- Department of Neurosurgery, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
Correspondence Address:
Nancy Ellen Epstein
Department of Neurosurgery, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
DOI:10.4103/2152-7806.182546
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Epstein NE. A review: Reduced reoperation rate for multilevel lumbar laminectomies with noninstrumented versus instrumented fusions. Surg Neurol Int 17-May-2016;7:
How to cite this URL: Epstein NE. A review: Reduced reoperation rate for multilevel lumbar laminectomies with noninstrumented versus instrumented fusions. Surg Neurol Int 17-May-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/a-review-reduced-reoperation-rate-for-multilevel-lumbar-laminectomies-with-noninstrumented-versus-instrumented-fusions/
Abstract
Background:The reoperation rate, including for adjacent segment disease (ASD), is lower following multilevel lumbar laminectomy with noninstrumented versus instrumented fusions.
Methods:This study reviews selected literature focusing on the reoperation rate, including for ASD, following multilevel laminectomies with noninstrumented versus instrumented fusions. Several prior studies document a 1.3–5.6% reoperation rate following multilevel laminectomy with/without noninstrumented fusions.
Results:The reoperation rates for instrumented fusions, including for ASD, are substantially higher. One study cited a 12.2–18.5% frequency for reoperation following instrumented transforaminal lumbar and posterior lumbar interbody fusions (TLIF and PLIFs) at an average of 164 postoperative months. Another study cited a 9.9% reoperation rate for ASD 1 year following PLIF; this increased to 80% at 5 postoperative years. A further study compared 380 patients variously undergoing laminectomies/noninstrumented posterolateral fusions, laminectomies with instrumented fusions (PLFs), and laminectomies with instrumented PLF plus an interbody fusions; this study documented no significant differences in outcomes for any of these operations at 4 postoperative years. Furthermore, other series showed fusion rates for 1–2 level procedures which were often similar with or without instrumentation, while instrumentation increased reoperation rates and morbidity.
Conclusions:Many studies document no benefit for adding instrumentation to laminectomies performed for degenerative disease, including spondylolisthesis. Reoperation rates for laminectomy alone/laminectomy with noninstrumented fusions vary from 1.3% to 5.6% whereas reoperation rates for ASD after instrumented PLIF was 80% at 5 postoperative years. This review should prompt spinal surgeons to reexamine when, why, and whether instrumentation is really necessary, particularly for treating degenerative lumbar disease.
