- Department of Biomedicine Neurosciences and Advanced Diagnostic, University of Palermo, School of Medicine, Palermo, Sicily, Italy,
- Department of Neurosurgery, ARNAS Garibaldi, P.O. Garibaldi Nesima, Via Palermo, 636, Catania, Italy,
- Division of Neurosurgery, Villa Sofia Hospital, Palermo, Sicily, Italy.
Correspondence Address:
Lara Brunasso
Department of Biomedicine Neurosciences and Advanced Diagnostic, University of Palermo, School of Medicine, Palermo, Sicily, Italy,
DOI:10.25259/SNI_340_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lara Brunasso1, Luigi Basile1, Domenico Gerardo Iacopino1, Carlo Gulì1, Francesca Graziano1, Maria Angela Pino1, Giovanni Federico Nicoletti2, Silvana Tumbiolo3, Rosario Maugeri1. All that glitters is not gold: A spinal epidural empyema following epidural steroid injection. 08-Aug-2020;11:240
How to cite this URL: Lara Brunasso1, Luigi Basile1, Domenico Gerardo Iacopino1, Carlo Gulì1, Francesca Graziano1, Maria Angela Pino1, Giovanni Federico Nicoletti2, Silvana Tumbiolo3, Rosario Maugeri1. All that glitters is not gold: A spinal epidural empyema following epidural steroid injection. 08-Aug-2020;11:240. Available from: https://surgicalneurologyint.com/surgicalint-articles/10186/
Abstract
