- Department of Neurosurgery, The Walton Centre NHS Foundation Trust, Liverpool,
- School of Health and Care Professions, University of Portsmouth, Portsmouth,
- Division of Neurosciences, Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom,
- School of Medicine, Aristotle University of Thessaloniki, Greece,
- Fondazione IRCCS Istituto Neurologico “Carlo Besta”, Milano,
- Department of Neurosurgery, Humanitas Research Hospital, Rozzano, Italy,
- Division of Neurosurgery, University of Strasbourg, Strasbourg, France,
- North West General Hospital and Research Centre, Khyber Pakhtunkhwa, Peshawar, Pakistan,
- Neuro Intensive Care Unit, Oxford, United Kingdom.
- 0Department of Neurosurgery, Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom.
Correspondence Address:
Mario Ganau, Department of Neurosurgery, Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom.
DOI:10.25259/SNI_203_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Davor Dasic1, Lucy Morgan2, Amir Panezai3, Nikolaos Syrmos4, Gianfranco K.I. Ligarotti5, Ismail Zaed6, Salvatore Chibbaro7, Tariq Khan8, Lara Prisco9, Mario Ganau10. A scoping review on the challenges, improvement programs, and relevant output metrics for neurotrauma services in major trauma centers. 29-Apr-2022;13:171
How to cite this URL: Davor Dasic1, Lucy Morgan2, Amir Panezai3, Nikolaos Syrmos4, Gianfranco K.I. Ligarotti5, Ismail Zaed6, Salvatore Chibbaro7, Tariq Khan8, Lara Prisco9, Mario Ganau10. A scoping review on the challenges, improvement programs, and relevant output metrics for neurotrauma services in major trauma centers. 29-Apr-2022;13:171. Available from: https://surgicalneurologyint.com/surgicalint-articles/11573/
Abstract
Background: For a neurotrauma unit to be defined as a structured neurotrauma service (NS) the following criteria must be satisfied: A dedicated neurointensive care unit, endovascular neuroradiology, in-hospital neurorehabilitation unit and helicopter platform within the context of a Level I trauma center. Designing an effective NS can be challenging, particularly when considering the different priorities and resources of countries across the globe. In addition the impact on clinical outcomes is not clearly established.
Methods: A scoping review of the literature spanning from 2000 to 2020 meant to identify protocols, guidelines, and best practices for the management of traumatic brain injury (TBI) in NS was conducted on the US National Library of Medicine and National Institute of Health databases.
Results: Limited evidence is available regarding quantitative and qualitative metrics to assess the impact of NSs and specialist follow-up clinics on patients’ outcome. Of note, the available literature used to lack detailed reports for: (a) Geographical clusters, such as low-to-middle income countries (LMIC); (b) clinical subgroups, such as mild TBI; and (c) long-term management, such as rehabilitation services. Only in the last few years more attention has been paid to those research topics.
Conclusion: NSs can positively impact the management of the broad spectrum of TBI in different clinical settings; however more research on patients’ outcomes and quality of life metrics is needed to establish their efficacy. The collaboration of global clinicians and the development of international guidelines applicable also to LMIC are warranted.
Keywords: Clinical outcome measures, Global neurosurgery, Guidelines, Head injury, Major trauma center, Neurotrauma
INTRODUCTION
Being the most common cause of death and disability in the young population (under 40 years old), traumatic brain injury (TBI) is a global health problem with widespread economic implications.[
The clinical and financial implications of TBI management call for the identification of best practices and the standardization of neurotrauma services (NSs).[
It is well known that modern advances in the clinical management of trauma patients are mostly based on guidelines that minimize the time interval between injury and primary care, improve hospital management, and overall help reducing the fatalities and sequelae of TBI worldwide.[
MATERIALS AND METHODS
Given this background, we defined the following research question: “is there any evidence for establishing the impact of structured NS on hospitals’ resource allocation and patients’ outcomes?,” and established the following two objectives: (a) To assess how current guidelines and protocols are designed and updated; and (b) to compare the relationship between adherence to guidelines and health economic performance in high-income countries (HIC) versus low- and middle-income countries (LMIC) around the world.