Keywords: Adjacent segment disease, instrumented fusion, low reoperation rate, lumbar surgery, multilevel laminectomy, noninstrumented fusion, spondylolisthesis
INTRODUCTION
In this review, we document that the reoperation rate, including for adjacent segment disease (ASD), is lower following multilevel lumbar laminectomy with noninstrumented versus instrumented fusions. We utilized literature focused on the reoperation rate, including for ASD, after multilevel laminectomies with noninstrumented versus instrumented fusions. In a previous study from 2008, only 1 (1.3%) of 75 predominantly geriatric patients undergoing multilevel laminectomy with noninstrumented fusion required a reoperation.[
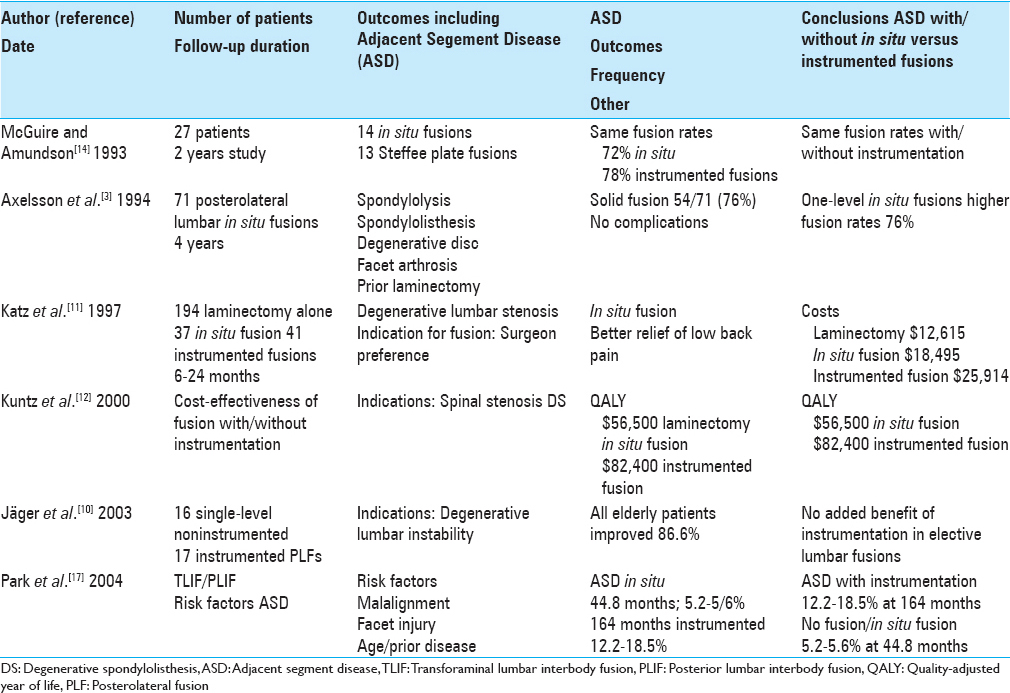
Primary internal fixation in spondylolisthesis
In 1993, McGuire and Amundson in their prospective randomized 2-year study evaluated the efficacy of primary fusions for two groups of patients with spondylolisthesis undergoing L5 laminectomy (Gill procedure)/L5 nerve root decompressions [
Comments: Although the number of patients in this study's two groups undergoing decompressions with noninstrumented versus instrumented fusions was extremely small, the comparable frequencies of fusion for 1 and 2 level procedures, respectively, 10 (72%) of 14 and 11 (78%) of 13 were of interest.[
About 71 posterolateral lumbar fusions; outcomes at 4 years
In 1994, Axelsson et al. reported on the outcomes of 71 consecutive posterolateral lumbar fusions performed without spinal instrumentation at 4 postoperative years [
Comments: This study documented a 76% fusion rate (54 of 71 patients) among a rather varied patient population undergoing laminectomy with noninstrumented fusion.[
Lumbar laminectomy alone or with instrumented or noninstrumented arthrodesis in degenerative lumbar spinal stenosis
Katz et al. in 1997 evaluated the results of laminectomy alone, laminectomy/noninstrumented fusions, and laminectomy/instrumented fusions for lumbar stenosis over a 6–24-month postoperative period [
Comments: There are several factors that are of interest in this study.[
Cost-effectiveness of fusion with/without instrumentation for spinal stenosis and degenerative spondylolisthesis
