- Department of Neurosurgery Mayo Clinic, Rochester, Minnesota, United States
- Global Neurosurgical Alliance, Rochester, Minnesota, United States
- Department of Neurology, Mayo Clinic, Rochester, Minnesota, United States
- Pittsburgh Mercy Health System, Operation Safety Net, Pittsburgh, Pennsylvania, United States
- Department of Neurosurgery, University of Arizona, Tucson, Arizona, United States.
Correspondence Address:
Albert Alan, Department of Neurosurgery Mayo Clinic, Rochester, Minnesota, United States.
DOI:10.25259/SNI_549_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Albert Alan1,2, Michelle Ennabe2,3, James Withers4, Neil Joshi5, Martin Weinand5. Addressing healthcare disparities in homeless neurosurgical patients: A comprehensive literature review on strategies for equitable care and improved outcomes. 16-Feb-2024;15:49
How to cite this URL: Albert Alan1,2, Michelle Ennabe2,3, James Withers4, Neil Joshi5, Martin Weinand5. Addressing healthcare disparities in homeless neurosurgical patients: A comprehensive literature review on strategies for equitable care and improved outcomes. 16-Feb-2024;15:49. Available from: https://surgicalneurologyint.com/surgicalint-articles/12753/
Abstract
Background: Homelessness is a growing concern in the US, with 3.5 million people experiencing it annually and 600,000 on any given night. Homeless individuals face increased vulnerability to 30-day hospital readmissions and higher mortality rates, straining the healthcare system and exacerbating existing disparities. This study aims to inform neurosurgeons on evidence-based strategies to reduce readmission and mortality rates among homeless patients by reviewing the literature on the impact of medical respite on 30-day readmission rates. The study aims to gauge the efficacy of medical respite in reducing hospital readmissions and improving health outcomes for homeless individuals.
Methods: A comprehensive literature search was conducted across PubMed, Embase/Medline, and Cochrane databases, as well as consulting the National Institute for Medical Respite Care and the Department of Health Care Access and Information. Ten articles were chosen from an initial 296 to investigate the impact of respite programs on readmission rates among homeless patients.
Results: Homeless patients experience high readmission rates due to various factors. Interventions such as respite programs and a comprehensive approach to healthcare can lower these rates. Collaboration between hospitals and medical respites has proven particularly effective.
Conclusion: Inadequate healthcare for homeless individuals leads to increased readmissions, longer hospital stays, and higher costs. Medical respites are a viable solution, but limited resources hamper their effectiveness. Therefore, it is crucial to facilitate cooperation between hospitals, respites, and other entities. Future research should focus on disparity in neurosurgical procedures and explore alternative services. An interdisciplinary approach is key to addressing healthcare inequalities.
Keywords: Healthcare disparities, Homelessness, Interdisciplinary collaboration, Medical respite, Neurosurgery
INTRODUCTION
The persistent challenge of unequal healthcare delivery affects numerous populations, with the homeless population being particularly susceptible to elevated rates of 30-day hospital readmissions and increased mortality.[
The higher risk of hospital readmission among homeless individuals across various treatment categories, including chronic respiratory disease and acute myocardial infarction (AMI), underscores the existence of healthcare disparities in this population.[
The present study draws on a comprehensive literature review examining the 30-day readmission rates of homeless patients to elucidate the existing disparities for neurosurgeons. Our findings reveal that homeless individuals experience higher 30-day readmission and mortality rates compared to their non-homeless counterparts. This study was motivated by the scarcity of extant literature addressing the provision of equitable care for homeless patients within the realm of neurosurgery. To the best of our knowledge, no prior research has specifically tackled this pressing issue. A thorough exploration of available sources highlights the prevailing inequities in healthcare for homeless individuals. Consequently, the primary objective of this study is to utilize the existing literature to inform neurosurgeons on the implementation of evidence-based strategies that ultimately aim to reduce readmission and mortality rates among the homeless patient population.
MATERIALS AND METHODS
We conducted a comprehensive and rigorous literature search encompassing PubMed, Embase/Medline, and Cochrane databases, to investigate the influence of medical respite on readmission rates among homeless patients. This search spanned from the inception of each database up to March 2023.