To achieve those objectives and answer our research question, a scoping review of the literature meant to identify protocols, guidelines, and best practices for the management of TBI in NS has been performed. The search was conducted on the US National Library of Medicine and National Institute of Health databases using the following MeSH terms: “traumatic brain injury,” “neurotrauma,” “health economics,” “regionalized trauma system.” We included only English-written articles relevant to the topic published between 2000 and 2020. Following an abstract-based screening of all articles, a second triaging led to the identification of those appropriate for inclusion and discussion in the present study. A consensus sought among authors through a Delphi approach solved any disagreement regarding articles’ suitability for inclusion.
Finally, to ensure quality and internal consistency, the authors relied on the checklist for reporting scoping review for the preparation of this manuscript.[
RESULTS
The review of the literature led to the selection of 58 articles. An analysis of their publication date indicated a 6-fold increase in the number of studies published over the last decade.
The first objective of this scoping review was achieved by selecting position statements, guidelines and protocols issued by national and international societies. Their recommendations are not always based on evidence but instead on consensus (suggesting a clash between evidence based medicine and eminence based medicine). Regarding the second objective, limited evidence is available regarding quantitative and qualitative metrics to assess the impact of NSs and specialist follow-up clinics on patients’ outcome. The available literature between 2000 and 2010 (8 articles) used to lack detailed reports for: (a) geographical clusters, such as LMIC; (b) clinical subgroups, such as mild TBI (mTBI); and (c) long-term management, such as rehabilitation services. Only in the last decade more attention has been paid to those research topics. Based on the data collected, the authors have proposed a series of recommendations for LMIC and a matrix for future research pertaining to NS.
The role of NSs
The literature provides evidence that established network protocols for Major Trauma Centers (MTCs) exist in most HIC, and include access to neurosurgical consultant/ attending/faculty-led care 24 h a day. An organized trauma system has been found to improve mortality in head-injured patients; for instance, Moran et al. demonstrated that the formal creation of a NS has led to significant improvement in overall mortality.[
To further optimize this admission pathway some pilot studies have been conducted. A recent innovative cluster-randomized trial was conducted by two UK-based ambulance services to examine the feasibility and measurable effects of directing patients with suspected TBI directly to specialist neurosurgical centers.[
NSs in the context of international guidelines
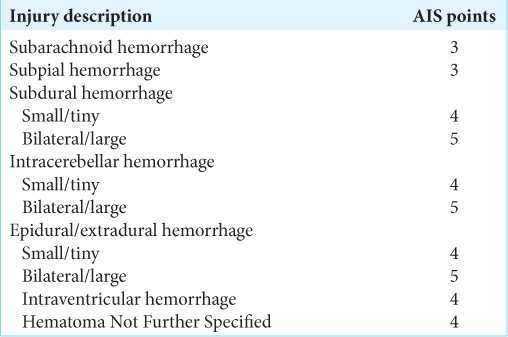
Many international scientific societies support the view that patients with severe head injuries irrespective of their need for surgery should be managed within a NS, and all those patients with evolving neurosurgical conditions should be promptly referred to it for ongoing specialist care. Equally, it should be noted that even less severe head injuries might require management within MTCs if they have other injuries warranting admission and a higher level of specialist care. Accordingly, while the most important parameters to assess the level of consciousness remain the Glasgow Coma Scale and the pupillary reactivity,[
Compliance with protocols issued by international societies is high in Western Europe, the Americas, and several Asian countries such as India, China, Japan, South Korea, and Singapore. Exemplificative cases indicate that the implementation of guidelines issued by the Brain Trauma Foundation led to a significant decrease in hospital days, improvement in clinical outcomes and optimization of financial return on investments made for this patients group.[
Referral to major trauma centers for acute care
In the context of the demands already faced by Emergency Departments (A&E), the sheer number of TBI patients that attend tertiary hospitals can place significant pressure on already stretched services. Up to 1.4 million patients attend the A&E in England and Wales each year with head injuries.[
Timing of admission is also very important and deserves attention by all stakeholders involved in the management of TBI patients. Comparative European data, possibly reflecting the higher population density in the continent, demonstrate that 80% of patients with severe TBI are admitted to a neurosurgical center within 12 h of injury and 68% within 4 h.[
Usually, the predominant number of TBI patients requiring initial neurosurgical telemedicine referral will remain in their referring hospitals since intensive multimodality monitoring or surgical treatment will not be deemed necessary.[
mTBI
In a recent global neurotrauma report Dewan et al. proposed a predictive model estimating that 64–74 million cases of TBI will occur worldwide annually. The majority of these (up to 81%) are predicted to be mTBI;[
Since over-triage of mTBI can consume existing resources available at the specialized care hospitals (subsequently limiting the adequate management of the moderate to severe TBI cases), the role for improved patient categorization cannot be stressed enough.[
Evidence regarding global neurotrauma provision has been reviewed for this article however a more robust analysis when large series will be available would be beneficial. It is clear that the challenges of TBI in different countries and continents are markedly different and strategies and improvement programs to ameliorate overall patient outcome is imperative.