Kuntz et al. in 2000 looked at the cost-effectiveness and benefits of laminectomy alone and laminectomy with lumbar fusion (noninstrumented vs. instrumented) for patients with degenerative lumbar spondylolisthesis and spinal stenosis [
Comments: This study documented utilizing QALY data that instrumentation costs more without a clear-cut “value added.”[
Clinical outcome in single-level noninstrumented versus instrumented fusion for degenerative lumbar instability
In 2003, Jäger et al. evaluated the outcome of 16 single-level noninstrumented versus 17 instrumented posterolateral fusions in elderly patients with degenerative lumbar instability [
Comments: This article cites an extraordinarily small number of patients in each sample; 16 single-level noninstrumented versus 17 instrumented posterolateral fusions for older patients with degenerative lumbar instability.[
Adjacent segment disease after lumbar or lumbosacral fusion: Review of the literature
Park et al. in 2004 assessed the risk factors contributing to ASD in their review article of TLIF and PLIF [
Comments: This is an extraordinary study that was well ahead of its time. It nicely documented the much lower reoperation rate for ASD following laminectomy alone or with noninstrumented fusion (5.2–5.6%) compared with a much higher 12.2–18.5% reoperation rate with instrumented fusions.[
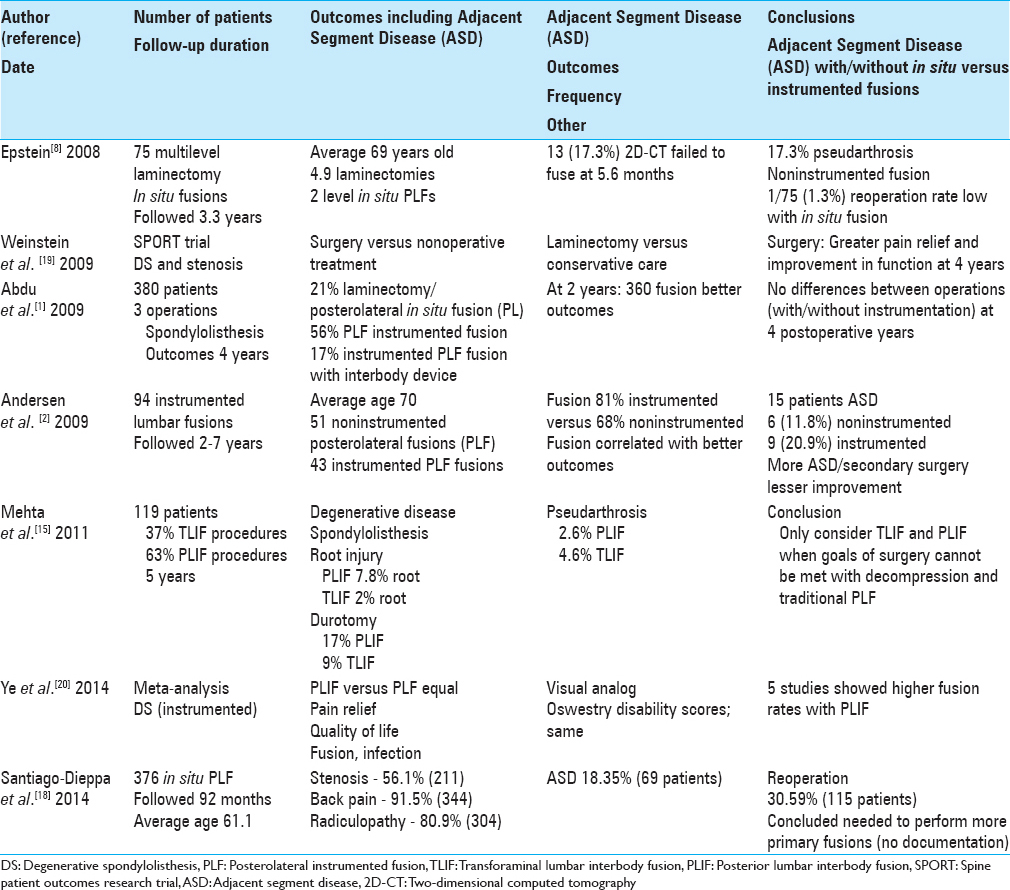
Fusion rates and short form-36 outcomes after multilevel laminectomy and noninstrumented lumbar fusions in a predominantly geriatric population
In 2008, Epstein prospectively analyzed posterolateral fusion rates and short form-36 (SF-36) outcomes for 75 patients, averaging 69 years of age, underwent average 4.9 level lumbar laminectomies and average 2.0 level noninstrumented fusions using lamina autograft and demineralized bone matrix [
Comments: This study involved 75 multilevel laminectomies with noninstrumented fusions performed in largely geriatric patients (e.g., average age 69).[
Surgical versus nonoperative treatment for lumbar degenerative spondylolisthesis; 4-year results in the Spine Patient Outcomes Research Trial (SPORT)
Weinstein et al. in the 2009 Spine Patient Outcomes Research Trial (SPORT) trial (13 centers/11 states) evaluated 4-year postoperative results of surgical versus nonoperative treatment of degenerative spondylolisthesis (DS) [
Comments: In this large SPORT study, patients with DS and spinal stenosis were treated with decompressive laminectomy (with or without fusion) versus nonoperative care.[
Degenerative spondylolisthesis: Does the fusion method influence outcome?
