- College of Letters and Science, University of Wisconsin-Madison, Madison, Wisconsin, United States
- M.D. Program, Mayo Clinic Alix School of Medicine, Rochester, Minnesota, United States
- Department of Neurosurgery, University of Wisconsin, Madison, Wisconsin, United States.
Correspondence Address:
Amgad Hanna, Department of Neurosurgery, University of Wisconsin, Madison, Wisconsin, United States.
DOI:10.25259/SNI_822_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Vaishnavi Sribhasyam1, Shilpa Maddikunta1, Barbara Hanna2, Amgad Hanna3. Accessory head of flexor carpi radialis and abnormal course of the median nerve in the forearm. 01-Dec-2023;14:411
How to cite this URL: Vaishnavi Sribhasyam1, Shilpa Maddikunta1, Barbara Hanna2, Amgad Hanna3. Accessory head of flexor carpi radialis and abnormal course of the median nerve in the forearm. 01-Dec-2023;14:411. Available from: https://surgicalneurologyint.com/surgicalint-articles/12654/
Abstract
Background: The median nerve anatomy and its clinical presentation are crucial for surgeons to consider avoiding iatrogenic injury and performing effective surgical interventions.
Case Description: An atypical presentation of median nerve anatomy proximal to the carpal tunnel was found during cadaveric dissection. The median nerve was located deep to a uniquely double-headed flexor carpi radialis and curved medially around the tendons of the forearm to enter the carpal tunnel superficially.
Conclusion: The atypical presentation of median nerve anatomy can assist surgeons in adverse event reduction during surgeries such as carpal tunnel and pronator teres syndrome releases.
Keywords: Anatomy, Iatrogenic injury, Median nerve, Surgery, Variation
INTRODUCTION
Recognizing classical nerve anatomy is important for understanding surgical approaches, but many variations exist that require specialized attention to decrease the risk of injury during surgery. The median nerve is classically described as originating from the lateral and medial cords of the brachial plexus and, from there, coursing down the brachium without branching.[
The most common procedure involving the median nerve is carpal tunnel release. Symptoms of median nerve compression include thenar muscle atrophy and weakness with numbness and shooting pain in the first three digits. Surgery involves the release of the transverse carpal ligament surrounding and compressing the nerve.[
Procedures involving the median nerve can also occur near the elbow due to entrapment of the median nerve by the pronator teres or the sublime arch. Compression of the median nerve near the elbow often presents symptoms similar to those of carpal tunnel syndrome, though the origin is at the proximal median nerve.[
While the classical presentation of median nerve anatomy is important for understanding surgical approaches to most cases of carpal tunnel and PTSs, it is not representative of every case, as anatomical variants are often reported in the literature. Recognizing anomalies such as the one reported here is crucial, as variations may lead to complications if not well anticipated and understood. To the best of our knowledge, this variant has not been previously described in the literature.
ILLUSTRATIVE CASE
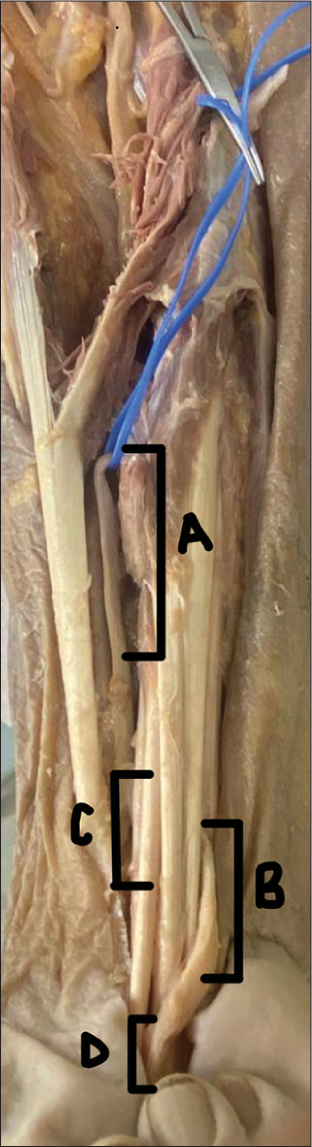
A cadaveric dissection of an elderly male’s right upper limb was performed to reveal the brachial plexus and its branching patterns. There were no apparent signs of trauma or prior surgery. Typical anatomy of the median nerve was observed at the brachial plexus. On further inspection of the proximal forearm, however, it was evident that the median nerve was not visible in its typical position, superficial to the flexor digitorium superficialis. In following the nerve, it was revealed that the median nerve lay deeper than classically described in
