- Department of Neurosurgery, Fukushima Medical University, 1 Hikarigaoka, Fukushima, Japan
Correspondence Address:
Ryo Hiruta
Department of Neurosurgery, Fukushima Medical University, 1 Hikarigaoka, Fukushima, Japan
DOI:10.25259/SNI-235-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ryo Hiruta, Shinya Jinguji, Taku Sato, Yuta Murakami, Mudathir Bakhit, Yosuke Kuromi, Keiko Oda, Masazumi Fujii, Jun Sakuma, Kiyoshi Saito. Acute paradoxical brain herniation after decompressive craniectomy for severe traumatic brain injury: A case report. 10-May-2019;10:79
How to cite this URL: Ryo Hiruta, Shinya Jinguji, Taku Sato, Yuta Murakami, Mudathir Bakhit, Yosuke Kuromi, Keiko Oda, Masazumi Fujii, Jun Sakuma, Kiyoshi Saito. Acute paradoxical brain herniation after decompressive craniectomy for severe traumatic brain injury: A case report. 10-May-2019;10:79. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=9314
Abstract
Background:Sinking skin flap syndrome or paradoxical brain herniation is an uncommon neurosurgical complication, which usually occurs in the chronic phase after decompressive craniectomy. We report a unique case presenting with these complications immediately after decompressive craniectomy for severe traumatic brain injury.
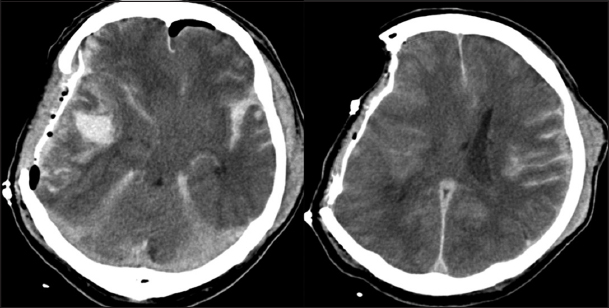
Case Description:A 65-year-old man had a right acute subdural hematoma (SDH), contusion of the right temporal lobe, and diffuse traumatic subarachnoid hemorrhage with midline shift to the left side. He underwent an emergency evacuation of the right SDH with a right decompressive frontotemporal craniectomy. Immediately after the operation, his neurological and computed tomography (CT) findings had improved. However, within 1 h after the surgery, his neurological signs deteriorated. An additional follow-up CT showed a marked midline shift to the left, i.e., paradoxical brain herniation, and his skin flap overlying the decompressive site was markedly sunken. We immediately performed an urgent cranioplasty with the right temporal lobectomy. He responded well to the procedure. We suspected that a cerebrospinal fluid leak had caused this phenomenon.
Conclusion:Decompressive craniectomy for severe traumatic brain injury can lead to sinking skin flap syndrome and/or paradoxical brain herniation even in the acute phase. We believe that immediate cranioplasty allows the reversal of such neurosurgical complications.
Keywords: Paradoxical brain herniation, Traumatic brain injury, Decompressive craniectomy, Intracranial hypotension, Neurosurgery
INTRODUCTION
Sinking skin flap syndrome, also known as “syndrome of the trephined,” is an uncommon complication after decompressive craniectomy. This condition involves sinking of the scalp on the decompressed side deep beyond the edges of the bone defect.[
CASE REPORT
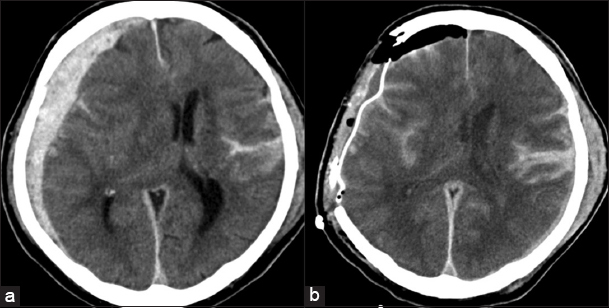
A 65-year-old man was found unconscious with bleeding from a left side scalp wound at the bottom of the stairs in his house where he seemed to have fallen down. On arrival at the hospital, his Glasgow Coma Scale (GCS) score was 5 (E1V1M3) without anisocoria. He had a laceration in his left frontotemporal scalp but presented with no other injuries on his trunk or extremities. There were no apparent findings of cerebrospinal fluid (CSF) leakage. However, within 20 min of arrival at the hospital, the diameter of his right pupil changed from 3 mm to 6 mm, although that of the left pupil remained 3 mm. He was immediately intubated. A plain brain computed tomography (CT) showed a right acute subdural hematoma (SDH), contusion of the right temporal lobe, traumatic subarachnoid hemorrhage, and midline shift to the left side [
Figure 1
(a) Axial plain of brain computed tomography obtained before the initial surgery showing a right acute subdural hematoma, brain contusion, traumatic subarachnoid hemorrhage, and midline shift to the left side measuring approximately 1.5 cm in thickness. (b) Axial plain brain computed tomography obtained right after the initial surgery showing decompressive right frontotemporal craniectomy and improvement of the midline shift.
