- School of Medicine, Universidad de los Andes, Bogota DC, Colombia
- Department of Diagnostic and Interventional Imaging, Hospital Universitario Fundacion Santa Fe de Bogota, Bogota DC, Colombia
- Department of Pathology, Hospital Universitario Fundacion Santa Fe de Bogota, Bogota DC, Colombia
Correspondence Address:
Juan N. Useche
Department of Diagnostic and Interventional Imaging, Hospital Universitario Fundacion Santa Fe de Bogota, Bogota DC, Colombia
DOI:10.4103/sni.sni_123_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nicolas Yanez, Luisa K. Cifuentes, Marcela Mejia, Juan N. Useche. Advantages of using a detachable-tip microcatheter and liquid embolic agents in the preoperative embolization of a recurrent cerebellar hemangioblastoma: A case report. 26-Sep-2017;8:239
How to cite this URL: Nicolas Yanez, Luisa K. Cifuentes, Marcela Mejia, Juan N. Useche. Advantages of using a detachable-tip microcatheter and liquid embolic agents in the preoperative embolization of a recurrent cerebellar hemangioblastoma: A case report. 26-Sep-2017;8:239. Available from: http://surgicalneurologyint.com/surgicalint-articles/advantages-of-using-a-detachable%e2%80%91tip-microcatheter-and-liquid-embolic-agents-in-the-preoperative-embolization-of-a-recurrent-cerebellar-hemangioblastoma-a-case-report/
Abstract
Background:The preferred treatment for intracranial hemangioblastomas is surgical resection with or without preoperative embolization, however, embolization remains controversial due to risks such as distal tip entrapment, vascular injury during navigation, and embolic agent migration.
Case Description:A 54-year-old woman was admitted for surgical resection and preoperative embolization of a cerebellar hemangioblastoma. Although experience using Onyx with detachable and nondetachable tip microcatheters has been well reported in a variety of clinical circumstances, we describe the first case of a presurgical embolization of an intra-axial tumor using a second-generation detachable-tip microcatheter and a nonadhesive liquid embolic agent. Following the procedure, a nearly complete angiographic obliteration was achieved, as well as a successful subsequent surgical resection.
Conclusion:Preoperative embolization with detachable-tip microcatheters and liquid embolic agents should be taken into consideration when assessing patients with hemangioblastomas of the posterior fossa due to the reduced risks of cardiac arrest, hemorrhage, and death.
Keywords: Catheterization, hemangioblastoma, intracranial hemorrhage, therapeutic embolization
INTRODUCTION
Hemangioblastomas are World Health Organization (WHO) grade I, highly vascularized mesenchymal tumors that represent approximately 2% of intracranial tumors and 10% of posterior fossa tumors.[
CASE HISTORY
Case presentation
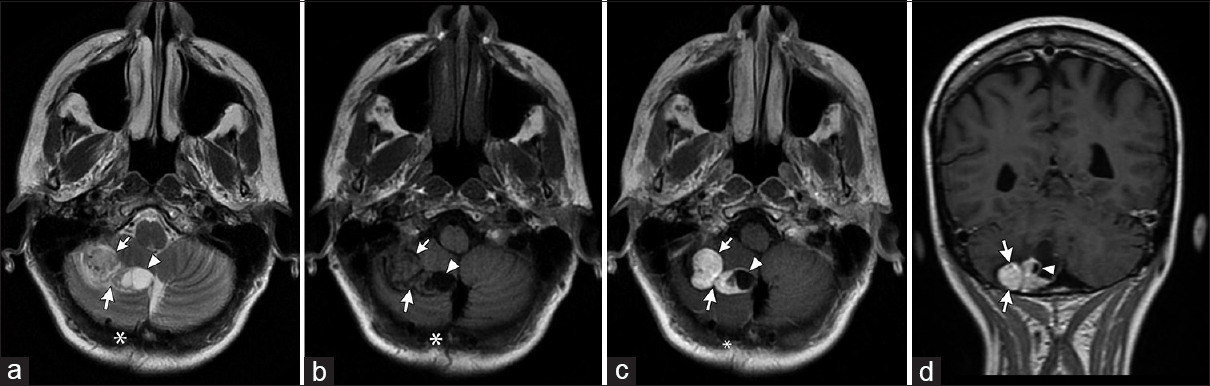
A 54-year-old woman with a history of a right cerebellar hemangioblastoma, who was surgically treated in 2005, presented 11 years later with a 2-week history of postural instability, vertigo, and left suboccipital headache. Brain magnetic resonance imaging (MRI) upon admittance revealed two brightly enhancing nodules with a medial cyst in the inferior surface of the right cerebellar hemisphere, which was consistent with recurrent disease [
Figure 1
Preoperative brain MRI sequences. (a) T2-weighted axial; (b) T1-weighted axial without contrast; (c) T1-weighted axial with contrast; (d) T1-weighted coronal with contrast. Images show a bilobular well-defined homogeneous solid mass (arrows) with a medial cystic component (arrowheads) involving the inferior and medial aspects of the right cerebellar hemisphere, consistent with recurrent disease. Adjacent postsurgical changes (asterisks) are also observed
Treatment
Using a Phillips Allura Xper FD 20 interventional X-ray system, a right transfemoral access was obtained, a 6-French introducer vascular sheath was placed and 4000 IU of unfractionated heparin (UFH) were administered.
