- Department of Neurosurgery, Sir Sunderlal Hospital, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India
- Department of Pathology, Sir Sunderlal Hospital, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India
Correspondence Address:
Sharad Pandey
Department of Pathology, Sir Sunderlal Hospital, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India
DOI:10.4103/2152-7806.174890
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Singh K, Pandey S, Gupta PK, Sharma V, Santhosh D, Ghosh A. Acquired dorsal intraspinal epidermoid cyst in an adult female. Surg Neurol Int 25-Jan-2016;7:
How to cite this URL: Singh K, Pandey S, Gupta PK, Sharma V, Santhosh D, Ghosh A. Acquired dorsal intraspinal epidermoid cyst in an adult female. Surg Neurol Int 25-Jan-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/acquired-dorsal-intraspinal-epidermoid-cyst-in-an-adult-female/
Abstract
Background:Epidermoid and dermoid cyst comprise
Case Description:Here, we report the a case of an acquired intradural extramedullary epidermoid cyst involving the thoracic region in an adult female who had no associated history of an accompanying congenital spinal deformity.
Conclusion:Early diagnosis and immediate surgical intervention reduce patient morbidity. Near complete or subtotal excision of the cyst wall is warranted to prevent inadvertent injury to the spinal cord thus minimizing neurological morbidity.
Keywords: Acquired, congenital, epidermoid cysts, spinal tumors
BACKGROUND
Epidermoid cysts within the neuraxis are rare benign neoplasms that are commonly located intracranially. They account for <1% of all intraspinal tumors.[
CASE DESCRIPTION
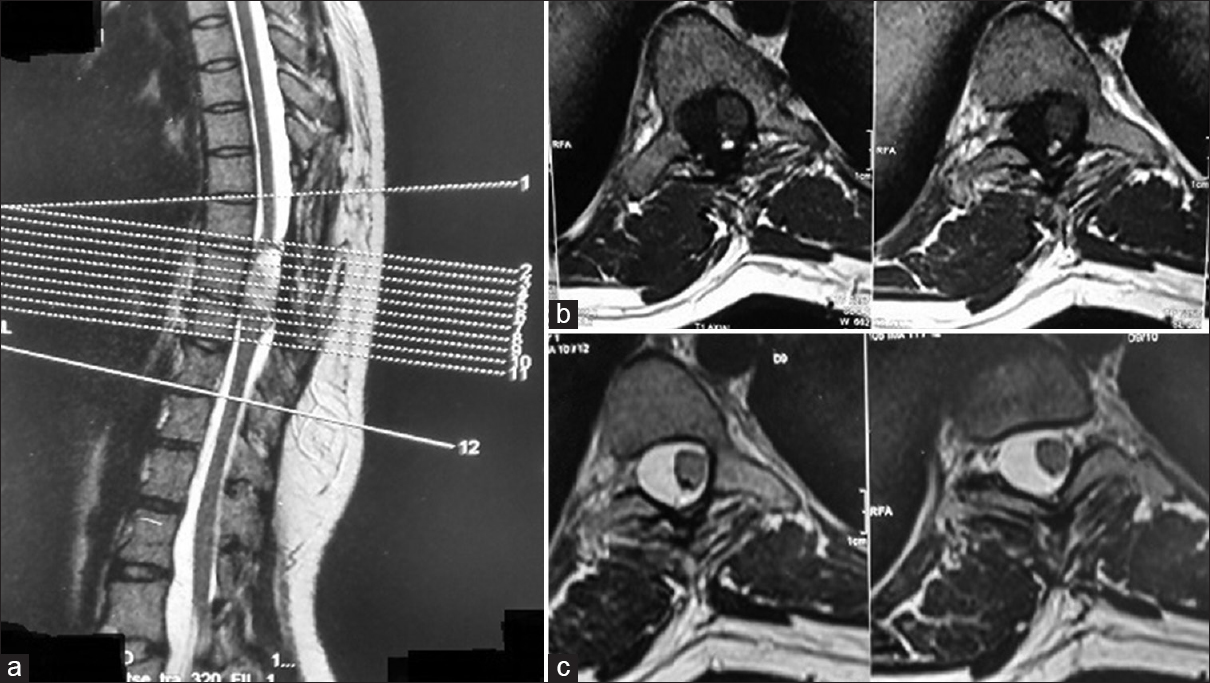
