- Division of Neurosurgery, Riverside University Health System Medical Center, Moreno Valley, California, USA
- Division of Neurosurgery, Arrowhead Regional Medical Center, Colton, California, USA
- Graduate College of Biomedical Sciences, Western University of Health Sciences, California, USA
- College of Osteopathic Medicine of the Pacific, Western University of Health Sciences, California, USA
Correspondence Address:
Jason Duong
Division of Neurosurgery, Arrowhead Regional Medical Center, Colton, California, USA
College of Osteopathic Medicine of the Pacific, Western University of Health Sciences, California, USA
DOI:10.4103/sni.sni_3_18
Copyright: © 2019 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Jason Duong, Christopher J. Elia, Dan Miulli, Fanglong Dong, Andrew Sumida. An approach using the occipital parietal point for placement of ventriculoperitoneal catheters in adults. 22-Feb-2019;10:21
How to cite this URL: Jason Duong, Christopher J. Elia, Dan Miulli, Fanglong Dong, Andrew Sumida. An approach using the occipital parietal point for placement of ventriculoperitoneal catheters in adults. 22-Feb-2019;10:21. Available from: http://surgicalneurologyint.com/surgicalint-articles/9205/
Abstract
Background:Ventriculoperitoneal shunts (VPS) have been widely used in the management of hydrocephalus. As current investigations into optimal approaches are being studied in the pediatric population, no general consensus on cranial entry points has been established for the adults. We compare conventional posterior and frontal approaches with an occipital parietal point (OPP) on computerized tomography (CT) while analyzing its associated outcomes.
Methods:An Institutional Review Board (IRB) approved retrospective review was conducted on patients at a single institution between 1999 and 2016, with searches of CPT codes of 62223, 62230, 62258. The patient's lost to follow-up were excluded. Demographics, etiology of hydrocephalus, cranial entry points, and clinical outcomes (optimal placement, blood loss, operative time, malfunctions, or infections) were abstracted. Chi-square analyses were conducted to identify the association between treatment and clinical outcomes.
Results:Ninety-three adults (≥18 years old) patients were included in the final analysis that had clinic follow-up, average age was 40.8 ± 15.6 years, with 57.0% had catheters placed utilizing the OPP, and 43.0% using conventional landmarks. OPP had less rates of suboptimal placement (P = 0.0469), and was less likely to develop a mechanical malfunction (5.7% vs. 12.5%). There was no difference in operative time, blood loss, or infection rate.
Conclusions:Shunt malfunctions remain to be a common complication but can be reduced by optimal catheter positioning. The OPP established on computed tomography (CT) is just as safe as conventional landmarks, and can aid in optimal catheter positioning and can potentially reduce the risk of shunt malfunction secondary to suboptimal catheter placement.
Keywords: Cranial approaches, Frazier's point, hydrocephalus, intracranial catheters, Keen's point, Kocher's point, occipital parietal point, ventriculoperitoneal shunt
INTRODUCTION
Ventricular shunting has been widely used in the management of hydrocephalus. Each year there are 38,200–39,900 admissions, 391,000–433,000 hospital days, and total hospital charges of $1.4–2.0 billion for pediatric hydrocephalus, and while shunts have revolutionized the treatment of increased intracranial pressure, they have associated complications with more than 50% of pediatric patients have a shunt malfunction within 2 year of surgery.[
While predictors of shunt malfunction have been mostly studied in the pediatric population, there is little literature addressing factors and outcomes with ventricular shunt systems in adult patients with hydrocephalus. Also, no consensus regarding optimal intracranial catheter placement has been established with studies demonstrating mixed results between anterior and posterior approaches.[
MATERIALS AND METHODS
An Institutional Review Board (IRB) approved retrospective review was conducted at a single Level II trauma institution. Patients included in the review were 18 year-of-age or older that underwent placement or revision of a VPS between 1999 and 2016 and searches of CPT codes of 62223, 62230, 62258. Those lost to follow-up upon discharge were excluded. Patient demographics, etiology of hydrocephalus, catheter entry point, and associated clinical outcomes (catheter placement, blood loss, operative time, shunt malfunction, or shunt infections) were obtained. Two groups of patients were established based on catheter entry site. Patients with the OPP entry site were in Group A and patients with traditional entry sites (Kocher’s, Frazier’s, Keen’s) were in Group B.
