- Department of Neurosurgery, Avicenne Military Hospital of Marrakech, Mohammed V University in Rabat, Rabat, Morocco
- Department of Histopathology, Avicenne Military Hospital of Marrakech, Mohammed V University in Rabat, Rabat, Morocco
Correspondence Address:
Ali Akhaddar
Department of Histopathology, Avicenne Military Hospital of Marrakech, Mohammed V University in Rabat, Rabat, Morocco
DOI:10.4103/sni.sni_64_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Ali Akhaddar, Hassan Baallal, Abderrahim Elktaibi. Abscess due to textiloma (gossypiboma: Retained surgical cottonoid). 05-Apr-2018;9:70
How to cite this URL: Ali Akhaddar, Hassan Baallal, Abderrahim Elktaibi. Abscess due to textiloma (gossypiboma: Retained surgical cottonoid). 05-Apr-2018;9:70. Available from: http://surgicalneurologyint.com/surgicalint-articles/abscess-due-to-textiloma-gossypiboma-retained-surgical-cottonoid/
Abstract
Background:Surgical site infections following spinal surgery, including spinal abscesses, are rare but serious as they are major causes of morbidity, and even mortality. They are, however, rarely attributed to infected, retained surgical cottonoids or sponges (textiloma or gossypiboma) inadvertently left in an operative field.
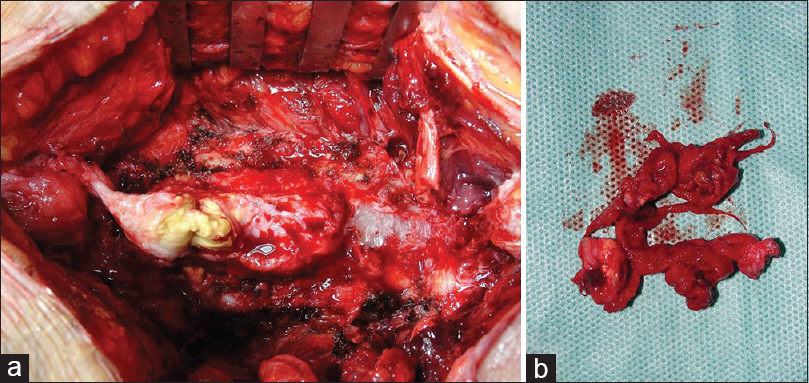
Case Description:A 53-year-old female with a history of two prior spinal operations at the L4-S1 levels (11 and 2 years previously) presented over a few weeks with the acute onset of a cauda equina syndrome (e.g., paraparesis and acute urinary incontinence). The patient demonstrated a mildly elevated white blood cell count (12,600/mm3) and abnormally increased C-reactive protein level that correlated with the magnetic resonance imaging that showed a dorsal epidural abscess extending from the L4 to S1 levels. At surgery, an encapsulated posterior epidural abscess was drained. Surgical findings included a granulomatous lesion consistent with a retained surgical cottonoid and was removed from the antero-inferior portion of the abscess wall at S1. Culture of the thick fibrotic abscess wall grew Klebsiella oxytoca. After 2 months of ciprofloxacin, the patient's infection cleared but the motor deficit only partially resolved.
Conclusion:Most spinal textilomas (gossypibomas) are aseptic and are found in paraspinal areas without neurological symptoms or sequelae. These lesions may remain silent for years and may only rarely cause neurologic or infectious symptoms/signs. Notably, textilomas following spinal surgery may be largely avoided if proper cottonoid and sponge counts are done prior to closing spinal wounds.