Background: Therapeutic epidural spinal injections (ESIs) of steroids are one of the most common nonsurgical management modalities employed for alleviating pain due to chronic persistent lumbar spinal disease. However, it is well documented that they have significant risks and complications without any long-term efficacy. ESI may result in epidural empyema which may be difficult to diagnose with delays resulting in significant permanent neurological sequelae.
Case Description: A 45-year-old female presented with a lumbar spinal epidural empyema after receiving ESI for low back and right leg pain due to a lumbar disc herniation. Laboratory studies showed elevations of multiple inflammatory markers, and the MR documented a significant lumbar epidural empyema contributing to significant thecal sac compression. Clinically, the patient had an acute cauda equina syndrome warranting emergency surgery consisting of a laminectomy for debridement/decompression followed by long-term antibiotic treatment.
Conclusion: Epidural empyema is a major potential complication of lumbar ESI. Multiple markedly elevated inflammatory markers (WBC, ESR, CRP, and procalcitonin) and MRI evidence of an epidural empyema necessitates emergent surgical intervention to limit morbidity, neurological sequelae, and mortality.
Keywords: Lumbar degenerative disease, Pain management, Spinal epidural abscess, Spinal infection, Spinal procedure
INTRODUCTION
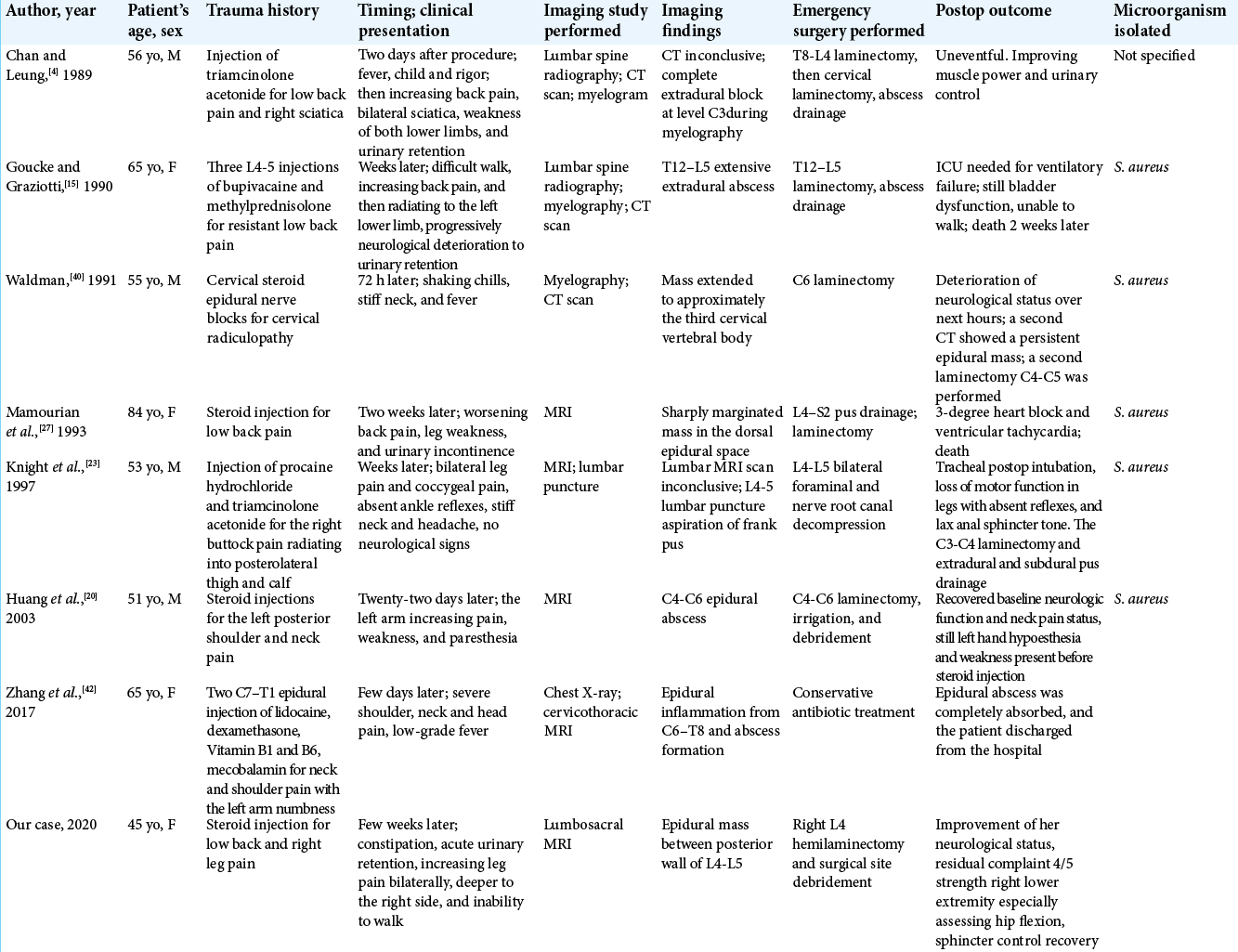
Spinal epidural empyema (SEE), also called spinal epidural abscesses (SEA), posts a significant risk of neurological morbidity and mortality (e.g., rates of 4–31% worldwide).[
