- Department of Emergency Medicine, HonorHealth Osborn, Scottsdale, United States
- Department of Surgery, Division of Trauma, Valleywise Health Medical Center, Phoenix, United States
- Department of Trauma Surgery and Surgical Critical Care, HonorHealth Osborn, Phoenix, United States
- Department of Surgery, Division of Plastic Surgery, Valleywise Health Medical Center, Phoenix, United States
- Department of Surgery, Division of Neurosurgery, Valleywise Health Medical Center, Phoenix, United States.
Correspondence Address:
Iman Feiz-Erfan, Division of Neurosurgery, Valleywise Health Medical Center, Phoenix, United States.
DOI:10.25259/SNI_386_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Adrienne R. Azurdia1, Jarvis Walters2, Chris R. Mellon3, Salvatore C. Lettieri4, Tammy R. Kopelman2, Paola Pieri2, Iman Feiz-Erfan5. Airway risk associated with patients in halo fixation. 29-Mar-2024;15:104
How to cite this URL: Adrienne R. Azurdia1, Jarvis Walters2, Chris R. Mellon3, Salvatore C. Lettieri4, Tammy R. Kopelman2, Paola Pieri2, Iman Feiz-Erfan5. Airway risk associated with patients in halo fixation. 29-Mar-2024;15:104. Available from: https://surgicalneurologyint.com/surgicalint-articles/12835/
Abstract
Background: The halo fixation device introduces a significant obstacle for clinicians attempting to secure a definitive airway in trauma patients with cervical spine injuries. The authors sought to determine the airway-related mortality rate of adult trauma patients in halo fixation requiring endotracheal intubation.
Methods: This study was a retrospective chart review of patients identified between 2007 and 2012. Only adult trauma patients who were intubated while in halo fixation were included in the study.
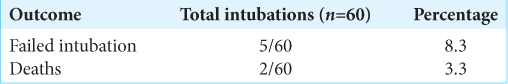
Results: A total of 46 patients underwent 60 intubations while in halo. On five occasions, (8.3%) patients were unable to be intubated and required an emergent surgical airway. Two (4.4%) of the patients out of our study population died specifically due to airway complications. Elective intubations had a failure rate of 5.8% but had no related permanent morbidity or mortality. In contrast to that, 25% of non-elective intubations failed and resulted in the deaths of two patients. The association between mortality and non-elective intubations was statistically highly significant (P = 0.0003).
Conclusion: The failed intubation and airway-related mortality rates of patients in halo fixation were substantial in this study. This finding suggests that the halo device itself may present a major obstacle in airway management. Therefore, heightened vigilance is appropriate for intubations of patients in halo fixation.
Keywords: Halo Fixation, Airway Management, Tracheostomy, Loss of Airway Mortality, Cervical Injury, Trauma Intubation, Emergent Intubation
INTRODUCTION
The halo fixation device introduced by Nickel et al. in 1959 initially provided a novel approach to cervical spine stabilization in patients suffering from poliomyelitis, and shortly after that, it was also used to treat traumatic cervical spine injuries.[
Endotracheal intubation in patients with traumatic cervical spine injuries is particularly challenging due to simultaneous inline stabilization, which prohibits the neck extension necessary to obtain an optimal tracheal view.[
The purpose of this study was to determine the airway-related morbidity and mortality rate of adult trauma patients in halo fixation undergoing emergent and non-emergent endotracheal intubation.