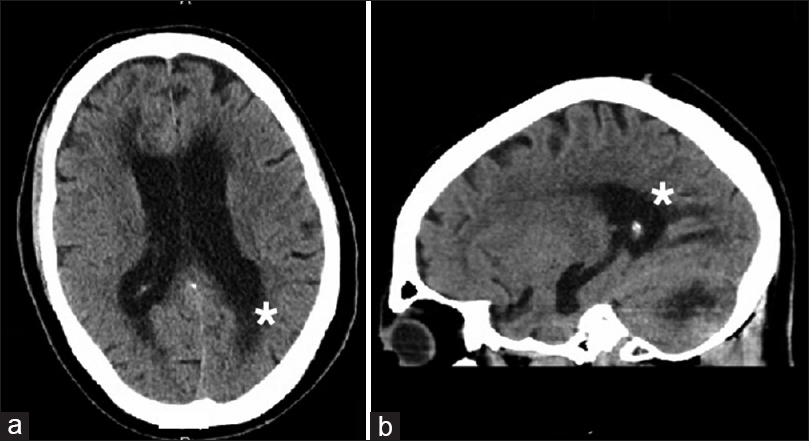
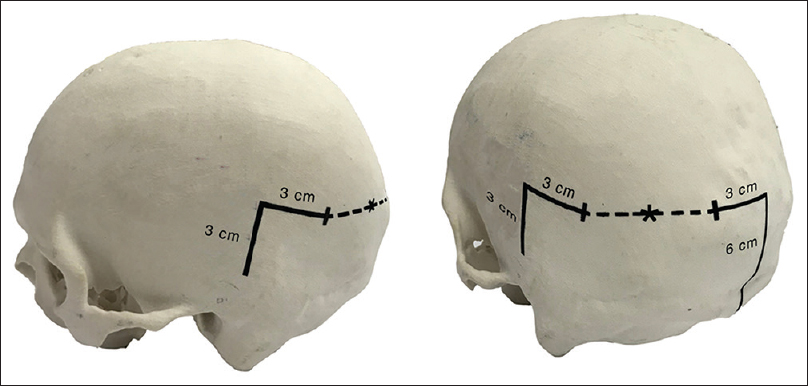
Radiographically, the OPP is determined by the point based on the trajectory with the shortest distance of traversing parenchyma from the skull to the atrium of the lateral ventricle [
Optimal placement as defined by this study is considered as catheter placement within the ipsilateral ventricle without crossing midline or contacting the septum pellucidum, choroid plexus, or terminating in brain parenchyma. Chi-square analyses were conducted to identify the association between treatment and clinical outcomes.
RESULTS
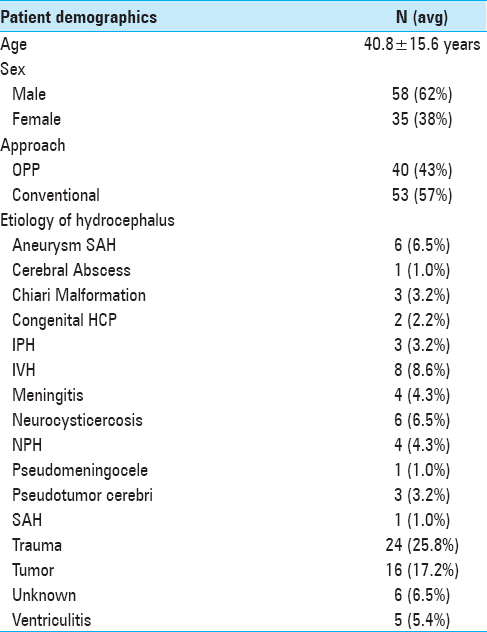
A total of 93 adults (≥18 years old) patients were included in the final analysis, 53 had catheters placed utilizing the OPP and 40 had catheters placed using other landmark entry points. The average age was 40.8 ± 15.6. The majority of adult patients who required a VPS were due to trauma (25.8%) causing communicating hydrocephalus, which included traumatic subarachnoid hemorrhages, intraparenchymal subdural, epidural hemorrhages, gunshot wounds, and those who required a decompressive craniectomy for refractory intracranial hypertension. The next common causes of hydrocephalus requiring VPS in our adult population are tumors (17.2%) then followed by intraventricular hemorrhages (8.6%) [
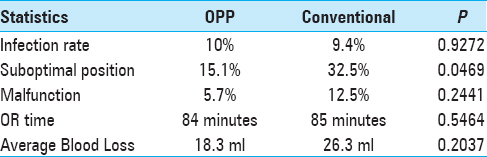
Among patients in Group A, 15.1% had suboptimal placement compared to 32.5% of patients in Group B (P = 0.0469). Additionally, Group A had less proximal catheter mechanical malfunctions compared to Group B (5.7% vs. 12.5%), although this did not achieve statistical significance. No difference was detected with infection rates (9.4% vs. 10%), OR time, and blood loss volume (18.3 mL vs. 26.3 mL) between the two groups [
DISCUSSION
Obstruction of the ventricular catheter is the most common reason for mechanical shunt failure in both pediatrics and adults, and it can be caused by proteinaceous cerebrospinal fluid (CSF), debris, and more often obstruction by the ventricular wall or choroid plexus and optimal catheter placement can reduce the rate of proximal failure.[
Ventricular catheter approaches have been investigated for optimal outcomes with mixed results and current studies are being conducted to investigate anterior versus posterior entry points.[
In addition to reducing malfunction rates, improved positioning can reduce the need for additional surgical procedures for revision. Shunting procedures cost the United States more than 1 billion each year, where predominantly the costs arise from complication and revision rates.[
This study provides insight into different surgical options pertaining to entry point for VPS placement; however, this study is not without its limitations. The study would be strengthened if it were a randomized controlled study while comparing to separate traditional entry sites, as well as increasing the number of patients for statistical significance. Due to its retrospective nature, this study includes patients with different etiologies of hydrocephalus which allow confounding variables to influence outcomes and also there may be confounding CPT codes. Lastly, the study may have been strengthened if it were a single-surgeon study, rather than a multiple-surgeon study.