Here, we present a patient with an acute cauda equina syndrome due to an MR-documented L4- L5 SEE/SEA following a spinal epidural spinal injection (ESI).
CASE REPORT
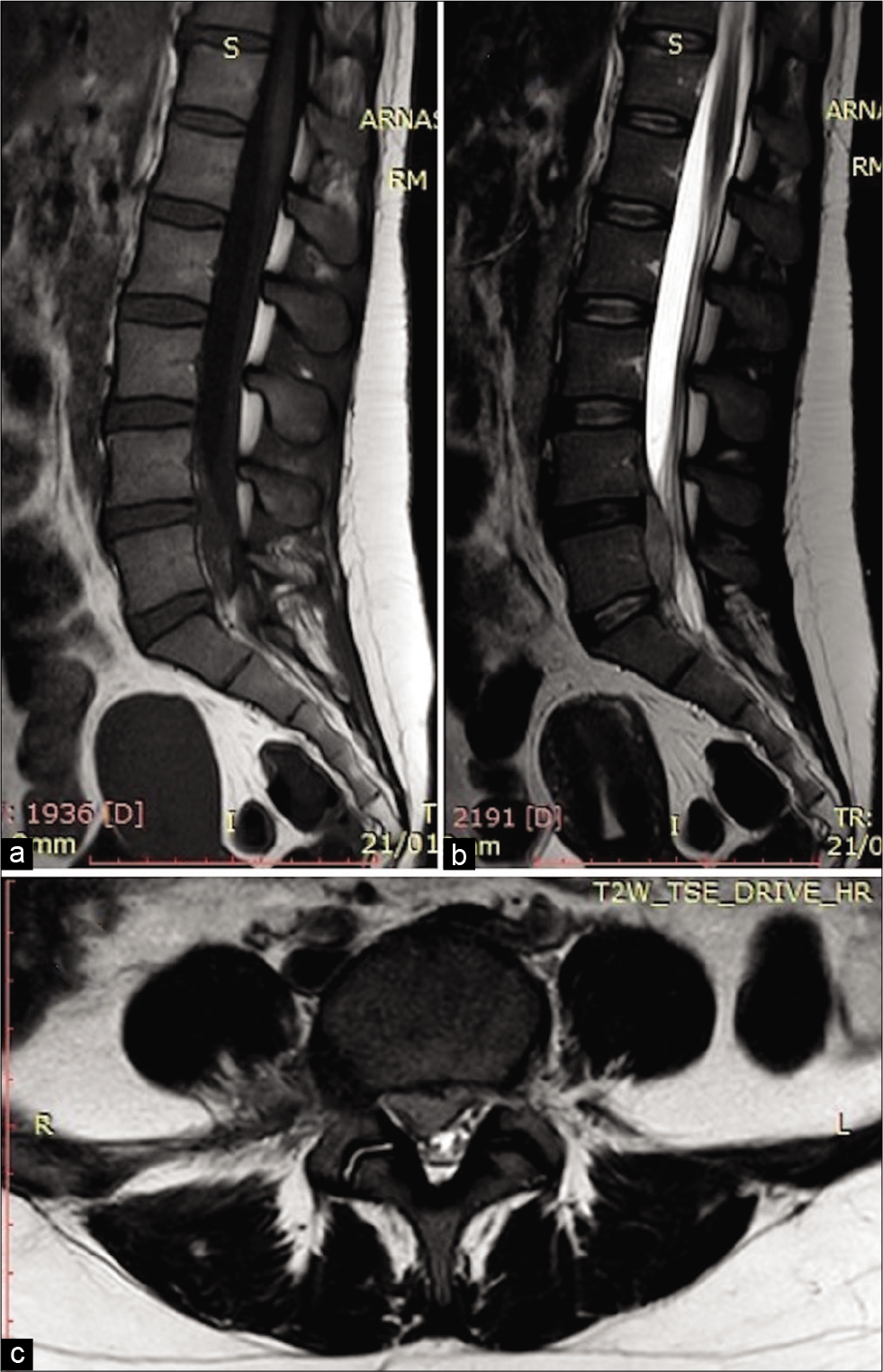
A 45-year-old female with a symptomatic lumbar disc herniation had an ESI. Over the next few weeks, she complained constipation with increasing leg pain and the progressive inability to walk; she finally developed in acute urinary retention. On examination, she had a cauda equina syndrome; 3/5 motor function in both lower extremities, with perineal hypoesthesia. Laboratory studies showed a high white blood cell count of 19.79 × 103/ml, while the emergent lumbar MRI without gadolinium showed an anterior epidural L4-L5-S1 empyema/abscess (e.g., low signal on T1- and a high signal in T2-weighted images) with marked thecal sac/root compression [
Figure 1:
Preoperative emergency MRI without gadolinium. In (a), the sagittal T1-weighted image provides suboptimal visualization of epidural abscess. In (b), the sagittal T2-weighted image demonstrates a longitudinally oriented mass-like lesion in the anterior epidural space spreading between the posterior wall of L4 and L5. In (c), the axial T2-weighted image demonstrates right side epidural abscess compressing both the cauda equina and right L5 and S1 emergent nerve roots.