Rehabilitation pathways
MTC patients are particularly complex and require specialized inpatients and outpatients’ pathways including appropriate rehabilitation programs. To facilitate the flow of patients from higher to lower levels of care an early and appropriate assessment is of fundamental importance, especially given the evidence that earlier access to multidisciplinary rehabilitation improves outcome.[
The rehabilitation requirements and resources available to this patient population vary from country to country, and even in the same nation, due to a markedly heterogeneous population, as well as significant differences in specialist rehabilitation provision by area. It is estimated that whilst 80% of the world’s population live in LMIC, only 2% have access to rehabilitation services;[
High - versus LMIC
As highlighted above the global incidence of TBI is rising and its burden is already apparent in any country across the globe; however, this is particularly prominent in the African continent and several Asian countries. Universal care access is lacking and the availability of tertiary neurosurgical units and rehabilitation is extremely limited in particular regions of the world.[
LMIC have a high proportion of risk factors for TBI, whilst simultaneously having the fewest available resources to effectively manage this complex population.[
Recommendations for NSs in LMIC
Due to the types of articles reviewed by this scoping review it would be difficult to apply the GRADE Working Group criteria ( Although our scoping review demonstrated that international guidelines improve TBI outcomes, it also showed that such guidelines have all been designed in HIC (mostly for HIC). It follows that an automatic translation to other healthcare systems is not appropriate due to the mismatch between the necessary pre-requisites for the application of those guidelines and the resources available in the specific local context of LMIC. In fact, our results indicate those latter countries have wider heterogeneity of pre-hospital emergency care and regional trauma systems, hospital infrastructures, and human resources One recommendation that can be formulated is therefore that regional standardized trauma care protocols should be context-specific, in other words they should be reversed engineered around the geographical characteristics, populations’ needs and resource limitations of each national healthcare system in LMIC. In doing so, healthcare managers and politicians should make use of the AGREE (Appraisal of Guidelines for Research & Evaluation) tools ( Emergency care is essential for universal, quality, and non-discriminatory healthcare delivery; as such continuously extended and upgraded training of all medical staff represents a priority. This is particularly important in remote areas, where general surgeons, orthopedic surgeons, and trauma surgeons should be nudged to expand their curriculum to match the needs of NS. In African countries where this was attempted (see Prospero Database: CRD42021258097) the minimal complication rate recorded did not indicate issues in terms of quality of care Hence, another suggestions for NSs in LMIC is that they should rely on a broader group of surgeons, adequately trained by local neurosurgeons, to perform lifesaving procedures, such as emergency burr holes and decompressive craniectomy Due to the differences in the natural history of mTBI and the demands for decentralized rehabilitation pathways, NSs in LMIC should leverage on telemedicine consultation to optimize patients’ care. Access to fast internet connections (either broadband or through communication satellites) represents a priority for LMIC because the availability of real time, widespread digital medicine would allow those countries to catch up with the standard of care provided in HIC It is recommended that LMIC consider telemedicine as the most readily available option to reduce the burden of non-acute management of TBI and long term follow-up on its NS The growing attention to global neurosurgery matters has also led to the recognition that not every aspect of neurosurgical practice has the same weight, challenges and constraints in different countries. Education and development of neurosurgery trainees anywhere in the world remains essential and has always been one the first and foremost mandate of scientific societies, including the World Federation of Neurosurgical Societies and European Association of Neurosurgical Societies. Noteworthy, the way neurosurgical education is delivered was reshaped over the last 2 years as a result of COVID19, and this should be kept in mind for future planning A lecture-panel-discussion model where experts trained in HIC and currently working in LMIC teachs other practitioners facing similar experiences could be recommended as a pivotal aspect of developing surgical skills and trauma competences in any LMIC.
