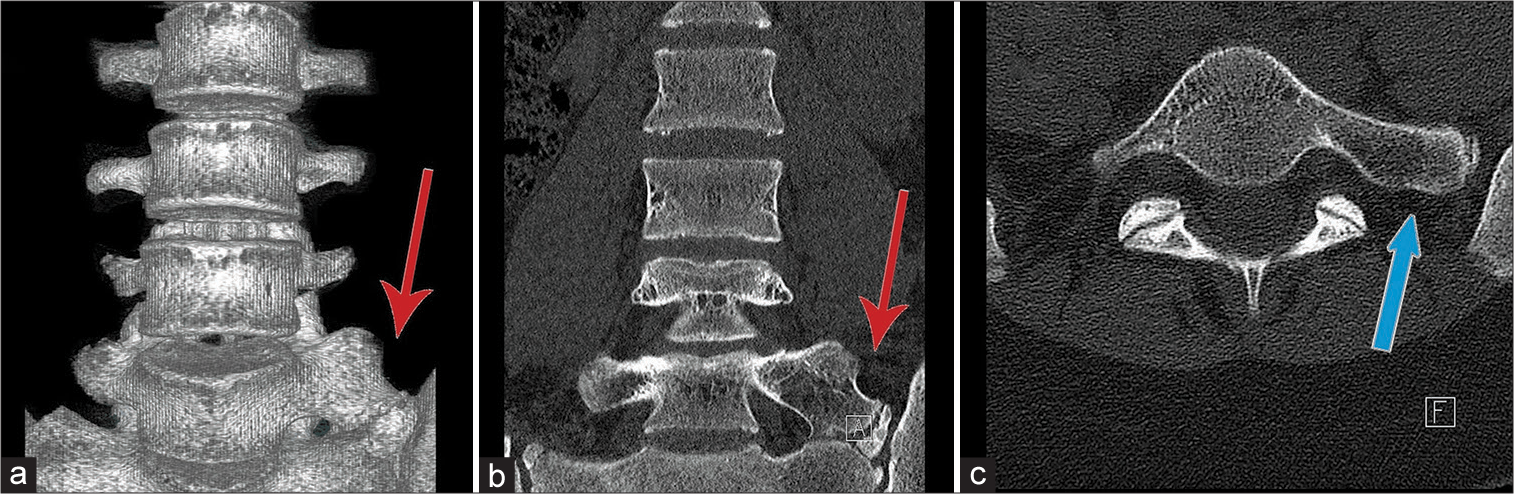
Figure 1:
(a and b) Three-dimensional reconstruction and coronal plane of the computed tomography (CT) scan demonstrates the pseudoarticulation on the left side between the transverse process (TP) of the L5 vertebra, sacral ala, and ilium (red arrow). (c) Axial CT scan demonstrates the enlarged TP (blue arrow).
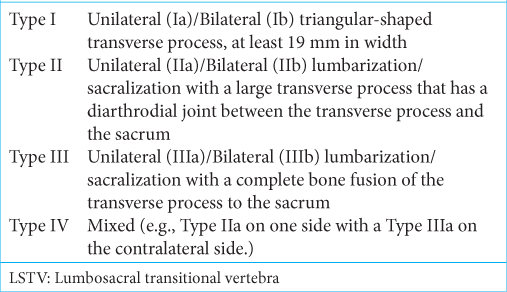
Table 1:
Castellvi et al. LSTV classification.[
DISCUSSION
Pain is seen with BS
Pain in BS may be due to disc, spinal canal, and posterior element pathology; degeneration of abnormous articulation between LSTV and sacrum; extraforaminal stenosis; and facet joint arthrosis.[
Radiological diagnosis of BS
The CT scan in this case was diagnostic for Castellvi classification: Type IIa LSTV/BS on the left side. [
Treatment of BS: Conservative
Treatment options for BS typically include physical therapy, NSAIDS, and rarely, surgery.[
Surgery
Surgical options include decompression, resection, and/ or fusion.[
CONCLUSION
BS must be considered a differential diagnosis in patients with LBP, including those in the adolescent age group. Notably, NSAIDs and conservative management should be the predominant management strategy.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976). 1984. 9: 493-5
2. Cuenca C, Bataille J, Ghouilem M, Ballouhey Q, Fourcade L, Marcheix PS. Bertolotti’s syndrome in children: From low-back pain to surgery. A case report. Neurochirurgie. 2019. 65: 421-4
3. Jancuska JM, Spivak JM, Bendo JA. A review of symptomatic lumbosacral transitional vertebrae: Bertolotti’s syndrome. Int J Spine Surg. 2015. 9: 42
4. Konin GP, Walz DM. Lumbosacral transitional vertebrae: Classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol. 2010. 31: 1778-86
5. Matson DM, Maccormick LM, Sembrano JN, Polly DW. Sacral dysmorphism and lumbosacral transitional vertebrae (LSTV) review. Int J Spine Surg. 2020. 14: 14-9
6. McGrath K, Schmidt E, Rabah N, Abubakr M, Steinmetz M. Clinical assessment and management of Bertolotti syndrome: A review of the literature. Spine J. 2021. 21: 1286-96
7. Quinlan JF, Duke D, Eustace S. Bertolotti’s syndrome. A cause of back pain in young people. J Bone Joint Surg Br. 2006. 88: 1183-6
8. Rodríguez BM, Sánchez RF, Domenech Abellán E, Parra JZ, Canovas CS, Castellón Sánchez MI. Bertolotti syndrome: A little known cause of low-back pain in childhood. J Pediatr. 2015. 166: 202
9. Sumarriva G, Cook B, Celestre P. Surgical resection of Bertolotti syndrome. Ochsner J. 2022. 22: 76-9