A 20-year-old female presented with a progressive thoracic myelopathy (numbness/difficulty in walking) of 5–6 months duration; she previously underwent some type of thoracic surgery (e.g., thoracic spine scar). Her neurological examination showed loss of motor function at the 3/5 levels in both legs accompanied by numbness in both legs. The thoracic magnetic resonance imaging (MRI) showed a well-defined intradural extramedullary mass on the right side of the spinal canal markedly compressing the cord extending from the D7/D8 to the D8/D9 levels (measuring approximately 3 cm × 1.7 cm × 1.5 cm). The tumor was isointense to hypointense on T1-weighted images, and hyperintense on T2-weighted studies [
Figure 1
(a) Magnetic resonance imaging dorsolumbar spine showing well-defined intradural extramedullary mass lesion on the right side of the spinal canal extending from the D7/D8 to D8/D9 levels. (b) Magnetic resonance imaging showing isointense to hypointense mass lesion with signal intensity nearly comparable to the cord (e.g., isointense) on T1-weighted images (c) Magnetic resonance imaging showing hyperintense signal intensity of the lesion on T2-weighted images with associated mass effects
DISCUSSION
Frequency spinal epidermoid tumors
In adults, epidermoids more commonly affect the cranium versus the spine (ratio 6:1).[
Location of spinal epidermoid tumors
Spinal dermoids can be extradural, intradural extramedullary, or intramedullary. The most common site of occurrence of these tumors is the lumbosacral region (60%), followed by the thoracic (10%), and cervical regions (5%).
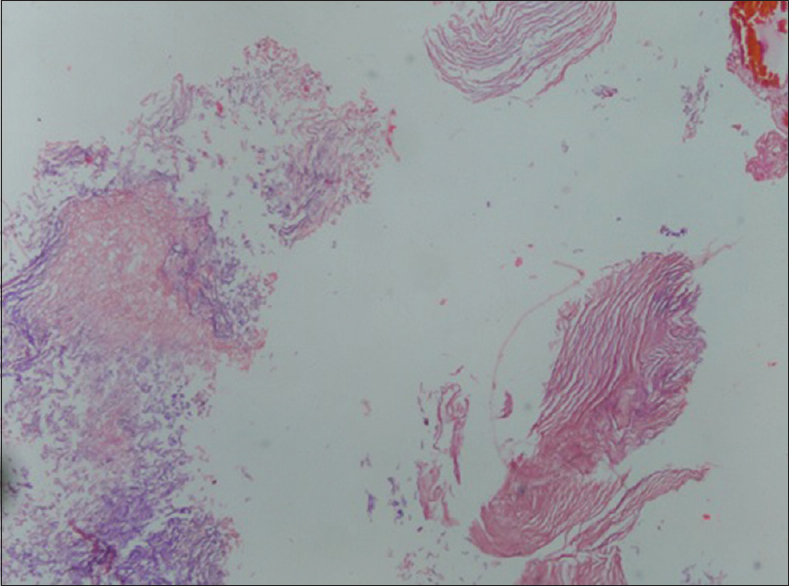
Histopathology of epidermoid/dermoid tumor
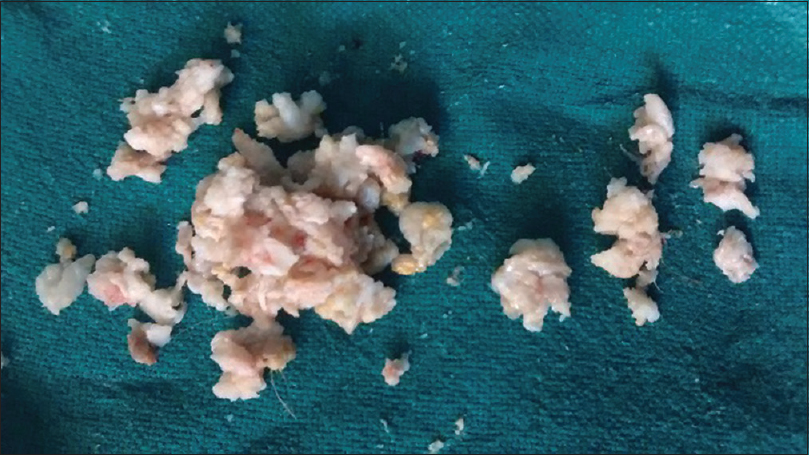
The histopathology of dermoid and epidermoid cysts is usually based on their typical contents. Classically, they are lined by stratified squamous epithelium supported by an outer layer of collagenous tissue with a soft white material toward the interior of the cyst as a result of progressive desquamation of keratin from epithelial lining.[
Magnetic resonance imaging findings for epidermoid tumors