Our initial search strategy incorporated the following terms: “Homeless” “readmission” “rate,” “homelessness” “readmission” “rate,” and “homeless” or “homelessness” “readmission” “rate.” To expand the scope of our inquiry, we performed a secondary search using the terms “medical respite” and “readmission.” Finally, we conducted a tertiary search employing the terms “homeless patients” and “neurosurgery.” Articles were deemed relevant if they examined the impact of medical respite on homeless readmission rates.
To supplement our findings with the most recent data on medical respite and homeless hospitalization in California, we consulted both the National Institute for Medical Respite Care and the Department of Health Care Access and Information website. We also cited an article from outside the search criteria. Furthermore, we enriched our analysis by referencing an article that, while falling outside our initial search parameters, provided valuable insight.
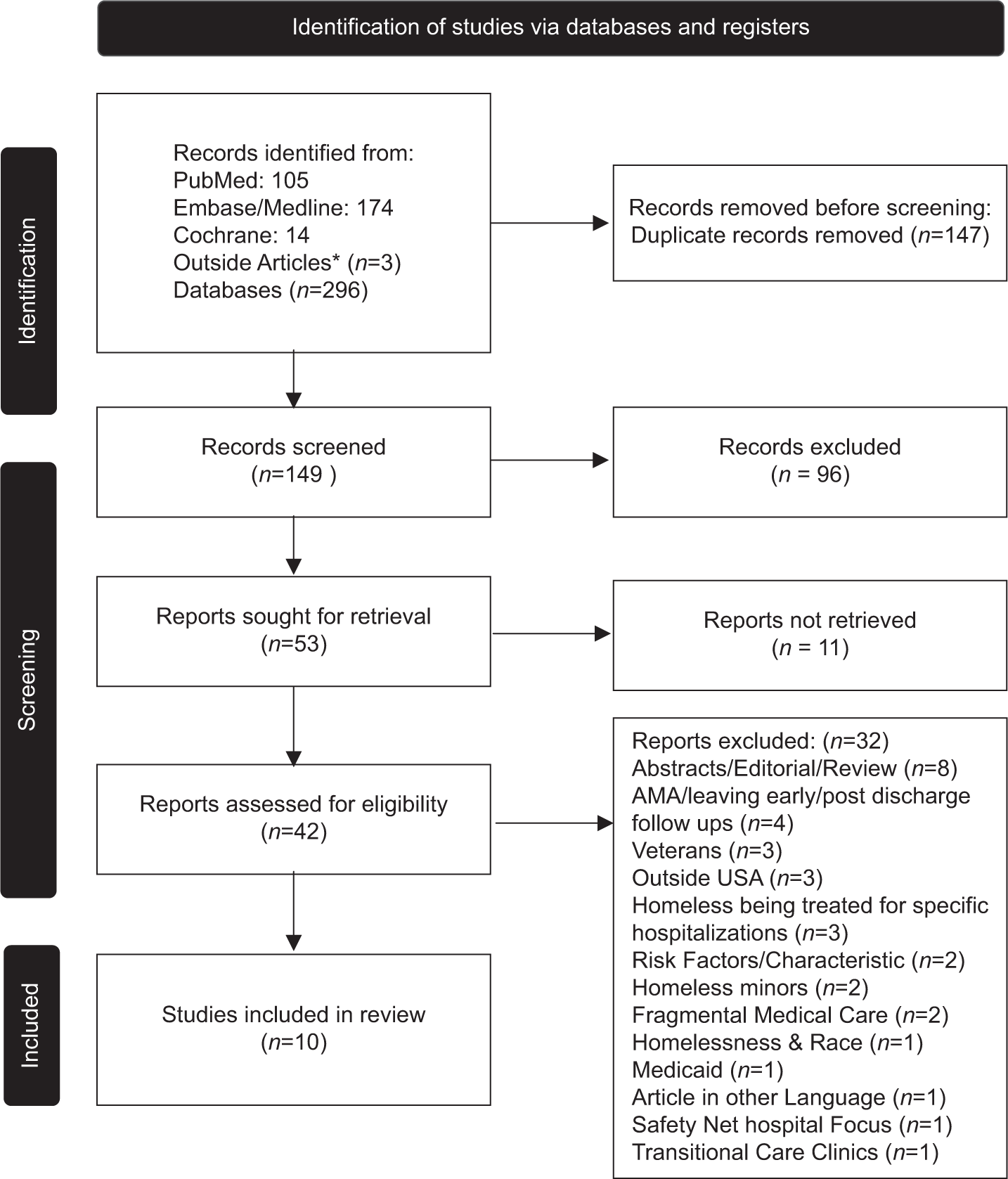
Our systematic search strategy, aligned with the PRISMA 2020 guidelines, is illustrated in
Figure 1:
Reducing homelessness recidivism: A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guided literature review on effective strategies. *Articles that were discovered beyond the established search parameters have been annotated with the appropriate citation designations. AMA: Against Medical Advice.