MATERIALS AND METHODS
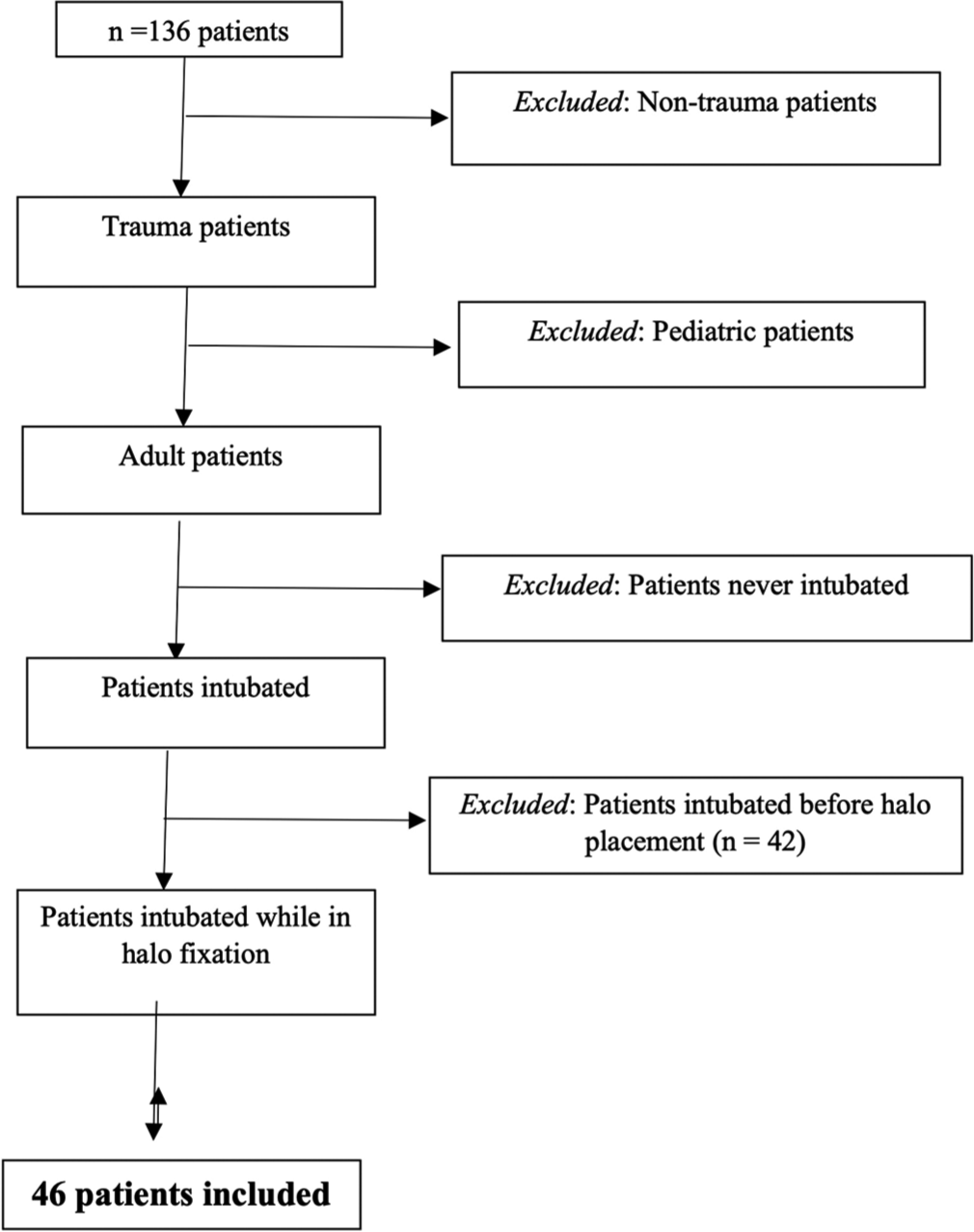
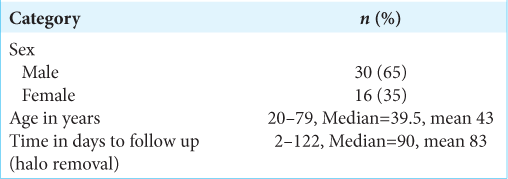
This study was a retrospective chart review at a single, urban, level 1 trauma center between 2007 and 2012. One hundred and thirty-six consecutive patients that required halo fixation provided by the senior author (IFE) were identified. All patients were placed in the same model of halo (Össur Americas, Foothill Ranch, CA; Hanger Orthotics, Tempe, AZ). Patients under the age of 18 years and those with atraumatic spinal pathology were excluded from the study. In addition, haloed patients who never required intubation while in halo were excluded from the study. Emergent intubation was deemed an unanticipated need for definitive airway control, while non-emergent intubations, such as intra-operative intubation, were planned. To specifically examine the mechanical challenges associated with intubating a haloed patient, only those who were intubated while in halo fixation were included in the study. Time to follow-up was defined as the number of days until removal of halo, death, or till lost to follow-up before halo removal. Failed intubation was defined as the immediate and unexpected need for a surgically established airway at the time of intubation and/or death or anoxic brain damage resulting from hypoxia immediately associated with complicated intubation. Failed intubation and overall mortality rates were calculated based on the final number of patients and number of intubations while in halo.