CONCLUSION
We describe the OPP as a safe alternative to shunt entry site. We are able to obtain a higher a higher rate of optimal catheter positioning when using this method at out single institution. Although, no entry point or method has been established as superior when compared to others, we hope that this study leads to future randomized controlled studies comparing different modalities.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Albright AL, Haines SJ, Taylor FH. Function of parietal and frontal shunts in childhood hydrocephalus. J Neurosurg. 1988. 69: 883-6
2. Bierbrauer KS, Storrs BB, McLone DG, Tomita T, Dauser R. A prospective, randomized study of shunt function and infections as a function of shunt placement. Pediatr Neurosurg. 1990. 16: 287-91
3. Colak A, Albright AL, Pollack IF. Follow-up of children with shunted hydrocephalus. Pediatr Neurosurg. 1997. 27: 208-10
4. Drake JM, Kestle JR, Milner R, Cinalli G, Boop F, Piatt J. Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery. 1998. 43: 294-303
5. Drake JM, Kestle JR, Tuli S. CSF shunts 50 years on--past, present and future. Childs Nerv Syst. 2000. 16: 800-4
6. Jeremiah KJ, Cherry CL, Wan KR, Toy JA, Wolfe R, Danks RA. Choice of valve type and poor ventricular catheter placement: Modifiable factors associated with ventriculoperitoneal shunt failure. J Clin Neurosci. 2016. 27: 95-8
7. Korinek A-M, Fulla-Oller L, Boch A-L, Golmard J-L, Hadiji B, Puybasset L. Morbidity of ventricular cerebrospinal fluid shunt surgery in adults: An 8-year study. Neurosurgery. 2011. 68: 985-94
8. Parker SL, McGirt MJ, Murphy JA, Megerian JT, Stout M, Engelhart L. Cost savings associated with antibiotic-impregnated shunt catheters in the treatment of adult and pediatric hydrocephalus. World Neurosurg. 2015. 83: 382-6
9. Pham ACQ, Fan C, Owler BK. Treating pediatric hydrocephalus in Australia: A 3-year hospital-based cost analysis and comparison with other studies. J Neurosurg Pediatr. 2013. 11: 398-401
10. Sekhar LN, Moossy J, Guthkelch AN. Malfunctioning ventriculoperitoneal shunts. Clinical and pathological features. J Neurosurg. 1982. 56: 411-6
11. Shannon CN, Simon TD, Reed GT, Franklin FA, Kirby RS, Kilgore ML. The economic impact of ventriculoperitoneal shunt failure. J Neurosurg Pediatr. 2011. 8: 593-9
12. Simon TD, Riva-Cambrin J, Srivastava R, Bratton SL, Dean JM, Kestle JRW. Hospital care for children with hydrocephalus in the United States: Utilization, charges, comorbidities, and deaths. J Neurosurg Pediatr. 2008. 1: 131-7
13. Stone JJ, Walker CT, Jacobson M, Phillips V, Silberstein HJ. Revision rate of pediatric ventriculoperitoneal shunts after 15 years. J Neurosurg Pediatr. 2013. 11: 15-9
14. Villavicencio AT, Leveque J-C, McGirt MJ, Hopkins JS, Fuchs HE, George TM. Comparison of revision rates following endoscopically versus nonendoscopically placed ventricular shunt catheters. Surg Neurol. 2003. 59: 375-9
15. Whitehead WLast accessed on 25 April 2017. Available: http://www.pcori. org/research-results/2014/randomized-controlled-trial-anterior-versus-pos terior-entry-site-cerebrospinal.
16. Whitehead WE, Riva-Cambrin J, Kulkarni AV, Wellons JC, Rozzelle CJ, Tamber MS. Ventricular catheter entry site and not catheter tip location predicts shunt survival: A secondary analysis of 3 large pediatric hydrocephalus studies. J Neurosurg Pediatr. 2017. 19: 157-67
17. Wilson TJ, McCoy KE, Al-Holou WN, Molina SL, Smyth MD, Sullivan SE. Comparison of the accuracy and proximal shunt failure rate of freehand placement versus intraoperative guidance in parietooccipital ventricular catheter placement. Neurosurg Focus. 2016. 41: E10-
18. Yamada SM, Kitagawa R, Teramoto A. Relationship of the location of the ventricular catheter tip and function of the ventriculoperitoneal shunt. J Clin Neurosci. 2013. 20: 99-101