Research in NSs
From the analysis of the literature and the secondary data sources identified by this scoping review, it is clear that further primary research is required to define the impact of NSs on TBI outcomes. Given the broad spectrum of neurotrauma mechanisms and required interventions, as well as regional differences in patient needs, markedly different priorities in the management of TBI exist within countries and between countries. The majority of TBI research is also conducted in HIC hence the current lack of evidence available to tackle the challenges of TBI management in reduced resource areas. In recent years this indicated an urgent need for international collaborative studies for future research and service development. Accordingly, the newly established National Institute for Health Research (NIHR) Global Health Research Group on Neurotrauma (whose activities are strongly supported by the Neurotrauma Committee of the World Federation of Neurosurgical Societies) aims to address the existing gap by producing evidence that should directly benefit patients anywhere in the world. The group aims to gain an in depth understanding of the global needs of TBI patients by creating a centralized TBI registry including details of emergency surgery, evaluating interventions used in LMIC and mapping future research in LMIC demonstrating significant steps toward improving outcomes for these patients. Specifically, follow-up and rehabilitation of TBI patients will require significantly more input from local governments as the current investment in this aspect of patient care is still reported to be fairly minimal.[
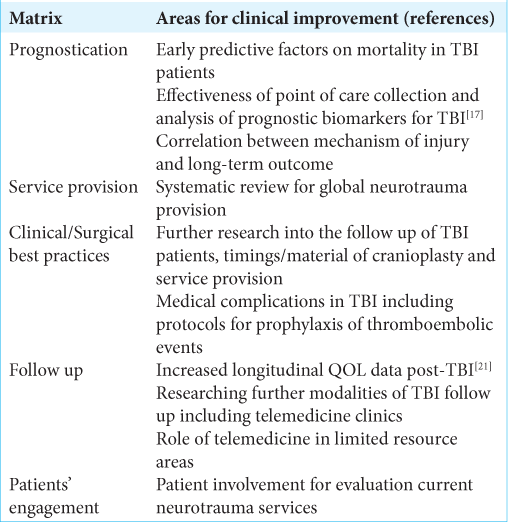
Based on this scoping review, beside the aspects discussed above, we have identified other examples of unmet needs in neurotrauma; those have been incorporated into a matrix showing the future areas for potential research in this field [
Study limitations
Despite the authors’ best efforts, this study presents several limitations, mostly related to the nature of the research question, which was deemed more suitable for a scoping review than a systematic one. In fact, some quantifiable aspects of neurotrauma management including granular information regarding type and timing required for pre-hospital rescue and transfer, type of imaging modalities required on admission and during in-hospital stay, type of surgical and medical treatment administered, and availability of multidisciplinary discussion teams were not available for further analysis. For this reason, our research question was not prone to a formal meta-analysis.
Another limitation regard the timeframe considered for our study. Whereas clinicians and public health institutions have recently started to pay more attention to the global burden of TBI, the literature up to 2020 might have not yet reflected how the initiatives spurred by such widespread interest are bringing effective changes in our clinical practice.
CONCLUSION
Due to the heterogeneous data and low evidence identified by this scoping review, more research is needed to assess the efficacy and usefulness of structured NSs in terms of patient outcome and quality of life metrics. International collaboration between relevant clinicians is required to produce best practice guidelines and research applicable also to those centers located in LMIC. Various aspects outlined in this study will likely be an integral part of these research progresses over the coming years. Our results further highlight that future studies set in LMIC should ideally investigate the impact of lack of rehabilitation and follow-up services for post-TBI patients in these settings. This should include patients with mTBI and the potential role they play on limited resource systems.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are thankful to Javier Magan Ventura RN, Clinical Research Network – National Institute for Health Research for his valuable support on critical review of our data collection and preparation of the manuscript.