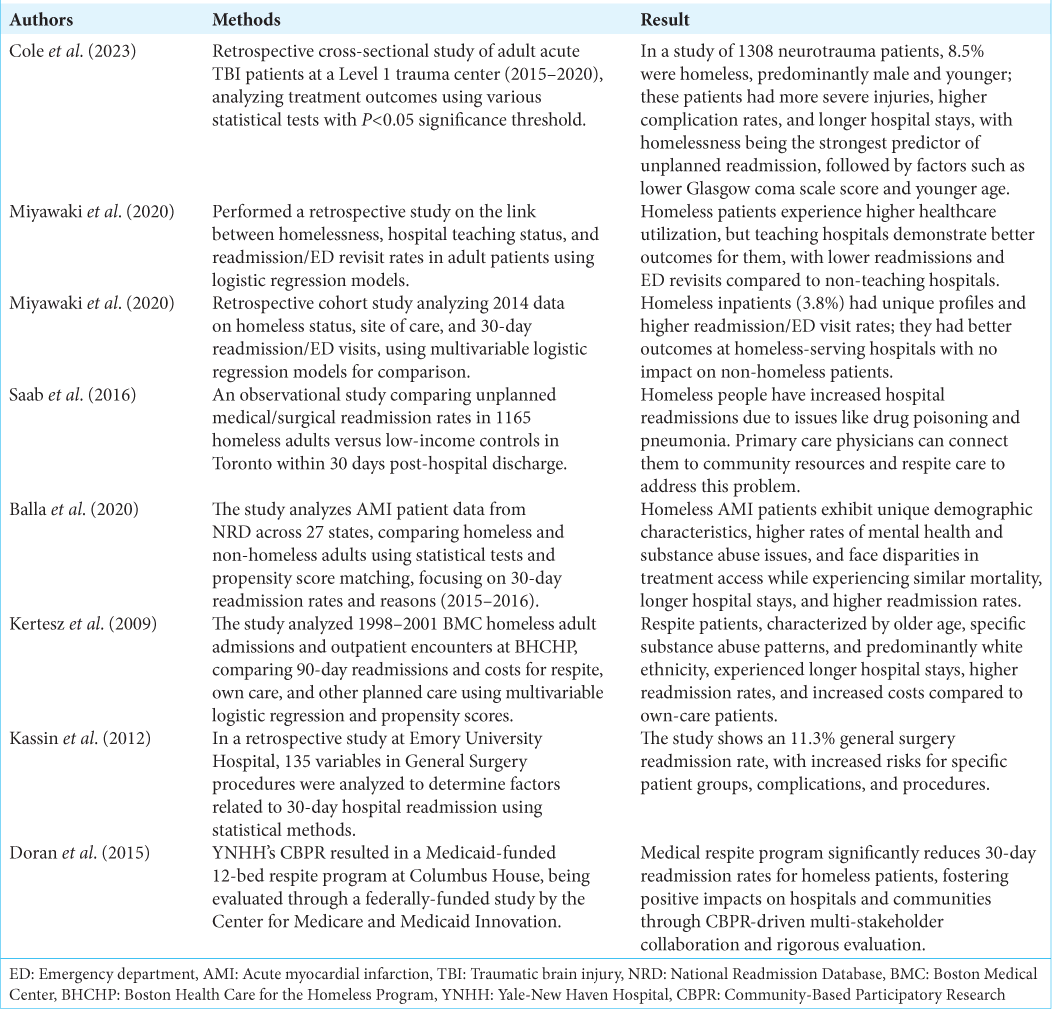
On meticulous evaluation of the remaining articles, 32 were deemed not relevant to the objectives of our systematic review and were subsequently excluded. Thus, our final analysis included ten articles, which constituted the foundation of our comprehensive review, with eight of these articles directly cited in
Overview of the articles
Of the eight distinct articles that are incorporated, four of these studies employed secondary data analysis, utilizing existing national or state databases such as the state inpatient database, the state emergency department (ED) database, the American Hospital Association Annual Survey, the American College of Surgeons National Surgical Quality Improvement Program database, and the National Readmission Database.