The Chi-square test for comparison of two proportions from independent samples was applied. P = 0.05 or less was considered statistically significant. P < 0.001 was considered statistically highly significant [
RESULTS
Based on our methods, the study population comprised 46 patients [
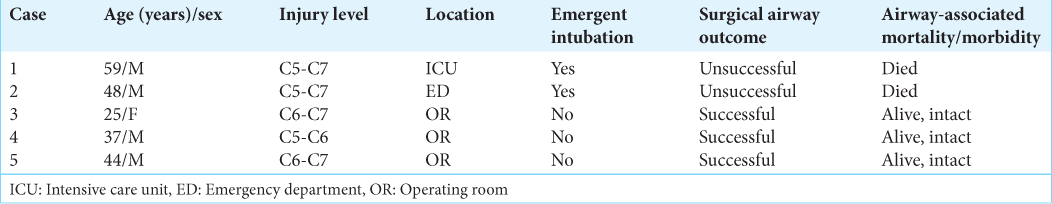
In contrast, eight intubations had to be done urgently or emergently. These were done mainly in the intensive care unit (ICU) in six instances. In one instance, non-elective intubation was done in the emergency department (ED) or OR. These intubations also applied the above mentioned techniques but on a non-elective basis. In these instances, personnel of the ED or ICU joined along with the anesthesia team to provide intubations. Under these circumstances, two intubations failed and required the placement of a definitive surgical airway. However, in both instances, the patient ultimately died secondary to hypoxia from the failure of timely establishment of functional airway and ventilation. Therefore, the mortality rate associated with non-elective intubations was 25%. Although there was a trend between airway failure and non-elective intubations, it did not reach statistical significance (P = 0.07). However, the mortality associated with failed non-elective intubation was statistically highly significant (P = 0.0003).
Calculated based on the number of intubations (n = 60), the airway failure rate was 8.3%, with an associated mortality rate of 3.3% [
Analyzing based on the study population (n = 46), five patients (10.9%) required an emergent surgical airway, of which two (4.4%) died specifically due to the inability to establish an airway sufficiently [
The presence of spinal cord injury (SCI) was noted in one patient out of five with failed intubations (20%) and in 6 patients (14.1%) out of 41 patients with successful intubations. Alternatively, 1 (14.3%) of seven patients with SCI suffered airway failure and death while being intubated in the halo. This contrasts with four patients (10.3%) out of 39 without SCI who suffered from airway failure while intubated in the halo. Of these, one patient (2.6%) died from this complication.
DISCUSSION
Intubating trauma patients with potential cervical spine injuries is challenging, but obtaining a definitive airway in haloed patients is an even more formidable task. In a recent study by Lockey et al. involving more than 7000 trauma patients, investigators found that only 0.7% of intubations failed.[
A variety of factors may have contributed to the poor outcomes in these patients, though some may have been more influential than others. The haloes prohibited the extension of the patient’s cervical spines, which notoriously made airway visualization more difficult.[
Another contributing factor to airway complications in this population may be the presence of a concomitant SCI. Cervical SCI can paralyze a patient’s diaphragm and thoracic musculature, leading to decreased pulmonary vital capacity. This subsequently puts patients at risk for rapid decompensation during airway management.[
Airway management can also be affected by the setting in which it takes place, such as in emergent or non-emergent settings. Patients requiring emergent intubation are frequently managed with minimal information available to the clinician and are more likely to be hemodynamically unstable or hypoxic before the procedure.[
Finally, the bulky halo itself may be a primary contributing factor complicating airway management in these patients. The fundamental structure of the orthosis obstructs the already limited workspace of the intubating physician. In fact, although the halo used with our patients is thought to be one of the most streamlined devices available, multiple metal struts still protrude anterolaterally and encompass the airway. This physical barrier, in conjunction with the obstacles, may have been a significant contributor to the markedly greater rate of unsuccessful intubations and deaths of our haloed patients.
There were limitations to our study. First, our sample size was limited due to the single site and author’s experience reviewed in this study. This may have produced a seemingly greater proportion of poor outcomes than would have been seen with a larger number of patients. Not all patients could be followed till the removal of the halo. Without knowing their complete outcomes and the possibility of intubations while in halo occurring at outside facilities, the findings of this study do not represent the true complication rates. Finally, we did not explore the different techniques used to intubate as well as the sequence in which such techniques were applied during intubation, which may have influenced the patient’s outcome in conjunction with the halo itself. The method used would be of particular interest given that most complications and deaths occurred during non-elective intubations and that advanced techniques such as planned fiberoptic intubation have been repeatedly shown to provide greater success in intubations that are expected to be difficult.[
CONCLUSION
With an immobile spine, limited respiratory reserve from SCI, and emergent airways, patients in halo fixation represent a culmination of individual factors that can make endotracheal intubation extremely challenging. The halo itself also appears to be an obstacle, contributing to the markedly increased failed intubation and mortality rates seen in this population. Considering early tracheostomy placement, as well as intubating before halo placement, may all prove to be strategies which could help to reduce the frequency of airway failure, its related morbidity, and mortality associated with intubations of patients in halo fixation.
