- Spinal Disorders Center, Fujieda Heisei Memorial Hospital, Fujieda, Japan.
Correspondence Address:
Koki Mitani, Spinal Disorders Center, Fujieda Heisei Memorial Hospital, Fujieda, Japan.
DOI:10.25259/SNI_740_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Koki Mitani, Manabu Minami, Toshiyuki Takahashi, Mariko Toyoda, Ryo Kanematsu, Junya Hanakita. Acute cervical epidural abscess with concurrent calcium pyrophosphate deposition after cervical spinal surgery: A case report. 15-Mar-2024;15:87
How to cite this URL: Koki Mitani, Manabu Minami, Toshiyuki Takahashi, Mariko Toyoda, Ryo Kanematsu, Junya Hanakita. Acute cervical epidural abscess with concurrent calcium pyrophosphate deposition after cervical spinal surgery: A case report. 15-Mar-2024;15:87. Available from: https://surgicalneurologyint.com/surgicalint-articles/12801/
Abstract
Background: Spinal epidural abscess (SEA) is a rare condition that may result in catastrophic outcomes. On the other hand, calcium pyrophosphate (CPP) deposition disease (CPPD) causes inflammatory arthritis. Spinal involvement of a crystal-induced inflammation caused by CPPD is also common. Surgery is a common risk factor for both SEA and CPPD; however, the postoperative acute onset of SEA complicated with CPPD is extremely rare.
Case Description: A man in his 70s presented to our hospital, complaining of right upper limb weakness, loss of dexterity, and gait disturbance. The diagnosis of cervical spondylotic myelopathy was made, and he performed laminectomy at C3, C4, and C5 levels. Four days after the laminectomy, he suffered from acute neck pain, weakness, and hypoesthesia in his arms and legs. Magnetic resonance imaging revealed a mass occupying the dorsal epidural space of C6 and C7, compressing the cervical spinal cord. Considering the acute symptomatology, an acute spinal epidural hematoma after surgery was suspected; therefore, emergency C6 and C7 laminectomy was performed. Surgical findings indicated that the pressure inside the spinal canal was elevated, and the mass was purulent exudate. Pathological examination showed suppurative inflammation with concomitant deposition of CPP. SEA complicated with CPPD was considered; therefore, antibiotics and non-steroidal anti-inflammatory drugs were administered. The motor weakness and hypoesthesia were improved despite a slight residual deficit in his dexterity.
Conclusion: An acute onset of SEA complicated with CPPD after cervical surgery has rarely been reported. The suppurative inflammation fostered by the crystal-induced inflammation may account for the acute symptomatology.
Keywords: Calcium pyrophosphate deposition disease, Chondrocalcinosis, Epidural abscess, Pseudogout, Surgical site infection
INTRODUCTION
Spinal epidural abscess (SEA) is a rare disease, but the early diagnosis of SEA is mandatory due to its potentially fatal outcome. Since the recent advent of imaging techniques enabled us to detect SEA with high sensitivity, the prevalence of SEA is increasing. However, mortality and the rate of the neurologically poor sequelae of SEA remain high.[
On the other hand, calcium pyrophosphate deposition disease (CPPD) causes crystal-induced arthritis mimicking gout. The patients typically presented with the acute onset of mono- or oligoarticular arthritis and constitutional symptoms in the inflammatory response to calcium pyrophosphate (CPP) crystals.[
Although a surgical invasion is known to be followed by SEA and CPPD, the acute onset of which after the surgery has been rarely reported.