References
1. Ahmed W, Alwe R, Wade D. One-year functional outcomes following major trauma: Experience of a UK level 1 major trauma centre. Clin Rehabil. 2017. 31: 1646-52
2. Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974. 14: 187-96
3. Bedry T, Tadele H. Pattern and outcome of pediatric traumatic brain injury at Hawassa University comprehensive specialized hospital, Southern Ethiopia: Observational cross-sectional study. Emerg Med Int. 2020. 2020: 1965231
4. Bond K, Ospina MB, Blitz S, Afilalo M, Campbell SG, Bullard M. Frequency, determinants and impact of overcrowding in emergency departments in Canada: A national survey. Healthc Q. 2007. 10: 32-40
5. Brennan PM, Murray GD, Teasdale GM. Simplifying the use of prognostic information in traumatic brain injury. Part 1: The GCS-Pupils score: An extended index of clinical severity. J Neurosurg. 2018. 128: 1612-20
6. Budohoski KP, Ngerageza JG, Austard B, Fuller A, Galler R, Haglund M. Neurosurgery in East Africa: Innovations. World Neurosurg. 2018. 113: 436-52
7. Butchart A, Mikton C, Dahlberg LL, Krug EG. Global status report on violence prevention 2014. Inj Prev. 2015. 21: 213
8. Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012. 367: 2471-81
9. Chibbaro S, Cebula H, Todeschi J, Fricia M, Vigouroux D, Abid H. Evolution of prophylaxis protocols for venous thromboembolism in neurosurgery: Results from a prospective comparative study on low-molecular-weight heparin, elastic stockings, and intermittent pneumatic compression devices. World Neurosurg. 2018. 109: e510-6
10. Citerio G, Prisco L, Oddo M, Meyfroidt G, Helbok R, Stocchetti N. International prospective observational study on intracranial pressure in intensive care (ICU): The SYNAPSE-ICU study protocol. BMJ Open. 2019. 9: e026552
11. Civil ID, Schwab CW. The abbreviated injury scale, 1985 revision: A condensed chart for clinical use. J Trauma. 1988. 28: 87-90
12. Cnossen MC, Polinder S, Lingsma HF, Maas AI, Menon D, Steyerberg EW. Variation in structure and process of care in traumatic brain injury: Provider profiles of european neurotrauma centers participating in the CENTER-TBI study. PLoS One. 2016. 11: e0161367
13. Davis T, Ings A. Head injury: Triage, assessment, investigation and early management of head injury in children, young people and adults (NICE guideline CG 176). Arch Dis Child Educ Pract Ed. 2015. 100: 97-100
14. Derlet R, Richards J, Kravitz R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med. 2001. 8: 151-5
15. Devi BI, Shukla DP, Bhat DI, Tripathi M, Warren A, Shanbhag NC. Neurotrauma care delivery in a limited resource setting-lessons learned from referral and patient flow in a tertiary care center. World Neurosurg. 2019. 123: e588-96
16. Dewan MC, Rattani A, Gupta S, Baticulon RE, Hung YC, Punchak M. Estimating the global incidence of traumatic brain injury. J Neurosurg. 2018. 130: 1-18
17. Di Pietro V, Porto E, Ragusa M, Barbagallo C, Davies D, Forcione M. Salivary microRNAs: Diagnostic markers of mild traumatic brain injury in contact-sport. Front Mol Neurosci. 2018. 11: 290
18. Fakhry SM, Ferguson PL, Johnson EE, Wilson DA. Hospitalization in low-level trauma centres after severe traumatic brain injury: Review of a population-based emergency department data base. Brain Inj. 2017. 31: 1486-93
19. Fakhry SM, Trask AL, Waller MA, Watts DD. Management of brain-injured patients by an evidence-based medicine protocol improves outcomes and decreases hospital charges. J Trauma. 2004. 56: 492-500
20. Fann JR, Bombardier CH, Vannoy S, Dyer J, Ludman E, Dikmen S. Telephone and in-person cognitive behavioral therapy for major depression after traumatic brain injury: A randomized controlled trial. J Neurotrauma. 2015. 32: 45-57
21. Formisano R, Longo E, Azicnuda E, Silvestro D, D’Ippolito M, Truelle JL. Quality of life in persons after traumatic brain injury as self-perceived and as perceived by the caregivers. Neurol Sci. 2017. 38: 279-86