Three of the studies under examination were single-center investigations, focusing on data collected from individual hospitals. One of these investigations was particularly unique, as it targeted the homeless population residing in shelters in Toronto, Canada.
On close examination of the methodologies employed in the eight articles included in this review, it was observed that seven of the studies utilized retrospective research designs, whereas one study implemented a Community-Based Participatory Research Program. The rigorous nature of these research approaches lends credence to the findings and conclusions drawn from the body of literature reviewed.
RESULTS
In our review of the research, we found that the studies focused on four main areas related to hospitalization for the homeless, even though their methods were different. These areas included:
How homelessness contributes to higher 30-day hospital readmission rates Substance abuse and injuries: the dual dilemma exacerbating health struggles for the homeless Unveiling the impact on homeless patients’ health, hospital care, and recovery Optimizing healthcare interventions to minimize hospital readmissions among homeless populations.
This research has helped us understand the many factors that affect the healthcare experiences of homeless people, giving us a starting point for future studies and new approaches to address these important issues. Further, elaboration on these four issues are discussed down below.
How homelessness contributes to higher 30-day hospital readmission rates
Numerous articles have reported that individuals labeled as homeless experience higher hospital 30-day readmission rates.[
In addition, studies have shown that homeless patients have higher rates of 30-day readmissions and ED visits after hospital discharge compared to non-homeless patients.[
Teaching hospitals may be particularly adept at managing care for homeless individuals due to their investment in resources and care processes tailored to this population.[
Substance abuse and injuries: The dual dilemma exacerbating health struggles for the homeless