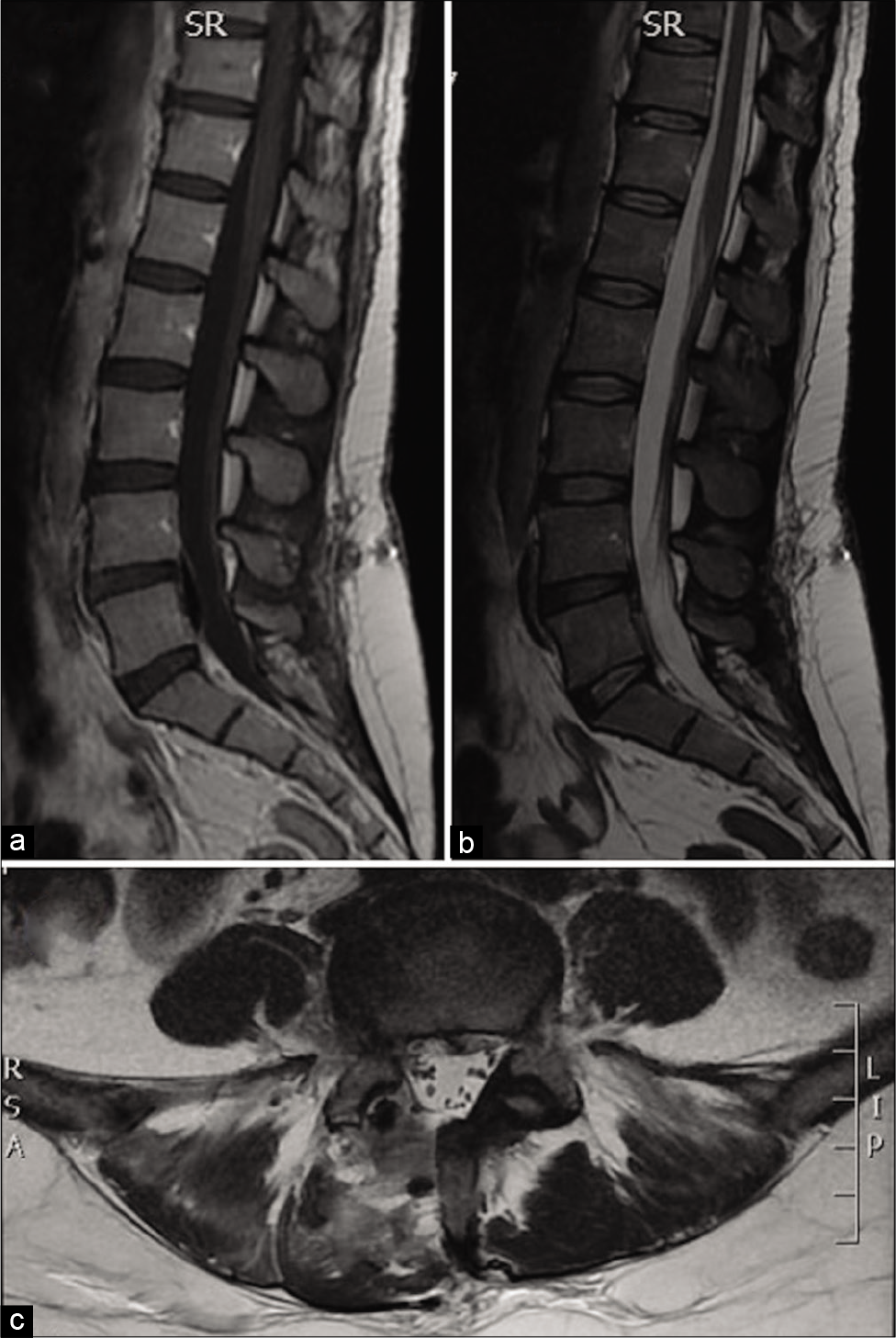
The presumptive initial vancomycin and ceftazidime were changed to clindamycin and gentamicin to address the methicillin-resistant Staphylococcus aureus and Streptococcus parasanguinis. The 3-day postoperative lumbar MRI documented adequate decompression of the cauda equina [
Figure 2:
Three days postoperative MRI without gadolinium. In (a), the sagittal T1-weighted image, in (b), the sagittal T2-weighted image, in (c), the axial T2-weighted image demonstrate marked reduction of the preoperative empyema mass at L4 and L5 level in the anterior epidural space with consensual reduction of the compression on the adjoining meningeal and neural structures.