Ethical approval
Institutional Review Board (IRB) permission obtained for the study, No: IRB # 2013-42 and approval date 3/8/2013.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aprahamian C, Thompson BM, Finger WA, Darinz JC. Experimental cervical spine injury model: Evaluation of airway management and splinting techniques. Ann Emerg Med. 1984. 13: 584-7
2. Austin N, Krishnamoorthy V, Dagal A. Airway management in cervical spine injury. Int J Crit Illn Inj Sci. 2014. 4: 50
3. Avitsian R, Lin J, Lotto M, Ebrahim Z. Dexmedetomidine and awake fiberoptic intubation for possible cervical spine myelopathy: A clinical series. J Neurosurg Anesthesiol. 2005. 17: 97-9
4. Bannister F, Macbeth R. Direct laryngoscopy and tracheal intubation. Lancet. 1944. 2: 651-4
5. Bellamy R, Pitt FW, Stauffer ES. Respiratory complications in traumatic quadriplegia: Analysis of 20 years’ experience. J Neurosurg. 1973. 39: 596-600
6. Bergofsky EH. Mechanism for respiratory insufficiency after cervical cord injury: A source of alveolar hypoventilation. Ann Intern Med. 1964. 61: 435-47
7. Bransford RJ, Stevens DW, Uyeji S, Bellabarba C, Chapman JR. Halo vest treatment of cervical spine injuries: A success and survivorship analysis. Spine (Phila Pa 1976). 2009. 34: 1561-6
8. Chan RC, Schweigel JF, Thompson GB. Halo-thoracic brace immobilization in 188 patients with acute cervical spine injuries. J Neurosurg. 1983. 58: 508-15
9. Cohn AI, Lau M, Leonard J. Emergent airway management at a remote hospital location in a patient wearing a halo traction device. Anesthesiology. 1998. 89: 545-6
10. Cooper PR, Maravilla KR, Sklar FH, Moody SF, Clark WK. Halo immobilization of cervical spine fractures: Indications and results. J Neurosurg. 1979. 50: 603-10
11. Crosby ET. Airway management in adults after cervical spine trauma. Anesthesiology. 2006. 104: 1293-318
12. Crosby ET. Considerations for airway management for cervical spine surgery in adults. Anesthesiol Clin. 2007. 25: 511-33
13. Garfin SR, Botte MJ, Waters RL, Nickel VL. Complications in the use of the halo fixation device. J Bone Joint Surg Am. 1986. 68: 320-5
14. Glaser JA, Whitehill R, Stamp WG, Jane JA. Complications associated with the halo-vest: A review of 245 cases. J Neurosurg. 1986. 65: 762-9
15. Horn EM, Theodore N, Feiz-Erfan I, Lekovic GP, Dickman CA, Sonntag VK. Complications of halo fixation in the elderly. J Neurosurg. 2006. 5: 46-9
16. Jaber S, Amraoui J, Lefrant JY, Arich C, Cohendy R, Landreau L. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: A prospective, multiple-center study. Crit Care Med. 2006. 34: 2355-61
17. James J. Fracture dislocation of cervical spine. J R Coll Surg Edinb. 1960. 5: 232-3
18. Koch RA, Nickel VL. The halo vest: An evaluation of motion and forces across the neck. Spine (Phila Pa 1976). 1978. 3: 103-7
19. Kostuik JP. Indications for the use of the halo immobilization. Clin Orthop Relat Res. 1981. 154: 46-50
20. Langeron O, Birenbaum A, Amour J. Airway management in trauma. Minerva Anestesiol. 2009. 75: 307-11
21. Lind B, Bake B, Lundqvist C, Nordwall A. Influence of halo vest treatment on vital capacity. Spine (Phila Pa 1976). 1987. 12: 449-52
22. Lockey D, Crewdson K, Weaver A, Davies G. Observational study of the success rates of intubation and failed intubation airway rescue techniques in 7256 attempted intubations of trauma patients by pre-hospital physicians. Br J Anaesth. 2014. 113: 220-5
23. Lyddon DW. Experience with the halo and body cast in the ambulatory treatment of cervical spine fractures. IMJ Ill Med J. 1974. 146: 458-61
24. Majernick TG, Bieniek R, Houston JB, Hughes HG. Cervical spine movement during orotracheal intubation. Ann Emerg Med. 1986. 15: 417-20
25. Martin LD, Mhyre JM, Shanks AM, Tremper KK, Kheterpal S. 3,423 Emergency tracheal intubations at a university hospital airway outcomes and complications. Anesthesiology. 2011. 114: 42-8