In the literature review search, we discovered that homeless patients had a heightened incidence of traumatic brain injuries on admission and frequently engaged in smoking, alcohol consumption, and illegal drug use.[
On examining risk factors for unexpected readmissions, homelessness emerged as the most influential predictor.[
Unveiling the impact on homeless patients’ health, hospital care, and recovery
Chronic morbidity, inadequate living conditions, and limited access to outpatient care contribute significantly to the high readmission rates among homeless patients.[
Adopting a comprehensive approach to patient care, which involves addressing both their acute conditions and overall well-being, could lead to more effective treatment outcomes.[
Optimizing healthcare interventions to minimize hospital readmissions among homeless populations
The study found that patients who received care at Boston’s respite program had a significantly lower likelihood of being readmitted to the hospital within 90 days compared to patients who received their care.[
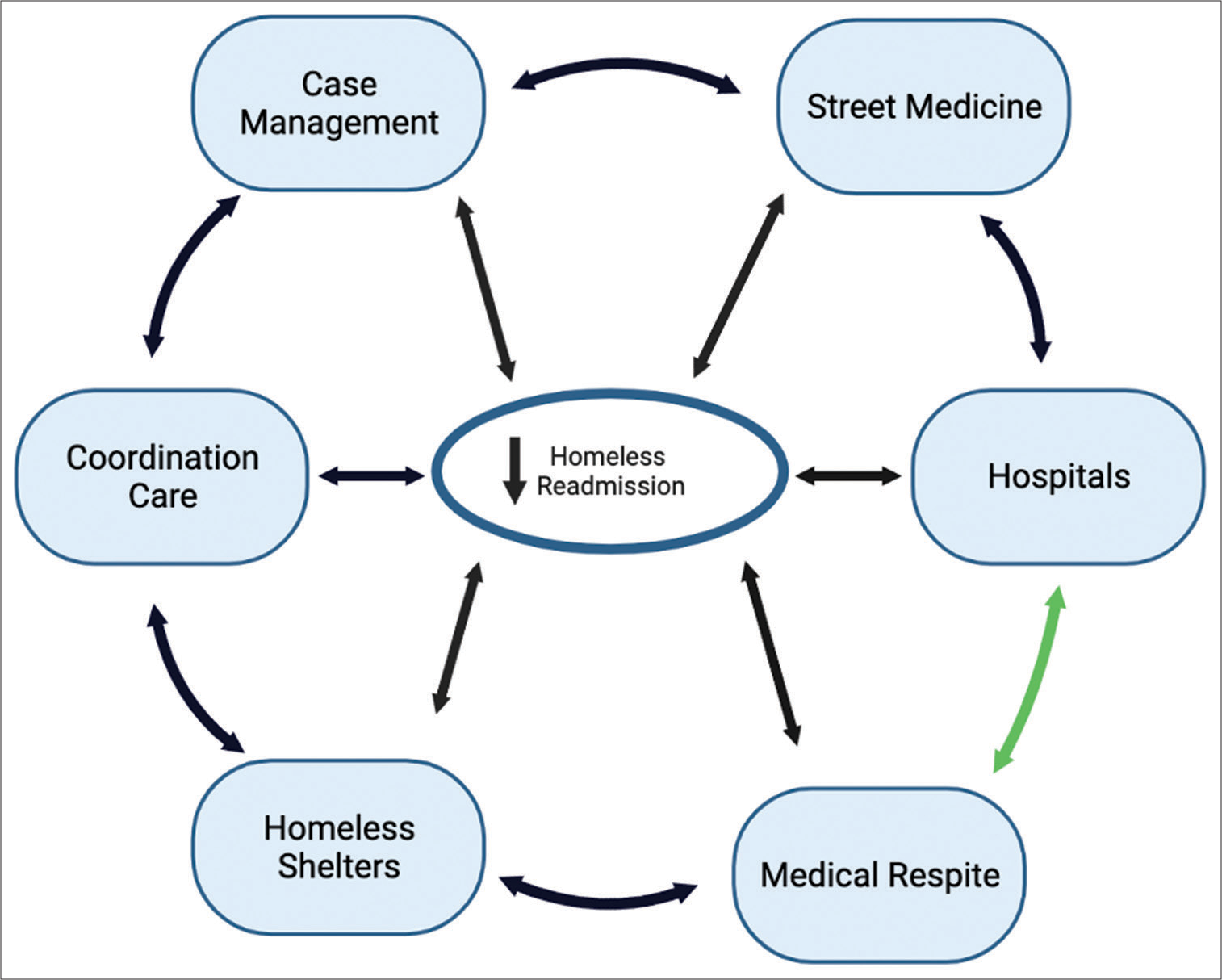
A comprehensive review of programs targeting the healthcare needs of the homeless has revealed a promising reduction in hospital readmission rates. To build on this progress, we advocate for an expanded collaborative care network, as visualized in
Figure 2:
Collaborative care network: Reducing readmissions. The flywheel model illustrates the impact of collaboration on outcomes and suggests that further reductions in homeless readmission may be attainable by incorporating additional resources such as street medicine teams, case managers, coordination of care, and homeless shelters.
The model underscores the potential benefits of these collaborations, signifying that further reductions may be possible by integrating resources from healthcare networks such as medical respites, hospitals, street medicine teams, case managers, care coordinators, and homeless shelters. The green arrow in the model connotes that while hospitals and medical respites individually contribute to decreased readmission rates, a collaborative approach might lead to a more significant decrease in readmissions.