CASE DESCRIPTION
A man in his 70s presented with a weakness in the right arm, loss of dexterity, and gait disturbance for one month. As the symptoms gradually worsened, the patient came to our department. His medical history included hypertension and hypercholesterolemia. He was an immunocompetent host and did not take any oral antithrombotic medication. Magnetic resonance imaging revealed cervical spinal canal stenosis at the level of C3/4 and C4/5 without ossification of the posterior longitudinal ligament and yellow ligament, and there is no evidence of cervical spinal instability [
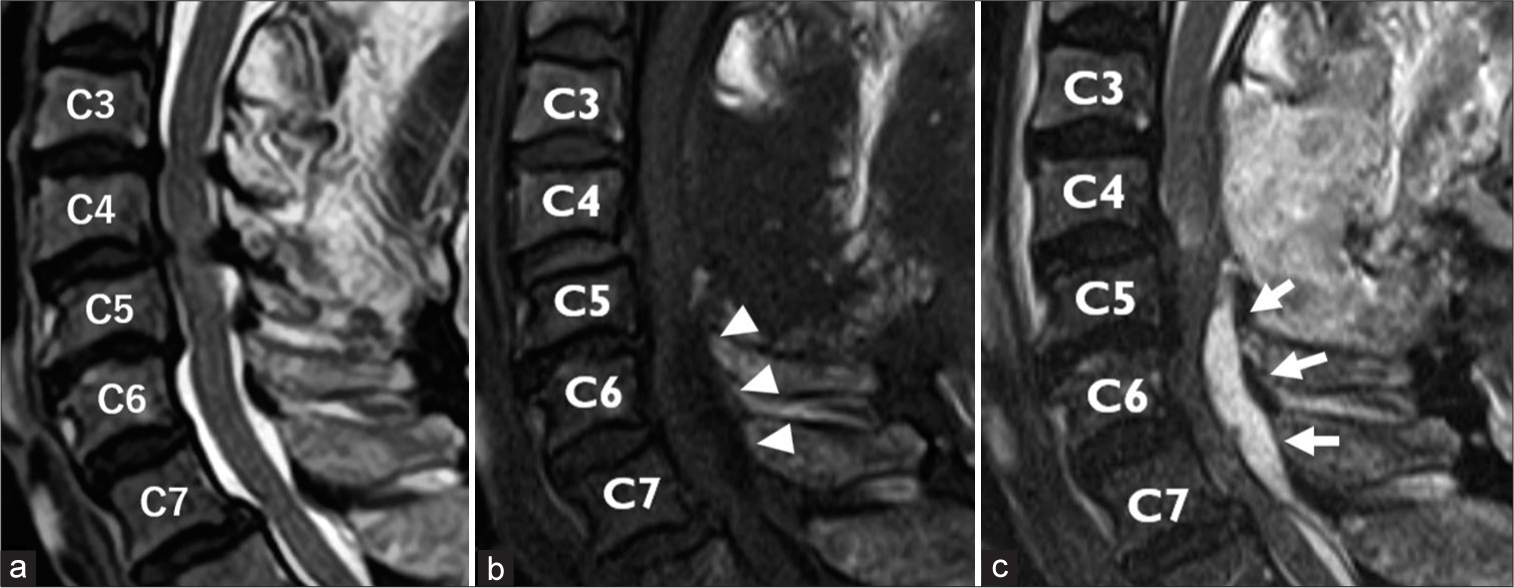
Figure 1:
Magnetic resonance image before and after the surgery. (a) Cervical spinal stenosis was found in the T2-weighted image, sagittal section, and the diagnosis of cervical spondylosis was made; therefore, the patient performed the C3 to C5 laminectomy. (b) Four days after the surgery, the mass occupying the dorsal epidural space (arrowhead) was well demarcated and low-intensity in T1-weighted and (c) homogeneously hyper-intensity in T2-weighted image (arrow).