26. Mashour GA, Stallmer ML, Kheterpal S, Shanks A. Predictors of difficult intubation in patients with cervical spine limitations. J Neurosurg Anesthesiol. 2008. 20: 110-5
27. Mather JS. Impossible direct laryngoscopy in achondroplasia. A case report. Anaesthesia. 1966. 21: 244-8
28. Mercer M. Respiratory failure after tracheal extubation in a patient with halo frame cervical spine immobilization--rescue therapy using the Combitube airway. Br J Anaesth. 2001. 86: 886-91
29. Mohan R, Rajiv I, Thaller S. Airway management in patients with facial trauma. J Craniofac Surg. 2009. 20: 21-3
30. Mort TC. Complications of emergency tracheal intubation: Immediate airway-related consequences: Part II. J Intensive Care Med. 2007. 22: 208-15
31. Nickel V, Perry J, Garrett A, Snelson R. Application of the halo. Orthop Prosthet Appliance J. 1960. 14: 31-5
32. Nickel VL, Perry J, Garrett A, Heppenstall M. The halo. A spinal skeletal traction fixation device. J Bone Joint Surg. 1968. 50: 1400-9
33. Perry J. The halo in spinal abnormalities: Practical factors and avoidance of complications. Orthop Clin North Am. 1972. 3: 69-80
34. Perry M, Morris C. Advanced trauma life support (ATLS) and facial trauma: Can one size fit all? Part 2: ATLS, maxillofacial injuries and airway management dilemmas. Int J Oral Maxillofac Surg. 2008. 37: 309-20
35. Prolo DJ, Runnels JB, Jameson RM. The injured cervical spine: Immediate and long-term immobilization with the halo. JAMA. 1973. 224: 591-4
36. Rose DK, Cohen MM. The airway: Problems and predictions in 18,500 patients. Can J Anaesth. 1994. 41: 372-83
37. Sakles JC, Laurin EG, Rantapaa AA, Panacek EA. Airway management in the emergency department: A one-year study of 610 tracheal intubations. Ann Emerg Med. 1998. 31: 325-32
38. Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults: A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995. 82: 367-76
39. Sharpe JP, Magnotti LJ, Weinberg JA, Schroeppel TJ, Fabian TC, Croce MA. The old man and the C-spine fracture: Impact of halo vest stabilization in patients with blunt cervical spine fractures. J Trauma Acute Care Surg. 2016. 80: 76-80
40. Sims CA, Berger DL. Airway risk in hospitalized trauma patients with cervical injuries requiring halo fixation. Ann Surg. 2002. 235: 280-4
41. Sloane C, Vilke GM, Chan TC, Hayden SR, Hoyt DB, Rosen P. Rapid sequence intubation in the field versus hospital in trauma patients. J Emerg Med. 2000. 19: 259-64
42. Stone DJ, Keltz H. The effect of respiratory muscle dysfunction on pulmonary function 1, 2: Studies in patients with spinal cord injuries. Am Rev Respir Dis. 1963. 88: 621-9
43. Tator CH, Rowed DW. Current concepts in the immediate management of acute spinal cord injuries. Can Med Assoc J. 1979. 121: 1453-64
44. Thompson H The. “Halo” traction apparatus. A method of external splinting of the cervical spine after injury. J Bone Joint Surg. 1962. 44: 655-61
45. Turkstra TP, Craen RA, Pelz DM, Gelb AW. Cervical spine motion: A fluoroscopic comparison during intubation with lighted stylet, GlideScope, and Macintosh laryngoscope. Anesth Analg. 2005. 101: 910-5
46. Van Middendorp JJ, Slooff WB, Nellestein WR, Öner FC. Incidence of and risk factors for complications associated with halo-vest immobilization: A prospective, descriptive cohort study of 239 patients. J Bone Joint Surg Am. 2009. 91: 71-9
47. Velmahos G, Toutouzas K, Chan L, Tillo A, Rhee P, Murray J. Intubation after cervical spinal cord injury: To be done selectively or routinely?. Am Surg. 2003. 69: 891-4
48. Victor DI, Bresnan MJ, Keller RB. Brain abscess complicating the use of halo traction. J Bone Joint Surg Am. 1973. 55: 635-9
49. Vieweg U, Schultheiss R. A review of halo vest treatment of upper cervical spine injuries. Arch Orthop Trauma Surg. 2001. 121: 50-5
50. Wright SW, Robinson GG, Wright MB. Cervical spine injuries in blunt trauma patients requiring emergent intubation. Am J Emerg Med. 1992. 10: 104-9
51. Wylie WD. Hazards of intubation. Anaesthesia. 1950. 5: 143-8