Our proposal includes an innovative approach through the integration of an electronic medical record system and a live vacancy system for post-discharge recovery spots. This integration, facilitated by technology, is poised to enhance collaborative efforts. Once a robust system is in place, other elements of the flywheel model can be incorporated, thereby fostering an integrated care system for homeless patients.
The observed decrease in readmission rates following the implementation of this collaborative model highlights the significance of inter-organizational cooperation in mitigating health disparities and reducing readmission rates among the homeless population. Neurosurgeons can contribute considerably to these efforts by acquainting themselves with available resources and coordinating with case managers and care coordinators to ensure homeless patients receive necessary postoperative care.
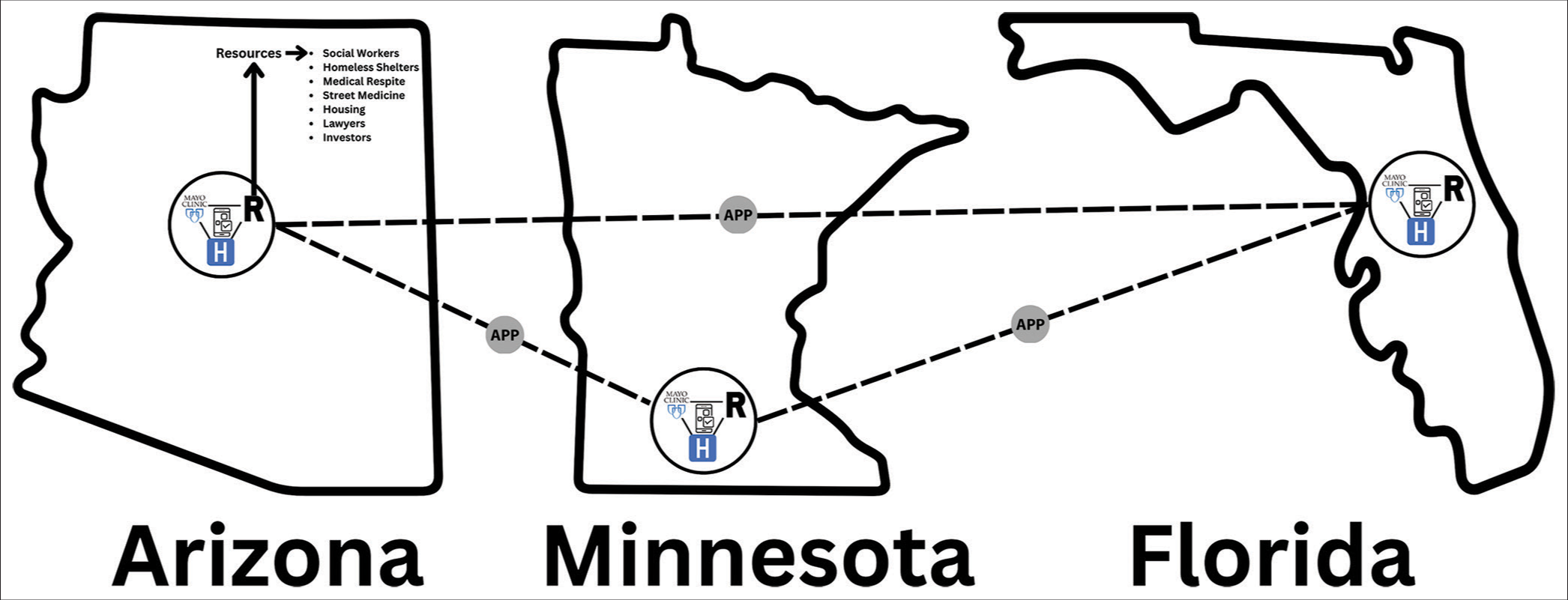
The integration of these resources through a software application, as illustrated in
Figure 3:
Ending Homelessness Task Force Integration Framework: This diagram illustrates a conceptual framework for the Ending Homelessness Task Force, highlighting the strategic integration of various resources through a software application to enhance the healthcare system for homeless individuals. The framework envisions a software program that notifies medical staff of available medical respites in proximity to hospitals. This connectivity is anticipated to facilitate a reduction in healthcare costs by streamlining access to appropriate care facilities for the homeless. Central to the framework is the Proposed Mayo Clinic Healthcare approach, which is designed to foster interdisciplinary collaboration among social workers, homeless shelters, medical respites, street medicine providers, housing authorities, lawyers, and investors. By bringing together these diverse resources, the framework aims to deliver comprehensive, quality healthcare to the homeless population and sets a precedent for standardizing care for marginalized groups. The schematic representation of the framework spans three states—Arizona, Minnesota, and Florida—indicating the scope and scalability of the initiative across different geographic regions. Within each state, hospitals identified with the Mayo Clinic symbol are connected to a centralized resource network, symbolized by the letter ‘R’. This network is accessible through an application, denoted by ‘APP’, serving as a digital gateway to the integrated resources. The proposed framework underscores the importance of technology and cross-sector collaboration in addressing the complex challenges associated with homelessness and healthcare provision. APP: Application, R: Resources, H: Hospitals.