Magnetic resonance imaging showed a mass located in the dorsal epidural space at C6 and C7 levels, which we did not manipulate during the surgery. The mass was well-demarcated, low-intensity in T1-weighted, and homogeneously hyperintensity in T2-weighted image [
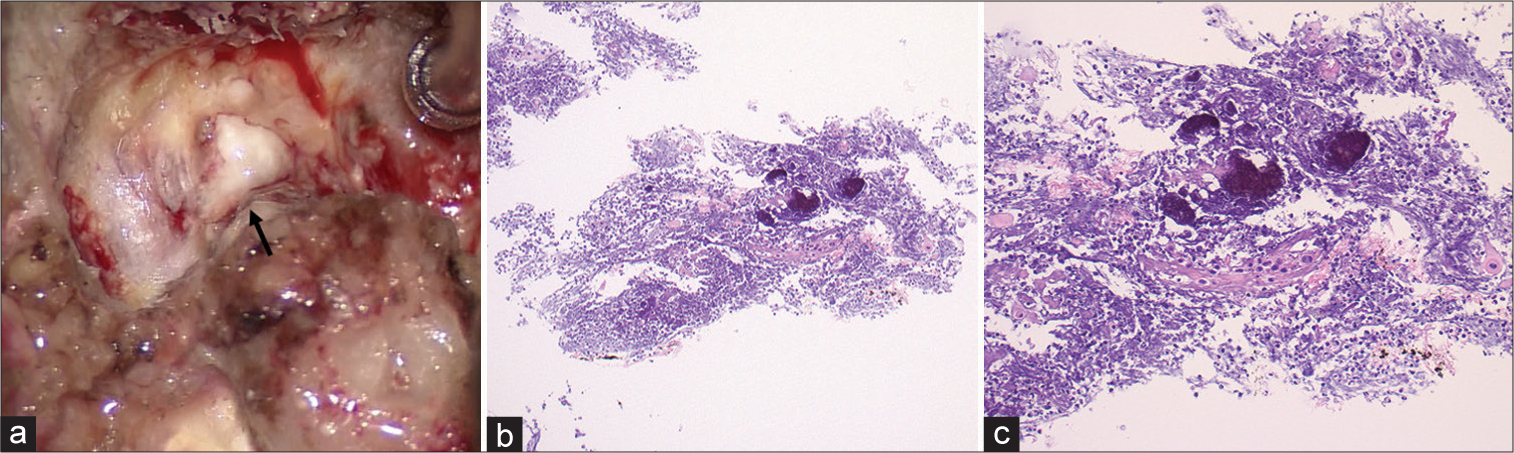
Figure 2:
(a) Intraoperative finding. After the laminectomy of C7, a purulent, whitish exudate (arrow) erupted from the thinned cortical bone; Hematoxylin and eosin stain showed the infiltration of neutrophils and the small clusters of weak birefringent, basophilic crystals compatible with calcium pyrophosphate deposition. (b) Low- (× 40), and (c) high-magnification (× 100).
DISCUSSION
SEA is characterized by pus accumulation in the epidural space, causing spinal cord compression and neurological deficit. The diagnosis of SEA is difficult, and the treatment is prone to be delayed.[
On the other hand, CPPD is characterized as the crystal deposition in several joints, causing joint pain and constitutional symptoms. CPPD commonly involves the large joints such as knees, wrists, shoulders, and hips, but it also involves the spine.[
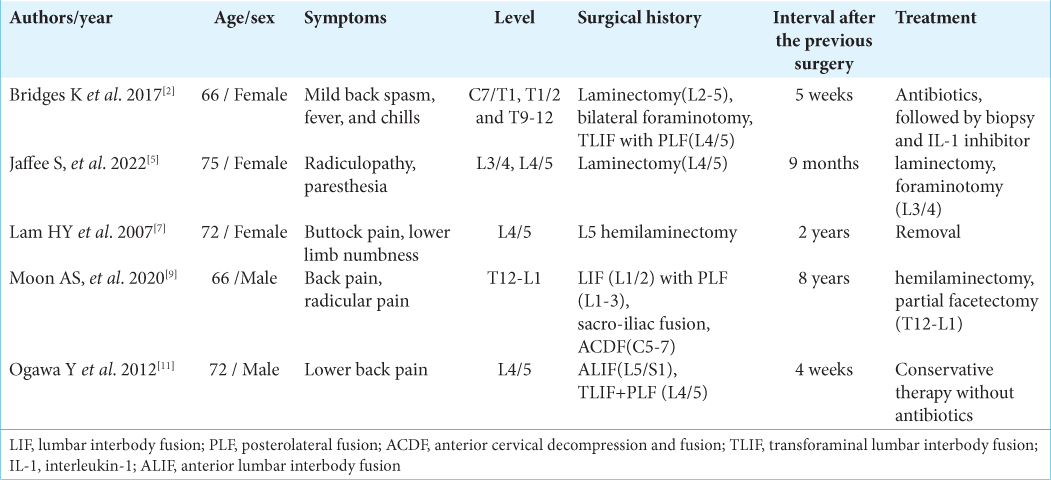
The present patient complained of neck pain and neurological symptoms immediately after the surgery for cervical spondylotic myelopathy, suggesting cervical spinal cord compression. Although a surgical procedure is the common predisposing factor of SEA and CPPD, the acute onset of 4 days of SEA and CPPD after the preceding surgery has been rarely reported. The interval time between the onset of SEA and the spinal surgery has not been well investigated. Literally reviewed, five cases of CPPD after the spinal surgery were reported, and the interval time after the surgical procedure ranged from 4 weeks to 8 years; however, acute onset within a week has not been reported [
CONCLUSION
A case of acute epidural abscess suspected of epidural hematoma after cervical laminectomy was reported. The acute onset of SEA complicated with CPPD after cervical spinal surgery has rarely been reported. The crystal-induced inflammation of the CPP could amplify the pyogenic inflammation.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Al-Hourani K, Al-Aref R, Mesfin A. Upper cervical epidural abscess in clinical practice: Diagnosis and management. Global Spine J. 2016. 6: 383-93