DISCUSSION
Despite the lack of documented safety and efficacy[
The classical triad of SEE/SEA includes fever, back pain, and neurological deficits which may rapidly progress to quadriplegia/paraplegia. Laboratory studies usually show elevated WBC counts and increased ESR, CRP, and procalcitonin levels.[
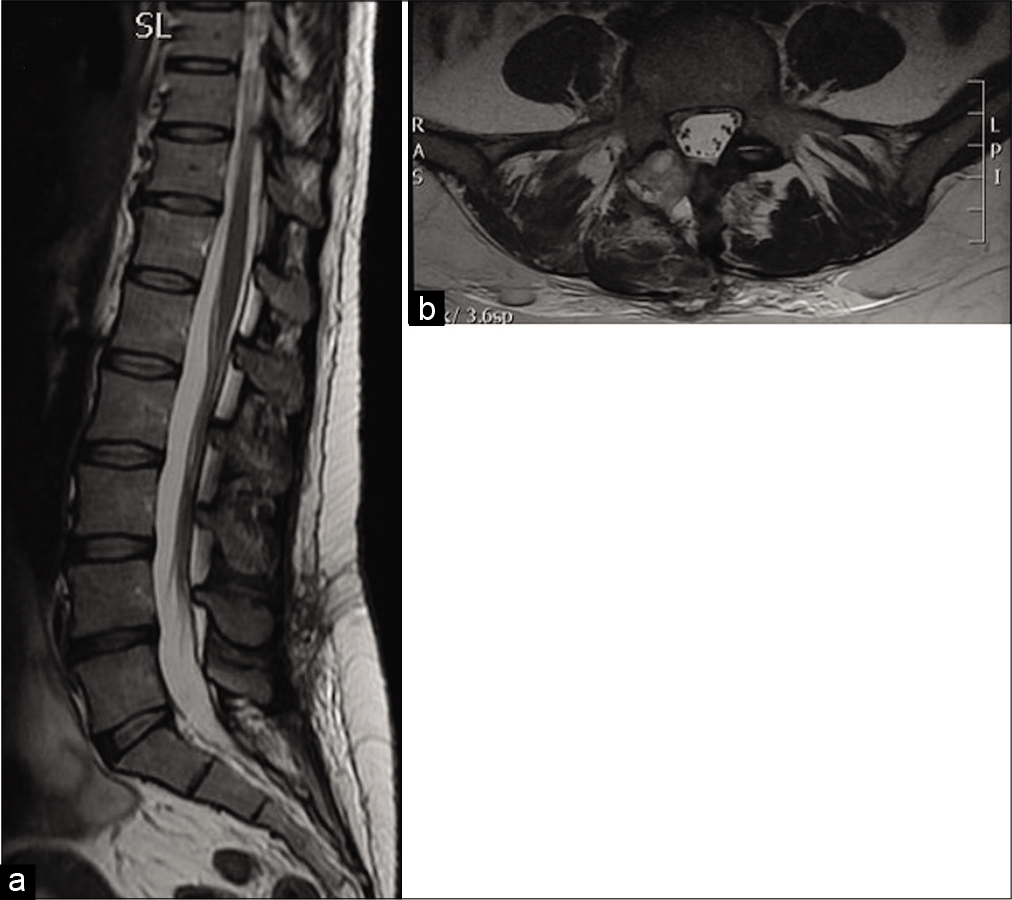
Enhanced MRI remains the study of choice for documenting SEE/SEA that is most frequently found in the thoracic (48%), lumbar (31%), and cervical regions.[
[
Following spinal ESI, patients generally present within few weeks with back pain, fever, radiculopathies, and/or myelopathy. Enhanced MRI studies are the examinations of choice as they will demonstrate show epidural infections within 2–4 weeks; X-rays and CT studies will take up to 6–10 weeks to show abnormalities.[
Here, the patient presented with pain, fever, and a neurological deficit (3/5 motor function of RLE), perineal hypoesthesia, and urinary retention. Once abnormally elevated laboratory inflammatory markers and an MR confirming an anterior L4-S1 epidural empyema were obtained, an emergent decompressive hemilaminectomy was performed that largely resolved the patient’s preoperative deficits. Sample biopsy was crucial to maximize efficacy, tailored antibiotic therapy, and limit resistance.