DISCUSSION
A thorough analysis of existing research reveals that homeless patients often receive inadequate medical care, leading to higher 30-day readmission rates and significant disparities in inpatient mortality compared to non-homeless individuals.[
The results of previous research have highlighted a concerning trend: a substantial proportion of patients are readmitted to hospitals after undergoing surgical procedures, frequently due to underlying comorbidities.[
In light of these challenges, it is imperative to explore alternative solutions such as those presented by Saab et al. They suggest that targeted interventions could significantly mitigate these readmission rates, primarily through the integration of primary care physicians into the care continuum. These interventions could include connecting homeless individuals with existing community resources and facilitating their transition into respite care.[
In addition, in a pioneering endeavor, Doran et al. facilitated a collaborative relationship between Columbus House, a homeless shelter, and Yale New Haven Hospital. This partnership was driven to enhance healthcare services for homeless individuals, with a focus on optimizing the discharge process from the hospital. Data from this partnership yielded encouraging results.[
Bearing these findings in mind, we propose
To build on the groundwork laid by Doran et al.,[
By integrating with other hospitals and resources, the Mayo Clinic could establish a robust system to track homeless patients’ journeys through the healthcare system, even when admitted at nearby hospitals. With successful implementation in one city, this model could potentially be adapted and adopted by other Mayo Clinic locations and nearby hospitals, resulting in an organized communication network between hospitals, medical respite care, and available resources across different states. The realization of this model marks a significant stride in addressing the intricate healthcare needs of homeless individuals. It is anticipated to stimulate further research and innovative developments in this field, ultimately aiming to enhance health outcomes for this underserved population.
In this study, several limitations need to be highlighted and addressed in future research. First, research is scarce on the disparities in neurosurgical procedures and readmission rates between homeless and non-homeless individuals. Further investigation is necessary to determine if homeless patients who undergo neurosurgery have a higher likelihood of being readmitted to the hospital within 30 days and to identify the factors contributing to these differences. Second, while numerous studies indicate that homeless patients have elevated 30-day readmission rates, they often fail to elaborate on the underlying causes of this phenomenon. Future research should strive to uncover the reasons for this disparity and explore potential solutions to enhance healthcare outcomes for this vulnerable population. Finally, the current literature lacks sufficient examination of the benefits of alternative healthcare services, such as street medicine or coordinated care, in reducing readmission rates among homeless patients. Additional research is required to assess the effectiveness of these services in improving healthcare outcomes and lowering readmission rates for this demographic. By addressing these knowledge gaps, future studies can contribute to a better understanding of healthcare disparities and inform policy development aimed at optimizing care for homeless individuals.
