- Department of Emergency Neurosurgery, Pescara Hospital, Pescara, Abruzzo, Italy.
- Department of Pathology, Pescara Hospital, Pescara, Abruzzo, Italy.
Correspondence Address:
Giada Toccaceli
Department of Emergency Neurosurgery, Pescara Hospital, Pescara, Abruzzo, Italy.
DOI:10.25259/SNI_878_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Raffaele Nigro1, Antonio Alessandro Scogna1, Daniele Intraina1, Giada Toccaceli1, Alfio Ieraci2, Donato Carlo Zotta1. Acute onset of paraplegia due to melanocytic cervicodorsal lesion. 20-Jan-2021;12:21
How to cite this URL: Raffaele Nigro1, Antonio Alessandro Scogna1, Daniele Intraina1, Giada Toccaceli1, Alfio Ieraci2, Donato Carlo Zotta1. Acute onset of paraplegia due to melanocytic cervicodorsal lesion. 20-Jan-2021;12:21. Available from: https://surgicalneurologyint.com/surgicalint-articles/10537/
Abstract
Background: Melanocytomas are rare pigmented tumors of the central nervous system (CNS). They are more frequent in females in their fifties and are typically benign, but locally aggressive lesions that very are rarely found in the spine. They can occur in all the age groups.
Case Description: A 62-year-old male presented with acute paraplegia a attributed to a C7-T1 intradural extramedullary melanocytoma. Urgent surgery, consisting of subtotal removal of the lesion, resulted in subtotal recovery of motor function with full resolution of his sensory deficit. Histologically, the lesion proved to be a melanocytoma.
Conclusion: Rarely, patients with intradural extramedullary melanocytomas of the spine may present with acute paralytic deficits warranting emergent surgical intervention.
Keywords: Melanocytoma, Paraplegia, Primary spinal tumor, Spinal cord
INTRODUCTION
Melanocytomas are rare pigmented tumors originating from leptomeningeal melanocytes. They are benign lesions that infrequently occur in the spine, where they may cause acute radiculopathy and/or myelopathy. In this case, a 62-year-old male acutely presented with paraplegia attributed to a C7-T1 intradural extramedullary anterior melanocytoma.
CASE PRESENTATION
Clinical and surgical history
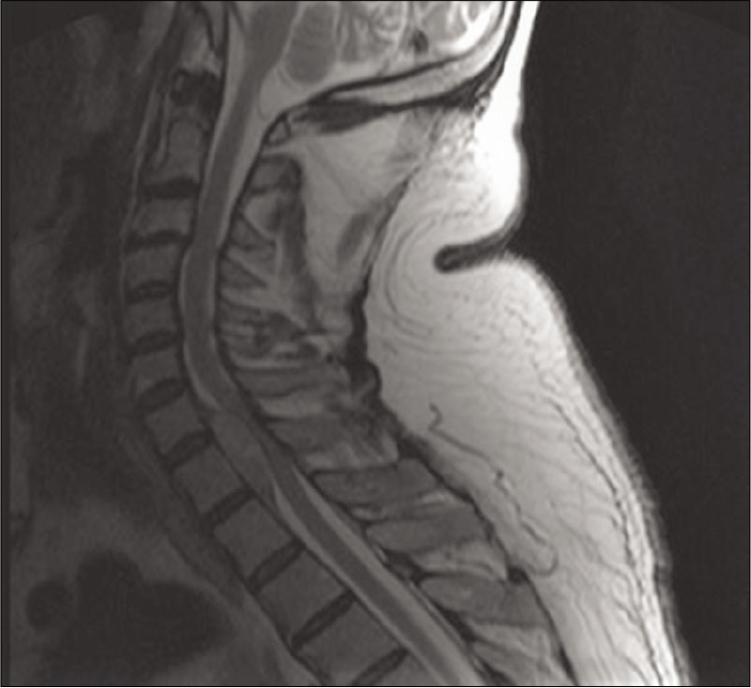
A 62-years-old male, with a 2 months history of interscapular pain, presented with acute T2-level paraplegia. The MRI showed an intradural extramedullary well-defined mass at the C7-T1 level located anterior to the spinal cord. The T2-weighted image demonstrated an isointense lesion with a wide dural attachment while the enhanced study demonstrated heterogeneous enhancement with compression and posterior displacement of the cord [
An emergent decompressive C7-T1 laminectomy was performed and achieved subtotal tumor removal. Intraoperatively, the cervicodorsal dura was blackened, and the lesion was firm.
