- Department of Surgery, Section of Neurosurgery, University of Chicago, Chicago, USA
- Department of Neurosurgery, Northshore University Health System, Evanston, Illinois, USA
- Department of Neurology, Northshore University Health System, Evanston, Illinois, USA
Correspondence Address:
Ricky H. Wong
Department of Neurosurgery, Northshore University Health System, Evanston, Illinois, USA
DOI:10.4103/sni.sni_190_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Sean P. Polster, Shirlene Obuobi, Victor J. Del Brutto, Kenneth Avner, Aikaterini Markopoulou, Ricky H. Wong. An unusual presentation of dystonia and chorea from intraventricular pneumocephalus. 21-Sep-2018;9:193
How to cite this URL: Sean P. Polster, Shirlene Obuobi, Victor J. Del Brutto, Kenneth Avner, Aikaterini Markopoulou, Ricky H. Wong. An unusual presentation of dystonia and chorea from intraventricular pneumocephalus. 21-Sep-2018;9:193. Available from: http://surgicalneurologyint.com/surgicalint-articles/9016/
Abstract
Background:Pneumocephalus is a common finding following intracranial procedures, typically asymptomatic and resolves within several days. However, in some cases, pneumocephalus presents with headache, encephalopathy, or symptoms of elevated intracranial pressure. Here, we present a case of iatrogenic tension pneumocephalus following endoscopic sinus surgery, presenting as abnormal involuntary movements resembling a movement disorder with choreiform movements.
Case Description:A 67-year-old previously healthy male presented with new onset chorea and dystonia associated with headache, encephalopathy, and postural instability 4 days after undergoing endoscopic sinus surgery for chronic sinusitis and nasal polyps. Computed tomography showed prominent intraventricular pneumocephalus causing enlargement of the anterior horns of both lateral ventricles with lateral displacement of the basal ganglia nuclei and a bony defect in the skull base. Neurosurgical correction of the cranial defect provided complete symptomatic resolution. Pneumocephalus as a result of an iatrogenic injury of the skull base manifesting as an acute movement disorder is a rare complication of a nasal sinus procedure. We speculate that compression of the caudate nucleus and striatum resulted in decreased pallidothalamic inhibition and thalamocortical disinhibition leading to the development of a hyperkinetic movement disorder.
Conclusion:This unusual presentation of a common procedure illustrates a neurological emergency that requires prompt recognition and timely correction.
Keywords: All movement disorders, clinical neurological examination, dystonia
INTRODUCTION
Tension pneumocephalus resulting in caudate compression is a unique etiology of choreiform movements.
CASE DESCRIPTION
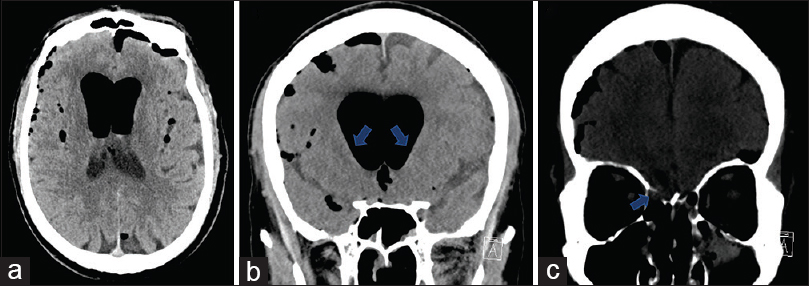
A 67-yeal-old man with no significant medical history presented to the emergency department (ED) with a one-day course of new onset headache, chorea, postural instability, and disorientation. Four days before presentation, he underwent endoscopic sinus surgery for chronic sinusitis and nasal polyps at an outpatient sinus surgery center. The operation was reported as uneventful and he was discharged home neurologically intact. No medications were prescribed nor used without prescription by the patient. Three days after surgery, the patient developed bilateral frontal headache associated with poor movement control, inability to ambulate or operate his automobile. At arrival to the ED, he was afebrile, hemodynamically