Abdu et al. in 2009 compared the outcomes of different fusion methods for treating DS [
Comments: This large SPORT database study evaluated 380 patients who were variously treated with decompressive laminectomy with posterolateral in situ fusion, PPS, PPS plus interbody fusion, or laminectomies alone.[
Impact of 94 noninstrumented versus instrumented lumbar fusions in elderly patients followed for 2–7 years
In 2009, Andersen et al. looked at the impact of performing 94 lumbar spinal fusions with/without instrumentation utilizing fresh frozen allograft versus autograft to avoid donor-site pain in older patients (e.g., average age 70; range 60–88) [
Comments: This study is a unique example wherein higher fusion rates were for instrumented (81%) versus noninstrumented fusions correlated with better outcomes.[
Surgical morbidity of transforaminal lumbar interbody fusion versus posterior lumbar interbody fusion
Over a 5-year period, Mehta et al. in 2011 retrospectively compared the relative risk of durotomy, nerve root injury, and other complications utilizing TLIF (37% of patients with its unilateral exposure) versus PLIF (63% of patient with its bilateral exposure) for 119 patients’ with degenerative spinal disease or spondylolisthesis [
Comments: What first stands out in this instrumented TLIF/PLIF study were the rather poor indications for surgery; for example, 92% of 119 patients had surgery for mechanical back pain, 80% for radicular pain, while only 8% had motor deficits.[
The comparison of instrumented and noninstrumented fusion in the treatment of lumbar degenerative spondylolisthesis: A meta-analysis
Ye et al. in 2014 performed a meta-analysis to determine whether lumbar noninstrumented versus instrumented fusions differently impacted patient-centered outcomes [
Comments: This meta-analysis evaluated patients with low back pain due to isthmic spondylolisthesis or DS undergoing instrumented versus noninstrumented fusions; interestingly, clinical outcomes were comparable for both groups.[
Noninstrumented lumbar fusions address different types of spinal degenerative lumbar diseases
Santiago-Dieppa et al. in 2014 noted that noninstrumented lumbar fusions address different types of spinal degenerative diseases [
Comments: This study retrospectively evaluated 376 patients who underwent lumbar multilevel laminectomy with noninstrumented fusions for relatively minimal indications: 91.5% had back pain and 80.9% had radiculopathy.[
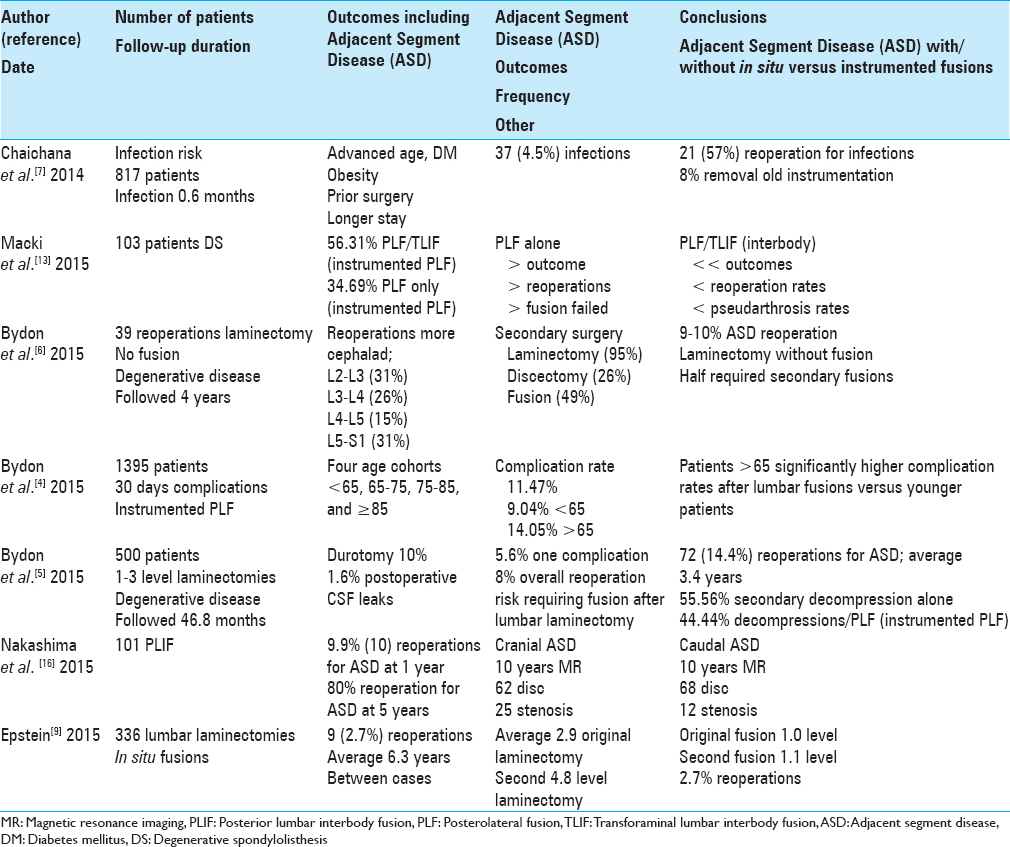
Risk of infection following 817 consecutive posterior instrumented lumbar fusions for degenerative spine disease
Chaichana et al. in 2014 evaluated the incidence and risk factors contributing to infections for lumbar spinal fusions performed to address degenerative lumbar disease [
Comments: In this study, 37 (4.5%) of 817 consecutive lumbar instrumented fusions became infected and 21 (57%) required reoperations.[
Lower reoperation rate for posterolateral fusion/interbody device versus posterolateral fusion alone for lumbar spondylolisthesis
Macki et al. in 2015 evaluated whether better outcomes could be achieved in 103 patients with DS utilizing either instrumented posterolateral fusion (PLF) with an interbody fusion device (PLF + PLIF/TLIF: 56.31%) versus instrumented posterolateral fusion (PLF: 43.69%) alone [
Comments: Here, we have 103 patients with DS undergoing PLF or PLF + PLIF/TLIF; most likely many of these patients could have been adequately managed with laminectomy alone or with laminectomy/noninstrumented fusions.[
Incidence of adjacent segment disease requiring reoperation after lumbar laminectomy without fusion: A study of 398 patients