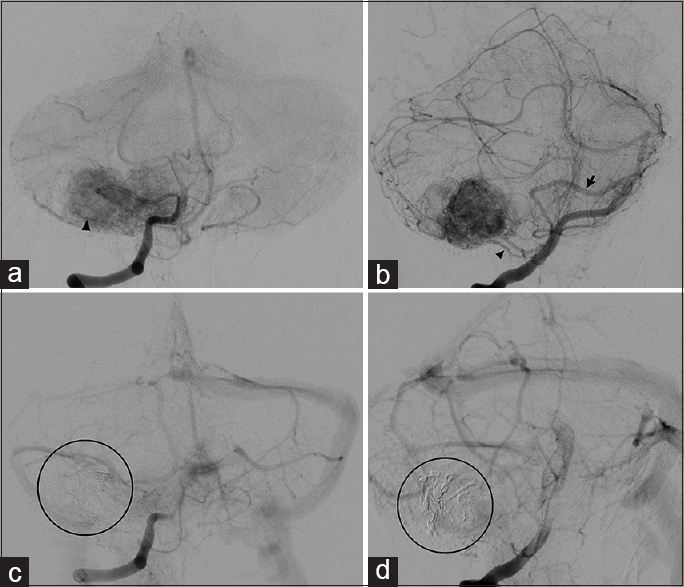
A right vertebral diagnostic angiography showed a right AICA–PICA complex as the main feeder of the tumor [
Figure 2
Diagnostic and postembolization angiograms. (a and b) AP and lateral views show a bilobular hypervascular mass with delineation of the cystic medial hypovascular component. The lateral main branch (arrowhead) of the right AICA-PICA complex (arrow) supplies the mass, as described in the text. (c and d) AP and lateral views show evidence of obliteration of approximately 70% of the lesion with a minimal residual filling of its medial component. The Onyx cast is visualized (circle)
Then, a Neuron 6F 070 guiding catheter (Penumbra Inc., Alameda, CA, USA) was placed in the second segment of the right vertebral artery (V2). An Apollo™ microcatheter with a 15 mm detachable-tip (Medtronic, Minneapolis, MN, USA) was navigated over a Mirage™ 0.008 hydrophilic guidewire (Micro Therapeutics Inc., Irvine, CA, USA) allowing the superselective catheterization of the lateral branch of the AICA–PICA complex. Adequate position of the microcatheter was confirmed, without evidence of opacification of normal parenchymal vessels.
The microcatheter was flushed with 5 mL of normal saline and 0.3 mL of dimethyl sulfoxide (DMSO), and, under fluoroscopic visualization, 0.8 mL of Onyx-18® (Medtronic, Minneapolis, MN, USA) were administered to embolize the main lateral branch, achieving an obliteration of 70% of the tumor vascular blush. Then, under road map guidance and permanent fluoroscopic visualization, controlled traction of the microcatheter was exerted in two periods, allowing for a brief interval of tension release between each period, until the 15 mm-tip was successfully detached without complications. The microcatheter extraction was performed carefully and slowly to prevent heart rates below 45 beats per minute.