Histopathology
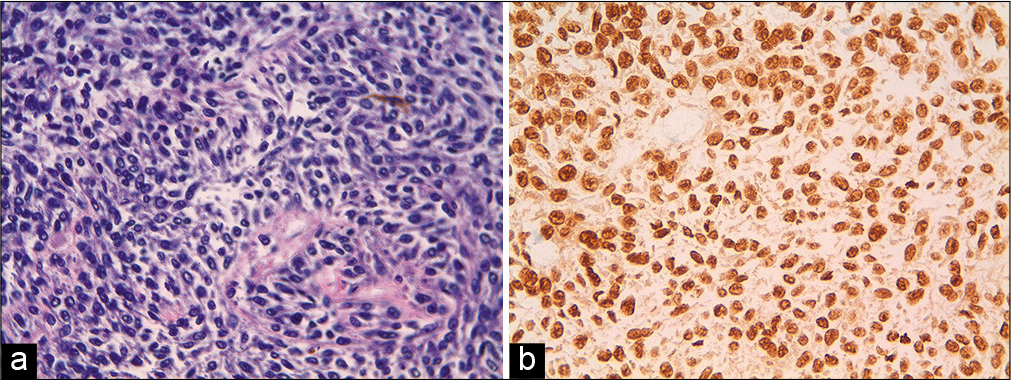
The histopathologic examination revealed large cells, oval to polygonal in shape with prominent nucleoli, and eosinophilic cytoplasm filled with melanin pigment. There was no significant increase in mitosis (1/10 HPF and low proliferation index Ki 67: 2%). On immunohistochemistry tumor cells showed positivity with S100, Vimentin and HBM45 and negativity for EMA (which is an indicator of meningioma), thus confirming the diagnosis of melanocytoma [
Postoperative course
The 1 day post-operative MRI revealed removal of the 90% of the lesion and no residual compression of the cervicothoracic cord at the same level. After the 1st postoperative week, he demonstrated subtotal recovery of motor (4/5 BMRC grade) and total sensory recovery of function. He was discharged in a rehabilitation unit. Three months later, the patient’s neurological status was improved (5/5 BMRC) and he is being referred for radiation therapy.
DISCUSSION
The World Health Organization’s classification classifies primary melanocytic lesions into four categories; meningeal melanocytosis, meningeal melanocytoma, meningeal melanoma, and meningeal melanomatosis.[
CONCLUSION
In the presence of spinal cord compression due to intradural extramedullary lesion with acute neurological onset, the surgical decompression and the removal of the lesion, despite subtotal, are necessary to achieve a good neurological outcome.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Eskandari R, Schmidt MH. Intramedullary spinal melanocytoma. Rare Tumors. 2010. 2: e24
2. Jayamma SS, Sud S, Buxi T, Madan VS, Goyal A, Dhawan S. Cervical spinal meningeal melanocytoma presenting as intracranial superficial siderosis. Case Rep Radiol. 2015. 2015: 674868
3. Louis DN, Perry A, Reifenberger G, von Deimling A, FigarellaBranger D, Cavenee WK. The 2016 World Health Organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016. 131: 803-20
4. Sen R, Sethi D, Goyal V, Duhan A, Modi S. Spinal meningeal melanocytoma. Asian J Neurosurg. 2011. 6: 110-2
5. Tateyama M, Fujimoto T, Nakamura T, Miyamoto T. Meningeal melanocytoma occurring at epidural region of the cervical spine. Spine Surg Relat Res. 2020. 4: 377-9
6. Xie S, Jiang Z. Primary spinal cord melanocytoma: A case report and review of literature. Int J Clin Exp Pathol. 2019. 12: 669-73