Existing research shows that homeless patients often receive inadequate medical care, resulting in higher readmission rates, longer hospital stays, and increased care costs. Medical respites have been found to reduce post-discharge readmissions for homeless patients. However, limited resources, including a lack of medical respites and inadequate shelter options, make proper recovery difficult for this vulnerable population. Collaboration between hospitals, medical respites, and other resources can help reduce readmissions and improve healthcare outcomes for homeless individuals. Neurosurgeons can play a crucial role in this collaboration by working closely with case managers and care coordinators. Future research should focus on understanding disparities in neurosurgical procedures, identifying underlying causes of high readmission rates among homeless patients, and assessing the effectiveness of alternative healthcare services in improving healthcare outcomes for this population.
CONCLUSION
Individuals experiencing homelessness grapple with poor living conditions and a diminished quality of life, which negatively impacts their health and places a considerable strain on the healthcare system. Neurosurgeons can play a pivotal role in alleviating these issues by implementing interventions such as collaborative care models or establishing homeless task forces to reduce hospital readmissions and ensure adequate healing time for homeless patients upon discharge. An interdisciplinary approach, which involves collaboration among various sectors, is essential for providing optimal care to homeless individuals and addressing healthcare disparities within this population. This united effort has the potential to decrease homeless readmission rates significantly. Future research should delve deeper into the impact of neurosurgical care on homelessness, specifically examining readmission rates. If subsequent studies reveal equivalent readmission rates between homeless and non-homeless patients in neurosurgery, it could serve as a model for the broader healthcare system. By uniting different forces dedicated to supporting homeless populations, the healthcare system can demonstrate the feasibility of equitable care and underscore the importance of addressing disparities across other medical disciplines.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Balla S, Alqahtani F, Alhajji M, Alkhouli M. Cardiovascular Outcomes and rehospitalization rates in homeless patients admitted with acute myocardial infarction. Mayo Clin Proc. 2020. 95: 660-8
2. Cole KL, Findlay MC, Earl E, Sherrod BA, Cutler CB, Nguyen S. Understanding the unique challenges faced by homeless patients with acute traumatic neurosurgical injuries. Neurosurgery. 2023. 93: 292-9
3. Doran KM, Greysen SR, Cunningham A, Tynan-McKiernan K, Lucas GI, Rosenthal MS. Improving post-hospital care for people who are homeless: Community-based participatory research to community-based action. Healthc (Amst). 2015. 3: 238-44
4. Inpatient hospitalizations and emergency department visits for persons experiencing homelessness in California: Patient demographics by facility. Available from: https://hcai.ca.gov/visualizations/inpatient-hospitalizations-and-emergency-department-visits-for-persons-experiencing-homelessness-in-california-patient-demographics-by-facility [Last accessed on 2023 Mar 07].
5. Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012. 215: 322-30
6. Kertesz SG, Posner MA, O’Connell JJ, Swain S, Mullins AN, Shwartz M. Post-hospital medical respite care and hospital readmission of homeless persons. J Prev Interv Community. 2009. 37: 129-42
7. Medical respite care directory. National institute for medical respite care. Available from: https://nimrc.org/medical-respite-directory [Last accessed on 2023 Mar 07].
8. Miyawaki A, Burke LG, Khullar D, Tsugawa Y. Comparison of 30-day readmission and emergency department revisit rates among homeless patients at teaching versus non-teaching hospitals. Soc Sci Med. 2020. 263: 113283
9. Miyawaki A, Hasegawa K, Figueroa JF, Tsugawa Y. Hospital readmission and emergency department revisits of homeless patients treated at homeless-serving hospitals in the USA: Observational study. J Gen Intern Med. 2020. 35: 2560-8
10. Saab D, Nisenbaum R, Dhalla I, Hwang SW. Hospital readmissions in a community-based sample of homeless adults: A matched-cohort study. J Gen Intern Med. 2016. 31: 1011-8






Dr. Miguel A. Faria
Posted February 19, 2024, 8:40 am
Disparities in eveything, including health care, will always exist in free countries. And in communist countries like Cuba today and the former USSR, the equality is at the lowest common denominator with equal misery and disparity for everyone, except the nomenklatura and the tourists and useful idiots who come in with hard cash. The worst inequality and disparity today is probably communist China, where the communist cadre are the only ones with free healthcare and high tier medical care, but don’t worry they will tell you that communism has not been tried yet…