Preoperative MRI using fat-suppressed sequences for these lesions usually demonstrate homogenous intensity combined with heterogeneous intensity. Sometimes calcification is also seen in the walls with hair and cartilaginous tissue.[
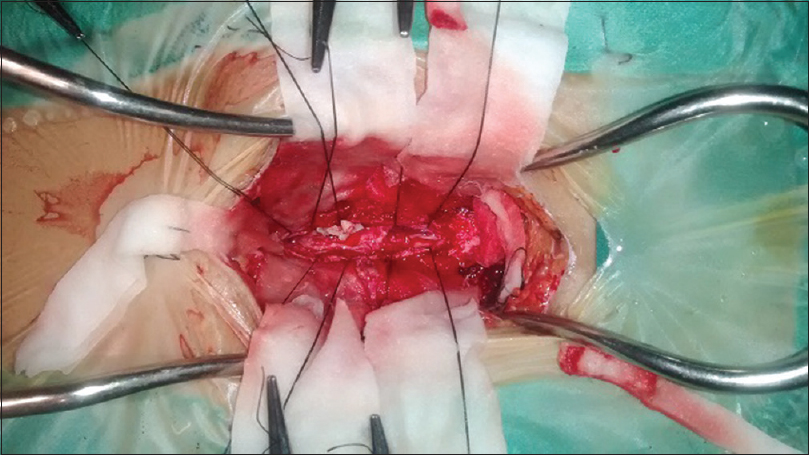
Surgical recommendation: Early gross total excision
The mainstay of treatment for these lesions is gross total surgical excision. If there is adherence of the cyst wall to critical neural elements partial resection will suffice, resulting in a low recurrence rates (10% or less).[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Amato VG, Assietti R, Arienta C. Intramedullary epidermoid cyst: Preoperative diagnosis and surgical management after MRI introduction. Case report and updating of the literature. J Neurosurg Sci. 2002. 46: 122-6
2. Baba H, Wada M, Tanaka Y, Imura S, Tomita K. Intraspinal epidermoid after lumbar puncture. Int Orthop. 1994. 18: 116-8
3. Ferrara P, Costa S, Rigante D, Mule A, D’Aleo C, Pulitanò S. Intramedullary epidermoid cyst presenting with abnormal urological manifestations. Spinal Cord. 2003. 41: 645-8
4. Kumar S, Gulati DR, Mann KS. Intraspinal dermoids. Neurochirurgia (Stuttg). 1977. 20: 105-8
5. Lunardi P, Missori P, Gagliardi FM, Fortuna A. Long-term results of the surgical treatment of spinal dermoid and epidermoid tumors. Neurosurgery. 1989. 25: 860-4
6. Pandey S, Sharma V, Shinde N, Ghosh A. Spinal intradural extramedullary mature cystic teratoma in an adult: A rare tumor with review of literature. Asian J Neurosurg. 2015. 10: 133-7
7. Park JC, Chung CK, Kim HJ. Iatrogenic spinal epidermoid tumor. A complication of spinal puncture in an adult. Clin Neurol Neurosurg. 2003. 105: 281-5
8. Roux A, Mercier C, Larbrisseau A, Dube LJ, Dupuis C, Del Carpio R. Intramedullary epidermoid cysts of the spinal cord. Case report. J Neurosurg. 1992. 76: 528-33
9. Scarrow AM, Levy EI, Gerszten PC, Kulich SM, Chu CT, Welch WC. Epidermoid cyst of the thoracic spine: Case history. Clin Neurol Neurosurg. 2001. 103: 220-2