22. Fricia M, Nicolosi F, Ganau M, Cebula H, Todeschi J, Santin MD. Cranioplasty with porous hydroxyapatite custom-made bone flap: Results from a multicenter study enrolling 149 patients over 15 years. World Neurosurg. 2019. 121: 160-5
23. Fridley J, Robertson C, Gopinath S. Quantitative lobar cerebral blood flow for outcome prediction after traumatic brain injury. J Neurotrauma. 2015. 32: 75-82
24. Ganau L, Prisco L, Ganau M. High altitude induced bilateral non-traumatic subdural hematoma. Aviat Space Environ Med. 2012. 83: 899-901
25. Ganau M, Cebula H, Fricia M, Zaed I, Todeschi J, Scibilia A. Surgical preference regarding different materials for custom-made allograft cranioplasty in patients with calvarial defects: Results from an internal audit covering the last 20 years. J Clin Neurosci. 2020. 74: 98-103
26. Ganau M, Fehlings MG. Clinical and health policy-related challenges of pediatric spinal cord injuries. Neurol India. 2017. 65: 475-6
27. Ganau M, Lavinio A, Prisco L. Delirium and agitation in traumatic brain injury patients: An update on pathological hypotheses and treatment options. Minerva Anestesiol. 2018. 84: 632-40
28. Ganau M, Ligarotti GK, Ganau L, Prisco L. Early cranioplasty is associated with greater neurological improvement: A systematic review and meta-analysis. Neurosurgery. 2018. 83: E87-9
29. Ganau M, Prisco L, Cebula H, Todeschi J, Abid H, Ligarotti G. Risk of deep vein thrombosis in neurosurgery: State of the art on prophylaxis protocols and best clinical practices. J Clin Neurosci. 2017. 45: 60-6
30. Ganau M, Prisco L. Comment on. “neuromonitoring in traumatic brain injury”. Minerva Anestesiol. 2013. 79: 310-1
31. 32. Goldberg HS, Paterno MD, Grundmeier RW, Rocha BH, Hoffman JM, Tham E. Use of a remote clinical decision support service for a multicenter trial to implement prediction rules for children with minor blunt head trauma. Int J Med Inform. 2016. 87: 101-10 33. Hasan S, Chari A, Ganau M, Uff C. Defining new research questions and protocols in the field of traumatic brain injury through public engagement: Preliminary results and review of the literature. Emerg Med Int. 2019. 2019: 9101235 34. Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: A global perspective. NeuroRehabilitation. 2007. 22: 341-353 35. Ibrahim GM, Bernstein M. Models of neurosurgery international aid and their potential ethical pitfalls. Virtual Mentor. 2015. 17: 49-55 36. Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB.editors. Disease Control Priorities in Developing Countries. Washington, DC: The International Bank for Reconstruction and Development/The World Bank; 2006. p. 37. Johnson WD, Griswold DP. Traumatic brain injury: A global challenge. Lancet Neurol. 2017. 16: 949-50 38. Láng J, Ganau M, Prisco L, Bozsik K, Banczerowski P. Syndrome of trephined-underestimated and poorly understood complication after decompressive craniectomy. Ideggyogy Sz. 2016. 69: 227-32 39. Latifi R, Olldashi F, Dogjani A, Dasho E, Boci A, El-Menyar A. Telemedicine for neurotrauma in Albania: Initial results from case series of 146 patients. World Neurosurg. 2018. 112: e747-53 40. Lawrence T, Helmy A, Bouamra O, Woodford M, Lecky F, Hutchinson PJ. Traumatic brain injury in England and Wales: Prospective audit of epidemiology, complications and standardised mortality. BMJ Open. 2016. 6: e012197 41. Lecky FE, Russell W, McClelland G, Pennington E, Fuller G, Goodacre S. Bypassing nearest hospital for more distant neuroscience care in head-injured adults with suspected traumatic brain injury: Findings of the head injury transportation straight to neurosurgery (HITS-NS) pilot cluster randomised trial. BMJ Open. 2017. 7: e016355 42. Marincowitz C, Lecky F, Allgar V, Sheldon T. Evaluation of the impact of the NICE head injury guidelines on inpatient mortality from traumatic brain injury: An interrupted time series analysis. BMJ Open. 2019. 