CONCLUSION
SEE diagnosis should be suspected in a patient presenting with the classic triad of back pain, fever, and a neurological deficit, associated with elevated laboratory inflammatory markers and MRI findings of significant epidural spinal compression. This clinical picture should prompt early neurosurgical intervention/decompression to minimize long-term neurological sequelae.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ackerman WE, Ahmad M. The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg. 2007. 104: 1217-22
2. Arko L, Quach E, Nguyen V, Chang D, Sukul V, Kim BS. Medical and surgical management of spinal epidural abscess: A systematic review. Neurosurg Focus. 2014. 37: E4
3. Benny B, Azari P, Briones D. Complications of cervical transforaminal epidural steroid injections. Am J Phys Med Rehabil. 2010. 89: 601-7
4. Chan ST, Leung S. Spinal epidural abscess following steroid injection for sciatica. Case report. Spine (Phila Pa 1976). 1989. 14: 106-8
5. Chou R, Huffman L.editors. Guideline for the Evaluation and Management of Low Back Pain: Evidence Review. Glenview, IL: American Pain Society; 2009. p.
6. Crowest PR, Hughes PJ, Elkins A, Jackson M, Ranu H. A rare presentation of spinal epidural abscess. BMJ Case Rep. 2011. 2011: bcr0820114647
7. Curry WT, Hoh BL, Amin-Hanjani S, Eskandar EN. Spinal epidural abscess: Clinical presentation, management, and outcome. Surg Neurol. 2005. 63: 364-71
8. Darouiche RO. Spinal epidural abscess and subdural empyema. Handb Clin Neurol. 2010. 96: 91-9
9. Davis DP, Wold RM, Patel RJ, Tran AJ, Tokhi RN, Chan TC. The clinical presentation and impact of diagnostic delays on emergency department patients with spinal epidural abscess. J Emerg Med. 2004. 26: 285-91
10. Duarte RM, Vaccaro AR. Spinal infection: State of the art and management algorithm. Eur Spine J. 2013. 22: 2787-99
11. Epstein NE. Major risk and complications of cervical epidural steroid injections: An updated review. Surg Neurol Int. 2018. 9: 86
12. Euba G, Narvaez JA, Nolla JM, Maurillo O, Narvaez J, Gomez-Vaquero C. Long-term clinical and radiological magnetic resonance imaging outcome of abscess-associated spontaneous pyogenic vertebral osteomyelitis under conservative management. Semin Arthritis Rheum. 2008. 38: 28-40
13. Friedly JL, Comstock BA, Turner JA, Heagerty PJ, Deyo RA, Sullivan SD. A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med. 2014. 371: 11-21
14. Goucke CR, Graziotti P. Extradural abscess following local anaesthetic and steroid injection for chronic low back pain. Br J Anaesth. 1990. 65: 427-9