In addition, abnormal muscle anatomy was found. The flexor carpi radialis (FCR) had one tendinous insertion [
DISCUSSION
Observations
Carpal tunnel syndrome is the most common form of neuropathy caused by entrapment of the median nerve.[
Neuropathy of the median nerve also occurs at the elbow. Median nerve compression in the elbow is most frequent at the pronator teres.[
Lessons
Knowledge of the structures of anatomical variations before operation is critical for improving long-term success and avoiding iatrogenic injury. The median nerve during carpal tunnel release is one of the most commonly injured nerves during surgery. Median nerve injury was found to occur in 0.55% of carpal tunnel release surgeries, with 0.2–0.3% of those cases being irreparable. Anatomic variation of the nerve’s branches, division locations, and sensory and motor branches is widely accepted to be implicated in these poor surgical outcomes.[
Dag et al. did a literature review to calculate the prevalence of median nerve anomalies.[
Although iatrogenic median nerve injury in the proximal forearm is not as well studied as in the carpal tunnel, the anatomical variations presented in this case study are relevant to any procedure concerning entrapment of the median nerve. In various emergency procedures such as venous cutdown, ignorance of anatomical variations of the median nerve can lead to iatrogenic injury.[
CONCLUSION
Knowledge of proper anatomy is crucial for accurate and effective surgical approaches, and classical anatomic descriptions only represent the majority of clinical anatomical presentations. Although less common, these anomalies are prevalent in the community and require careful attention to avoid median nerve injury during carpal tunnel and PTS releases.
Ethical approval
Not applicable
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Dag F, Dirim Mete B, Gursoy M, Uluc ME. Variations ignored in routine wrist MRI reports: Prevalence of the median nerve anatomical variations and persistent median artery. Acta Radiol. 2021. 63: 76-83
2. Dididze M, Tafti D, Sherman AL, editors. Pronator teres syndrome. StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. p. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526090 [Last accessed on 2023 Oct 31]
3. Hanna AS, Wei Z, Hanna BA. Median nerve variation: A complete spin before terminal branching. J Brachial Plex Peripher Nerve Inj. 2020. 15: e1-4
4. Kansay R, Singhal A, Patil B, Malhotra A. Iatrogenic median nerve injury as a result of venous cut down procedure: A rare case report. Int J Surg Case Rep. 2020. 73: 146-9
5. Löppönen P, Hulkkonen S, Ryhänen J. Proximal median nerve compression in the differential diagnosis of carpal tunnel syndrome. J Clin Med. 2022. 11: 3988
6. Luangjarmekorn P, Tsai TM, Honsawek S, Kitidumrongsook P. Role of pronator release in revision carpal tunnel surgery. SICOT J. 2016. 2: 9
7. Mayo Clinic. Carpal tunnel syndrome. Available from: https://www.mayoclinic.org/diseases-conditions/carpal-tunnel-syndrome/symptoms-causes/syc-20355603 [Last accessed on 2022 Jun 15].
8. Miller TT, Reinus WR. Nerve entrapment syndromes of the elbow, forearm, and wrist. AJR Am J Roentgenol. 2010. 195: 585-94
9. Moore KL, Dalley AF, Agur AM, editors. Clinically oriented anatomy. Baltimore, MD: Lippincott Williams and Wilkins; 2014. p.
10. Pederson WC. Median nerve injury and repair. J Hand Surg Am. 2014. 39: 1216-22
11. Sevy JO, Varacallo M, editors. Carpal tunnel syndrome. StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. p.
12. Sharp E, Roberts M, Żurada-Zielińska A, Zurada A, Gielecki J, Tubbs RS. The most commonly injured nerves at surgery: A comprehensive review. Clin Anat. 2020. 34: 244-62