9: e028912 43. McGowan J, Straus S, Moher D, Langlois EV, O’Brien KK, Horsley T. Reporting scoping reviews-PRISMA ScR extension. J Clin Epidemiol. 2020. 123: 177-9 44. Migliaretti G, Ciaramitaro P, Berchialla P, Scarinzi C, Andrini R, Orlando A. Teleconsulting for minor head injury: The piedmont experience. J Telemed Telecare. 2013. 19: 33-5 45. Mock C, Joshipura M, Quansah R, Arreola-Risa C. Advancing injury prevention and trauma care in North America and globally. Surg Clin North Am. 2007. 87: 1-19 46. Moran CG, Lecky F, Bouamra O, Lawrence T, Edwards A, Woodford M. Changing the system major trauma patients and their outcomes in the NHS (England) 2008-17. EClinicalMedicine. 2018. 2-3: 13-21 47. Negida A, Raslan AM. Invitation to the GNS-I study; a global evaluation of traumatic brain injury in low-, middle-, and high income countries. Adv J Emerg Med. 2019. 3: e21 48. Patel HC, Menon DK, Tebbs S, Hawker R, Hutchinson PJ, Kirkpatrick PJ. Specialist neurocritical care and outcome from head injury. Intensive Care Med. 2002. 28: 547-53 49. Picetti E, Oddo M, Prisco L, Helbok R, Taccone FS. A survey on fever monitoring and management in patients with acute brain injury: The SUMMA study. J Neurosurg Anesthesiol. 2019. 31: 399-405 50. Prisco L, Ganau M, Aurangzeb S, Moswela O, Hallett C, Raby S. A pragmatic approach to intravenous anaesthetics and electroencephalographic endpoints for the treatment of refractory and super-refractory status epilepticus in critical care. Seizure. 2020. 75: 153-64 51. Prisco L, Iscra F, Ganau M, Berlot G. Early predictive factors on mortality in head injured patients: A retrospective analysis of 112 traumatic brain injured patients. J Neurosurg Sci. 2012. 56: 131-6 52. Richardson DB, Mountain D. Myths versus facts in emergency department overcrowding and hospital access block. Med J Aust. 2009. 190: 369-74 53. Rubiano AM, Carney N, Chesnut R, Puyana JC. Global neurotrauma research challenges and opportunities. Nature. 2015. 527: S193-7 54. Selveindran SM, Khan MM, Simadibrata DM, Hutchinson PJ, Brayne C, Hill C. Mapping global evidence on strategies and interventions in neurotrauma and road traffic collisions prevention: A scoping review protocol. BMJ Open. 2019. 9: e031517 55. Stein DM, Feather CB, Napolitano LM. Traumatic brain injury advances. Crit Care Clin. 2017. 33: 1-13 56. Suehiro E, Fujisawa H, Koizumi H, Yoneda H, Ishihara H, Nomura S. Survey of current neurotrauma treatment practice in Japan. World Neurosurg. 2011. 75: 563-8 57. Syrmos N, Ganau M, De Carlo A, Prisco L, Ganau L, Valadakis V. Dealing with the surgical and medical challenges of penetrating brain injuries. Case Rep Surg. 2013. 2013: 209750 58. Tarapore PE, Vassar MJ, Cooper S, Lay T, Galletly J, Manley GT. Establishing a traumatic brain injury program of care: Benchmarking outcomes after institutional adoption of evidence-based guidelines. J Neurotrauma. 2016. 33: 2026-33 59. Turner-Stokes L, Pick A, Nair A, Disler PB, Wade DT. Multi-disciplinary rehabilitation for acquired brain injury in adults of working age. Cochrane Database Syst Rev. 2015. 12: CD004170 60. VanItallie TB. Traumatic brain injury (TBI) in collision sports: Possible mechanisms of transformation into chronic traumatic encephalopathy (CTE). Metabolism. 2019. 100S: 153943 61. Velt KB, Cnossen M, Rood PP, Steyerberg EW, Polinder S, Lingsma HF. Emergency department overcrowding: A survey among European neurotrauma centres. Emerg Med J. 2018. 35: 447-8 62. Wan Y, Griffiths S, Ganau M. Neurosurgical care of nonpowder firearm injuries: A narrative review of the literature. Emerg Med Int. 2019. 2019: 4680184 63. Zuckerman SL, Yengo-Kahn AM, Buckley TA, Solomon GS, Sills AK, Kerr ZY. Predictors of postconcussion syndrome in collegiate student-athletes. Neurosurg Focus. 2016. 40: E13