15. Govender S. Spinal infections. J Bone Joint Surg. 2005. 87: 1454-8
16. Greenberg MS.editors. The Handbook of Neurosurgery. New York: Thieme; 2016. p.
17. Grieve JP, Ashwood N, O’Neill KS, Moore AJ. A retrospective study of surgical and conservative treatment for spinal extradural abscess. Eur Spine J. 2000. 9: 67-71
18. Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ. Hematogenous pyogenic spinal infections and their surgical management. Spine. 2000. 25: 1668-79
19. Harrast MA. Epidural steroid injections for lumbar spinal stenosis. Curr Rev Musculoskelet Med. 2008. 1: 32-8
20. Huang RC, Gary SS, Lim M, Sandhu HS, Lutz GE, Herzog RJ. Cervical epidural abscess after epidural steroid injection. Spine. 2004. 29: E7-9
21. Joshi SM, Hatfield RH, Martin J, Taylor W. Spinal epidural abscess: A diagnostic challenge. Br J Neurosurg. 2003. 17: 150-3
22. Khanna RK, Malik GM, Rock JP, Rosenblum ML. Spinal epidural abscess: Evaluation of factors influencing outcome. Neurosurgery. 1996. 39: 958-64
23. Knight JW, Cordingley JJ, Palazzo MG. Epidural abscess following epidural steroid and local anaesthetic injection. Anaesthesia. 1997. 52: 576-85
24. Kraeutler MJ, Bozzay JD, Walker MP, John K. Spinal subdural abscess following epidural steroid injection. J Neurosurg Spine. 2015. 22: 90-3
25. Lener S, Hartmann S, Barbagallo GM, Certo F, Thomé C. Management of spinal infection: A review of the literature. Acta Neurochir (Wien). 2018. 160: 487-96
26. Leys D, Lesoin F, Viaud C, Pasquier F, Rousseaux M, Jomin M. Decreased morbidity from acute bacterial spinal epidural abscesses using computed tomography and nonsurgical treatment in selected patients. Ann Neurol. 1985. 17: 350-5
27. Mamourian AC, Dickman CA, Drayer BP, Sonntag VK. Spinal epidural abscess: Three cases following spinal epidural injection demonstrated with magnetic resonance imaging. Anesthesiology. 1993. 78: 204-7
28. Mampalam TJ, Rosegay H, Andrews BT, Rosenblum ML, Pitts LH. Nonoperative treatment of spinal epidural infections. J Neurosurg. 1989. 71: 208-10
29. Manchikanti L, Ramsin MB, Falco FJ, Alan DK, Joshua AH. Do epidural injections provide short-and long-term relief for lumbar disc herniation? A systematic review. Clin Orthop Relat Res. 2015. 473: 1940-56
30. Patel AR, Alton TB, Bransford RJ, Lee MJ, Bellabarba CB, Chapman JR. Spinal epidural abscesses: Risk factors, medical versus surgical management, a retrospective review of 128 cases. Spine J. 2014. 14: 326-30
31. Pereira CE, Lynch JC. Spinal epidural abscess: An analysis of 24 Cases. Surg Neurol. 2005. 63: S26-9
32. Pilkington SA, Jackson SA, Gillett GR. Spinal epidural empyema. Br J Neurosurg. 2003. 17: 196-200
33. Pradilla G, Ardila GP, Hsu W, Rigamonti D. Epidural abscesses of the CNS. Lancet Neurol. 2009. 8: 292-300
34. Reihasaus E, Waldbaur H, Seeling W. Spinal epidural abscess: A meta-analysis of 915 patients. Neurosurg Rev. 2000. 232: 175-204
35. Rigamonti D, Liem L, Sampath P, Knoller N, Namaguchi Y, Schreibman DL. Spinal epidural abscess: Contemporary trends in etiology, evaluation, and management. Surg Neurol. 1999. 52: 189-96
36. Sagar S, Wilkinson JR, Erickson BJ, Temesgen Z, Boeve BF. Extensive S aureus spinal epidural empyema. Neurology. 2005. 65: 1970
37. Tan LA, Kasliwai MK, Deutsch H. Complications associated with epidural steroid injection. J Neurosurg Spine. 2015. 22: 558-60
38. Tanj HJ, Lin HJ, Liu YC, Li CM. Spinal epidural abscess-experience with 46 patients and evaluation of prognostic factors. J Infect. 2002. 45: 76-81
39. Vakili M, Crum-Cianflone NF. Spinal epidural abscess: A series of 101 Cases. Am J Med. 2017. 130: 1458-63
40. Waldman SD. Cervical epidural abscess after cervical epidural nerve block with steroids. Anesth Analg. 1991. 72: 717-8
41. Watters WC, Resnick DK, Eck JC, Ghogawala Z, Mummaneni PV, Dailey AT. Guidelines update for the performance of fusion procedures for degenerative disease of the lumbar spine Part. 13. Injection therapies, low-back pain, and lumbar fusion. J Neurosurg Spine. 2014. 21: 79-90
42. Zhang JH, Wang ZL, Wan L. Cervical epidural analgesia complicated by epidural abscess: A case report and literature review. Medicine (Baltimore). 2017. 96: e7789