After the operation, his anisocoria improved: the right pupil was 3 mm and the left pupil was 1.5 mm, and plain brain CT showed a regression of the mass effect and midline shift [
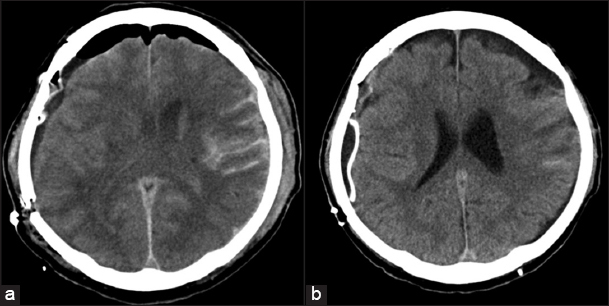
Figure 4
(a) Axial plain brain computed tomography obtained right after the second surgery showing improvement and resolution of the midline shift, which was recognized after the initial surgery. (b) Axial plain brain computed tomography obtained 14 days after the second surgery showing no additional abnormal findings compared to that obtained after the second surgery.
A follow-up CT scan 2 weeks later showed complete resolution of the midline shift [
DISCUSSION
In the present case, we performed decompressive craniectomy to treat a severe head injury. However, the patient experienced paradoxical brain herniation in the immediate postoperative period. We suspected that his serious condition was similar to sinking skin flap syndrome and, therefore, performed an immediate cranioplasty. The patient responded to the treatment well and showed no further deterioration.
In many cases of severe brain injury that requires decompressive craniectomy, brain swelling may occur toward the decompressed area due to the elevating intracranial pressure of the injured brain.[
The first step of treatment for sinking skin flap syndrome or paradoxical brain herniation is similar to that of treatment for intracranial hypotension, i.e., correction of the intracranial pressure, which is exceeded by extracranial pressure.[
It is generally agreed on that cranioplasty is the definitive treatment for sinking skin flap syndrome and paradoxical brain herniation.[
Although craniotomy and decompressive craniectomy are both used in acute SDH, yet it is not clear which one is the most appropriate. The decision to perform a decompressive craniectomy is usually based on the personal judgment of the neurosurgeons.[
CONCLUSION
A decompressive craniectomy for a severe traumatic brain injury may induce “acute paradoxical brain herniation,” and may lead to sudden neurological deterioration. Although such situations are infrequent, we suggest that immediate cranioplasty is required to improve such complications as well as to prevent further implications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understanding that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akins PT, Guppy KH. Sinking skin flaps, paradoxical herniation, and external brain tamponade:A review of decompressive craniectomy management. Neurocrit Care. 2008. 9: 269-76
2. Annan M, De Toffol B, Hommet C, Mondon K. Sinking skin flap syndrome (or Syndrome of the trephined):A review. Br J Neurosurg. 2015. 29: 314-8
3. Ashayeri K, Jackon EM, Huang J, Brem H, Gordon CR. Syndrome of the trephined:A systematic review. Neurosurgery. 2016. 79: 525-34
4. Bor-Seng-Shu E, Figueiredo EG, Amorim RL, Teixeira MJ, Valbuza JS, de Oliveira MM. Decompressive craniectomy:A meta-analysis of influences on intracranial pressure and cerebral perfusion pressure in the treatment of traumatic brain injury. J Neurosurg. 2012. 117: 589-96
5. Creutzfeldt CJ, Vilela MD, Longstreth WT. Paradoxical herniation after decompressive craniectomy provoked by lumbar puncture or ventriculoperitoneal shunting. J Neurosurg. 2015. 123: 1170-5
6. Fields JD, Lansberg MG, Skirboll SL, Kurien PA, Wijman CA. “Paradoxical” transtentorial herniation due to CSF drainage in the presence of a hemicraniectomy. Neurology. 2006. 67: 1513-4
7. Hasheminia D, Motamedi MR, Hashemzehi H, Nazeri R, Movahedian B. A 7-year study of 1,278 patients with maxillofacial trauma and cerebrospinal fluid leak. J Maxillofac Oral Surg. 2015. 14: 258-62
8. Ji H, Chen W, Yang X, Guo J, Wu J, Huang M. Paradoxical herniation after unilateral decompressive craniectomy:A retrospective analysis of clinical characteristics and effectiveness of therapeutic measures. Turk Neurosurg. 2017. 27: 192-200
9. Muehlschlegel S, Voetsch B, Sorond FA. Emergent epidural blood patch:Lifesaving treatment of paradoxical herniation. Arch Neurol. 2009. 66: 670-1
10. Phan K, Moore JM, Griessenauer C, Dmytriw AA, Scherman DB, Sheik-Ali S. Craniotomy versus decompressive craniectomy for acute subdural hematoma:Systematic review and meta-analysis. World Neurosurg. 2017. 101: 677-85
11. Ramos-Zuniga R, Mares-Pais R, Gutierrez-Avila O, Saldana-Koppel DA. Paradoxical herniation in the postcraniectomy syndrome:Report and literature update. J Neurol Surg Rep. 2016. 77: e035-8
12. Rush B, Rousseau J, Sekhon MS, Griesdale DE. Craniotomy versus craniectomy for acute traumatic subdural hematoma in the United States:A national retrospective cohort analysis. World Neurosurg. 2016. 88: 25-31
13. Sarrafzadeh AS, Hopf SA, Gautschi OP, Narata AP, Schaller K. Intracranial hypotension after trauma. Springerplus. 2014. 3: 153-
14. Watanabe J, Maruya J, Nishimaki K. Sinking skin flap syndrome after unilateral cranioplasty and ventriculoperitoneal shunt in a patient with bilateral decompressive craniectomy. Interdiscip Neurosurg. 2016. 5: 6-8
15. Yamaura A, Sato M, Meguro K, Nakamura T, Uemura K. Cranioplasty following decompressive craniectomy analysis of 300 cases. No Shinkei Geka. 1977. 5: 345-53