Bydon et al. in 2015 determined a 9–10% incidence of ASD requiring reoperations following 1 (10%)–2 (9%) level laminectomy without fusion, respectively, in patients with degenerative spinal disease [
Comments: At 4 postoperative years, this study nicely documents that the risk of ASD following 1–2 level laminectomy was 10% for 1 level and 9% for 2 level procedures.[
Impact of age on short-term outcomes after lumbar fusion
Bydon et al. in 2015 studied the safety and efficacy (e.g., 30-day complication rate) for older patients undergoing instrumented posterolateral lumbar fusions between 2005 and 2011 [
Comments: This study documents, utilizing NSQUIP data, that the 30-day complication rate for 1395 patients undergoing instrumented posterolateral fusions was 11.47%: <65 it was 9.04% versus >65 it was 14.05%.[
Clinical and surgical outcomes of 500 patients after lumbar laminectomy
Bydon et al. in 2015 retrospectively evaluated the outcomes for 500 patients undergoing initial 1–3 level laminectomies for degenerative lumbar disease (e.g., excluding discectomy, complete facetectomy, and fusion) over an average of 46.79 months [
Comments: In this study, outcomes for 500 patients undergoing initial 1–3 level laminectomies for degenerative lumbar disease, 72 patients (14.40%) required reoperations for ASD at an average of 3.40 years later; 55.56% decompressions alone versus 44.44% decompressions/posterolateral fusions.[
Adjacent segment disease after posterior lumbar interbody fusion (PLIF): 10 years of follow-up
Nakashima et al. in 2015 evaluated 101 patients undergoing PLIF [
Comments: This is one of the most ground-breaking studies regarding the high risk of ASD for patients undergoing PLIF instrumented fusions; 9.9% at 1 year, but a staggering 80% at 5 postoperative years.[
Low reoperation rate following 336 multilevel lumbar laminectomies with noninstrumented fusions
Epstein in 2016 evaluated 336 patients who had undergone at an initial average of 4.7 level lumbar laminectomies with an average of 1.4 level noninstrumented fusions over an average of 7.1-year period (range 2.0–16.5 years) [
Comments: The reoperation rate following multilevel laminectomy with noninstrumented fusion in this series was 2.7%: 9 of 336 patients an average of 6.3 years postoperatively required secondary surgery.[
SUMMARY
The risk of reoperation, including for ASD, following laminectomy with noninstrumented fusion remains lower than for instrumented fusions.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abdu WA, Lurie JD, Spratt KF, Tosteson AN, Zhao W, Tosteson TD. Degenerative spondylolisthesis: Does fusion method influence outcome? Four-year results of the spine patient outcomes research trial. Spine (Phila Pa 1976). 2009. 34: 2351-60
2. Andersen T, Christensen FB, Niedermann B, Helmig P, Høy K, Hansen ES. Impact of instrumentation in lumbar spinal fusion in elderly patients: 71 patients followed for 2-7 years. Acta Orthop. 2009. 80: 445-50
3. Axelsson P, Johnsson R, Strömqvist B, Arvidsson M, Herrlin K. Posterolateral lumbar fusion.Outcome of 71 consecutive operations after 4 (2-7) years. Acta Orthop Scand. 1994. 65: 309-14
4. Bydon M, Abt NB, De la Garza-Ramos R, Olorundare IO, McGovern K, Sciubba DM. Impact of age on short-term outcomes after lumbar fusion: An Analysis of 1395 patients stratified by decade cohorts. Neurosurgery. 2015. 77: 347-53
5. Bydon M, Macki M, Abt NB, Sciubba DM, Wolinsky JP, Witham TF. Clinical and surgical outcomes after lumbar laminectomy: An analysis of 500 patients. Surg Neurol Int. 2015. 6: S190-3
6. Bydon M, Macki M, De la Garza-Ramos R, McGovern K, Sciubba DM, Wolinsky JP. Incidence of adjacent segment disease requiring reoperation after lumbar laminectomy without fusion: A study of 398 patients. Neurosurgery. 2015. p.