Keywords: Cauda equina syndrome, gossypiboma, retained cottonoid, spinal epidural abscess, surgical complication, surgical site infection, textiloma
INTRODUCTION
Surgical site infections (SSIs) following spinal surgery are rare but serious as they are major causes of morbidity, and even mortality.[
CASE PRESENTATION
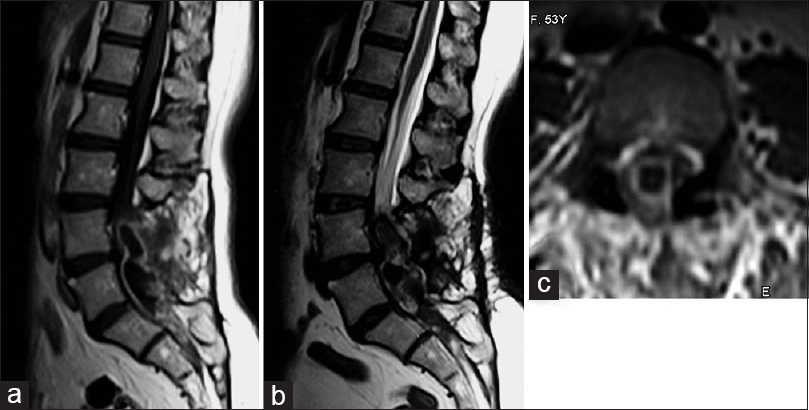
A 53-year-old female with a long history of low back pain had undergone two prior operations: an L5-S1 discectomy (11 years ago) and an L4-L5 decompressive laminectomy (2 years ago). Over several weeks duration, she presented with an acute cauda equina syndrome characterized by paraparesis and acute urinary incontinence. On examination, she had mild tenderness over the lower back region. Laboratory tests revealed mild elevation of the white blood cell count (12,600/mm3), a high C-reactive protein level, and no urinary tract infection. Plain X-rays showed the various laminectomy defects (L4 to L5) due to her prior surgery. The MRI showed an oblong posterior epidural lesion compressing the thecal sac from the L4 to S1 levels; it was hypointense on T1 and hyperintense on T2-weighted images, which demonstrated ring enhancement with gadolinium injection [
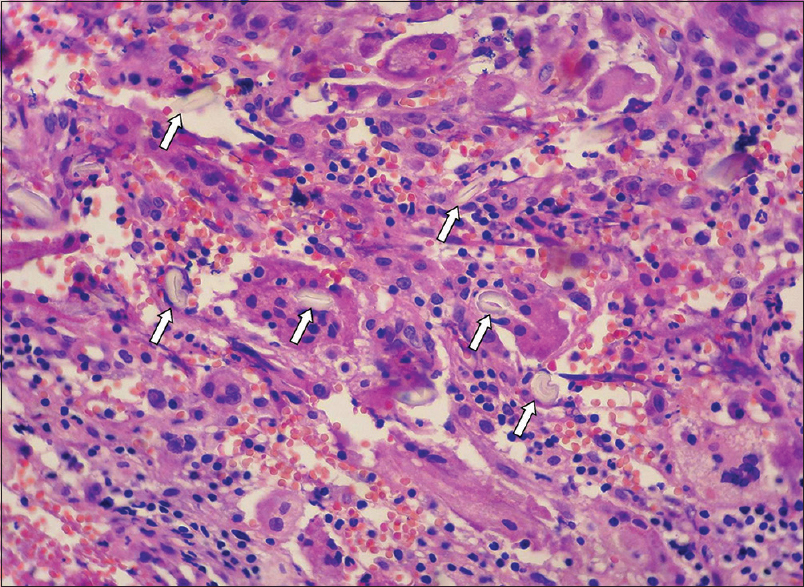
Histology
The histopathological examination confirmed a textiloma; there was chronic inflammation and fibrosis surrounding the retained cottonoid [
DISCUSSION
In this case, the spinal epidural abscess occurred 2 years after the last surgical procedure, and the patient presented with an acute cauda equina syndrome with urinary incontinence. Following a laminectomy to decompress a spinal abscess L4-S1 and resection of the retained infected cottonoid (textiloma), the infection fully resolved with 2 months of antibiotic therapy, but the paraparesis only partially resolved.
Review of textilomas
Most spinal textilomas (gossypibomas) are aseptic and are found in paraspinal areas without neurological symptoms.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akhaddar A, Boulahroud O, Naama O, Al-Bouzidi A, Boucetta M. Paraspinal textiloma after posterior lumbar surgery: A wolf in sheep's clothing. World Neurosurg. 2012. 77: 375-80
2. Akhaddar A.editors. Surgical site infections in spinal surgery. In: Atlas of Infections in Neurosurgery and Spinal surgery. Switzerland: Springer International Publishing; 2017. p. 217-28
3. Choma T, Burke M, Kim C, Kakarlapudi R. Epidural abscess as a delayed complication of spinal instrumentation in scoliosis surgery: A case of progressive neurologic dysfunction with complete recovery. Spine (Phila Pa 1976). 2008. 33: E76-80
4. Guzel Y, Polat G, Naldan ME, Ogul H, Kantarci M. Postoperative lumbar epidural abscess: Conventional and advanced magnetic resonance imaging findings. Spine J. 2015. 15: e43-5
5. Kim HS, Chung TS, Suh SH, Kim SY. MR imaging findings of paravertebral gossypiboma. AJNR Am J Neuroradiol. 2007. 28: 709-13
6. Kim YS, Lee HJ, Jeon JH, Park IJ. A 12-year-old chronic form textiloma after revision surgery for infected spinal instrumentation. Eur J Orthop Surg Traumatol. 2012. 22: S53-6
7. Tokuhashi Y, Ajiro Y, Umezawa N. Conservative follow-up after epidural abscess and diskitis complicating instrumented metal interbody cage. Orthopedics. 2008. 31: 611-