Subsequent angiographic runs did not reveal any unexpected vascular occlusions or dissections. After the vascular sheath removal, there was no evidence of inguinal hematoma or peripheral pulse abnormalities.
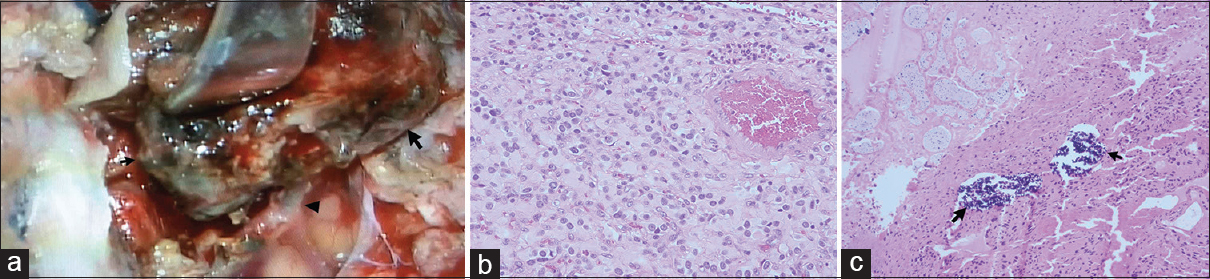
The patient underwent a successful complete surgical resection the following day. Pathology demonstrated a recurrent hemangioblastoma with embolization-induced ischemic changes [
Figure 3
Intraoperative findings and microphotographs of hematoxylin-eosin-stained slides of the specimen. (a) The devascularized tumor (arrows) is held by a spatula, exposing a vessel containing embolization material (arrowheads). Normal cerebellar parenchyma can be observed on the inferior left corner of the picture. (b) The abundance of monomorphic stromal cells with pale and vacuolated cytoplasm is consistent with a recurrent hemangioblastoma (40×). (c) Onyx (arrows) can be observed within a vascular lumen, along with surrounding ischemic-induced pathological changes (10×)
Outcome and follow-up
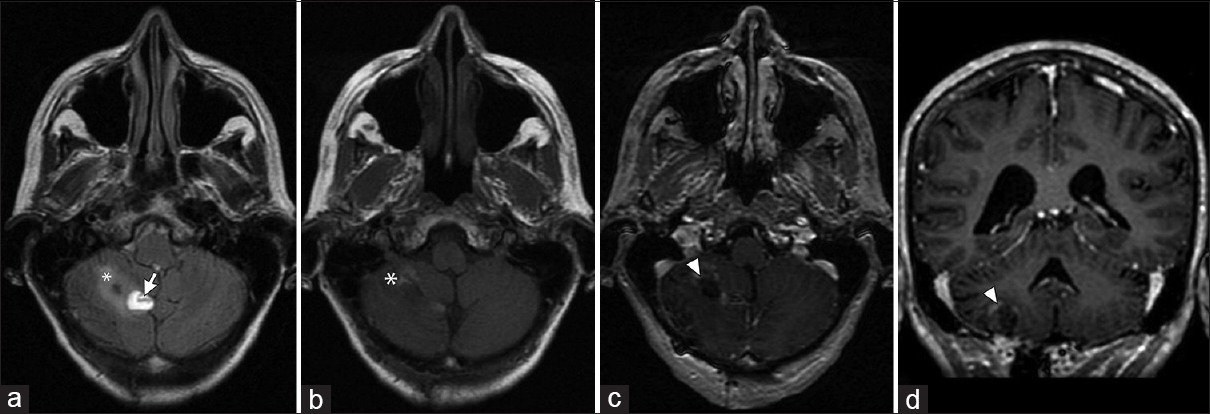
During the follow-up, the patient remained symptom-free for more than a year without MRI findings of recurrent disease [
Figure 4
Postoperative brain MRI sequences (13 days later). (a) T2-weighted FLAIR axial; (b) T1-weighted axial without contrast; (c) T1-weighted axial with contrast; (d) T1-weighted coronal with contrast. Images show a small hematoma (arrow) in the medial aspect of the surgical cavity, mild residual edema (asterisk) and minimal linear postsurgical enhancement (arrowhead) without evidence of a residual lesion
DISCUSSION
Complete resection of cerebellar hemangioblastomas can be difficult owing to the location, mass effect, and tumor vascularity. Intractable intraoperative hemorrhage with high rates of morbidity and mortality has been reported.[
Endovascular embolization can be performed with coils, particles, or liquid embolic agents. Coils can occlude large feeders and provide a more controllable embolization, however, they lack the ability to reach deep into the tumor vascular bed. Particles such as Gelfoam, polyvinyl alcohol (PVA), and Embospheres provide the advantage of better tumor vessel occlusion; however, they carry a high risk of inadvertent nontarget embolization, permanent neurologic deterioration as reported by Montano et al.,[