2. Bridges KJ, Bullis CL, Wanchu A, Than KD. Pseudogout of the cervical and thoracic spine mimicking infection after lumbar fusion: Case report. J Neurosurg Spine. 2017. 27: 145-9
3. Darouiche RO. Spinal epidural abscess. N Engl J Med. 2006. 355: 2012-20
4. Ehioghae M, Lawlor MC, Mesfin A. Calcium pyrophosphate dihydrate of the ligamentum flavum in the cervical spine-a review of the literature. Surg Neurol Int. 2022. 13: 470
5. Jaffee S, Jeong SW, Dabecco R, Elhamdani S, Yu A. Pseudogout, an unconventional imitator of the lumbosacral spine with associated chronic epidural hematoma: Illustrative cases. J Neurosurg Case Lessons. 2022. 3: CASE21571
6. Kinoshita T, Maruoka S, Yamazaki T, Sakamoto K. Tophaceous pseudogout of the cervical spine: MR imaging and bone scintigraphy findings. Eur J Radiol. 1998. 27: 271-3
7. Lam H, Cheung K, Law S, Fung K. Crystal arthropathy of the lumbar spine: A report of 4 cases. J Orthop Surg. 2007. 15: 94-101
8. Lu YH, Lin HH, Chen HY, Chou PH, Wang ST, Liu CL. Multilevel calcium pyrophosphate dihydrate deposition in cervical ligamentum flavum: Clinical characteristics and imaging features. BMC Musculoskelet Disord. 2021. 22: 929
9. Moon AS, Mabry S, Pittman JL. Calcium pyrophosphate deposition disease of the cervical and thoracolumbar spine: A report of two cases. N Am Spine Soc J. 2020. 3: 100026
10. Muthukumar N, Karuppaswanny U, Sonntag VK, Traynelis VC, Benzel EC, Haid RW. Tumoral calcium pyrophosphate dihydrate deposition disease of the ligamentum flavum. Neurosurgery. 2003. 53: 103-9
11. Ogawa Y, Nagatsuma M, Kubota G, Inoue G, Eguchi Y, Orita S. Acute lumbar spinal pseudogout attack after instrumented surgery. Spine (Phila Pa 1976). 2012. 37: 1529-33
12. Rosenthal AK, Ryan LM. Calcium pyrophosphate deposition disease. N Engl J Med. 2016. 374: 2575-84
13. Sharfman ZT, Gelfand Y, Shah P, Holtzman AJ, Mendelis JR, Kinon MD. Spinal epidural abscess: A review of presentation, management, and medicolegal implications. Asian Spine J. 2020. 14: 742-59
14. Tetsuka S, Suzuki T, Ogawa T, Hashimoto R, Kato H. Spinal epidural abscess: A review highlighting early diagnosis and management. JMA J. 2019. 3: 29-40