7. Chaichana KL, Bydon M, Santiago-Dieppa DR, Hwang L, McLoughlin G, Sciubba DM. Risk of infection following posterior instrumented lumbar fusion for degenerative spine disease in 817 consecutive cases. J Neurosurg Spine. 2014. 20: 45-52
8. Epstein NE. Fusion rates and SF-36 outcomes after multilevel laminectomy and noninstrumented lumbar fusions in a predominantly geriatric population. J Spinal Disord Tech. 2008. 21: 159-64
9. Epstein NE. Low reoperation rate following 336 multilevel lumbar laminectomies with non-instrumented fusions. Surg Neurol Int. 2016. 7: 349-54
10. Jäger M, Seller K, Raab P, Krauspe R, Wild A. Clinical outcome in monosegmental fusion of degenerative lumbar instabilities: Instrumented versus non-instrumented. Med Sci Monit. 2003. 9: CR324-7
11. Katz JN, Lipson SJ, Lew RA, Grobler LJ, Weinstein JN, Brick GW. Lumbar laminectomy alone or with instrumented or noninstrumented arthrodesis in degenerative lumbar spinal stenosis.Patient selection, costs, and surgical outcomes. Spine (Phila Pa 1976). 1997. 22: 1123-31
12. Kuntz KM, Snider RK, Weinstein JN, Pope MH, Katz JN. Cost-effectiveness of fusion with and without instrumentation for patients with degenerative spondylolisthesis and spinal stenosis. Spine (Phila Pa 1976). 2000. 25: 1132-9
13. Macki M, Bydon M, Weingart R, Sciubba D, Wolinsky JP, Gokaslan ZL. Posterolateral fusion with interbody for lumbar spondylolisthesis is associated with less repeat surgery than posterolateral fusion alone. Clin Neurol Neurosurg. 2015. 138: 117-23
14. McGuire RA, Amundson GM. The use of primary internal fixation in spondylolisthesis. Spine (Phila Pa 1976). 1993. 18: 1662-72
15. Mehta VA, McGirt MJ, Garcés Ambrossi GL, Parker SL, Sciubba DM, Bydon A. Trans-foraminal versus posterior lumbar interbody fusion: Comparison of surgical morbidity. Neurol Res. 2011. 33: 38-42
16. Nakashima H, Kawakami N, Tsuji T, Ohara T, Suzuki Y, Saito T. Adjacent segment disease after posterior lumbar interbody fusion: Based on Cases with a minimum of 10 years of follow-up. Spine (Phila Pa 1976). 2015. 40: E831-41
17. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: Review of the literature. Spine (Phila Pa 1976). 2004. 29: 1938-44
18. Santiago-Dieppa D, Bydon M, Xu R, De la Garza-Ramos R, Henry R, Sciubba DM. Long-term outcomes after non-instrumented lumbar arthrodesis. J Clin Neurosci. 2014. 21: 1393-7
19. Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, Tosteson AN. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis.Four-year results in the Spine patient outcomes research trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009. 91: 1295-304
20. Ye YP, Chen D, Xu H. The comparison of instrumented and non-instrumented fusion in the treatment of lumbar spondylolisthesis: A meta-analysis. Eur Spine J. 2014. 23: 1918-26