Alternatively, detachable-tip microcatheters have been used for arteriovenous malformation (AVM) embolization. The Apollo microcatheter is a second-generation single-lumen end-hole catheter with a 15-mm, 30-mm, or 50-mm detachable-tip. These microcatheters are NBCA and Onyx compatible and have the advantage of allowing longer injection times than conventional microcatheters, which is particularly useful when using NBCA. A true circumferential occlusion can be achieved with Onyx, permitting the filling of a larger amount of angioarchitecture. However, its most important advantage is a better and less traumatic catheter withdrawal, which decreases the risk of retention and artery rupture.
Since the first report of the use of detachable-tip microcatheters in 2008 by Ozturk et al.,[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abo-Al Hassan A, Ismail M, Panda SM. Pre-operative endovascular embolization of a cerebellar haemangioblastoma. A case report. Med Princ Pract. 2006. 15: 459-62
2. Cornelius JF, Saint-Maurice JP, Bresson D, George B, Houdart E. Hemorrhage after particle embolization of hemangioblastomas: Comparison of outcomes in spinal and cerebellar lesions. J Neurosurg. 2007. 106: 994-8
3. Dabus G, Pryor J, Spilberg G, Samaniego EA, Nogueira RG. Embolization of intra-axial hypervascular tumors with Onyx: Report of three cases. J Neurointerv Surg. 2013. 5: 177-80
4. Ding D, Starke RM, Evans AJ, Liu KC. Direct transcranial puncture for Onyx embolization of a cerebellar hemangioblastoma. J Clin Neurosci. 2014. 21: 1040-3
5. Eskridge JM, McAuliffe W, Harris B, Kim DK, Scott J, Winn HR. Preoperative endovascular embolization of craniospinal hemangioblastomas. AJNR Am J Neuroradiol. 1996. 17: 525-31
6. Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D. The CARE Guidelines: Consensus-based Clinical Case Reporting Guideline Development. Glob Adv Health Med. 2013. 2: 38-43
7. Liu AH, Peng TM, Wu Z, Xiao XR, Jiang CH, Wu ZX. Clinical effectiveness of preoperative embolization for cerebellar hemangioblastoma. Asian Pac J Cancer Prev. 2013. 14: 5179-83
8. Montano N, Doglietto F, Pedicelli A, Albanese A, Lauretti L, Pallini R. Embolization of hemangioblastomas. J Neurosurg. 2008. 108: 1063-
9. Ozturk MH, Unal H, Dinc H. Embolization of an AVM with acrylic glue through a new microcatheter with detachable tip: An amazing experience. Neuroradiology. 2008. 50: 903-4
10. Sakamoto N, Ishikawa E, Nakai Y, Akutsu H, Yamamoto T, Nakai K. Preoperative endovascular embolization for hemangioblastoma in the posterior fossa. Neurol Med Chir (Tokyo). 2012. 52: 878-84
11. Seong Eom K, Won Kim D, Sung Choi S, Ha Choi K, Young Kim T. Preoperative embolization of a cerebellar haemangioblastoma using Onyx: Case report and literature review. Neurol Neurochir Pol. 2011. 45: 292-6
12. Shin GW, Jeong HW, Seo JH, Kim ST, Choo HJ, Lee SJ. Preoperative embolization of cerebellar hemangioblastoma with onyx: Report of three cases. Neurointervention. 2014. 9: 45-9