stable, and in no acute distress. On neurological examination, he was awake, but inattentive, oriented to self and place but not time. There was no nuchal rigidity and cranial nerves were intact. He was noted to have involuntary chorea-like movements of the neck and shoulders as well as dystonic posturing of his right arm and neck. His muscle strength was preserved and tone was increased in the lower extremities. Right patellar hyperreflexia, right ankle clonus, and right extensor plantar response were present. Sensory examination was unremarkable. He was unable to stand due to significant postural instability. Clear fluid rhinorrhea was noted during the exam. Computed tomography on presentation showed prominent pneumocephalus with intraventricular air causing enlargement of the anterior horns of both lateral ventricles with lateral displacement of the basal ganglia nuclei bilaterally [
Figure 1
Nonenhanced computerized tomography scans showing in the (a) axial and (b) coronal planes, extra-axial, subarachnoid, and intraventricular air (arrows in b shows depression of the ventricular wall causing distortion of the bilateral caudate nuclei). (c) Coronal computerized tomography scan with arrow depicting bony defect caused by iatrogenic transgression of the fovea ethmoidalis
DISCUSSION
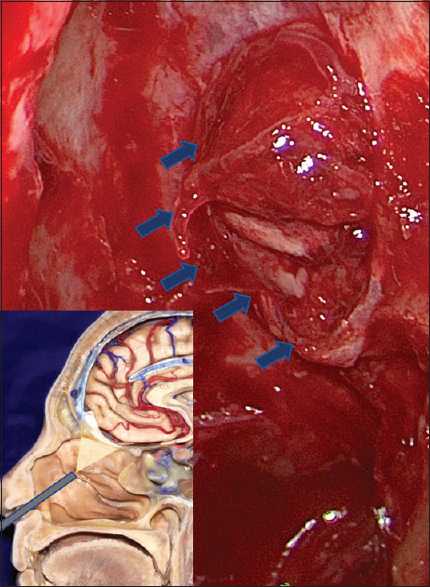
Pneumocephalus as a result of an iatrogenic injury of the skull base presenting as an acute movement disorder is a rare complication of a nasal sinus procedure. This complication resulted from the violation of the subdural and subarachnoid compartments resulting in CSF drainage and intraventricular accumulation of air under pressure. The intraventricular air caused lateral ventricle distortion that compressed and displaced the bilateral basal ganglia nuclei inferolaterally.
Pneumocephalus is a routine radiographic finding after intracranial procedures, usually asymptomatic and resolves within days. Infrequently, iatrogenic violation of the dura with subsequent CSF loss results in a “valve” phenomenon with intracranial accumulation of air that can cause mass effect on surrounding structures. A dramatic example is the “Mt Fuji sign” with bilateral frontal lobe compression. Further communication to the ventricular system and subarachnoid space can lead to intraventricular accumulation of air and progressive neurological deterioration.[
Historically, isolated intraventricular air was most commonly encountered after pneumoencephalography. Neurological complications of this air procedure lack a particular pattern and include headaches, alteration of consciousness, and seizures as well as abnormal pyramidal and extrapyramidal system involvement.[
Lutjens and colleagues reported a single case of akinetic mutism and Parkinsonism associated with tension pneumocephalus after decompression of a subdural hygroma where downward pressure distorted the frontal hemispheres and deep nuclei.[
This presentation illustrates a neurosurgical emergency that requires prompt recognition and intervention.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Gönül E, Izci Y, Sali A, Baysefer A, Timurkaynak E. Subdural and intraventricular traumatic tension pneumocephalus: Case report. Minim Invasive Neurosurg. 2000. 43: 98-101
2. Hantraye P, Riche D, Maziere M, Isacson O. A primate model of Huntington's disease: Behavioral and anatomical studies of unilateral excitotoxic lesions of the caudate-putamen in the baboon. Exp Neurol. 1990. 108: 91-104
3. Lin JJ. Generalized chorea in the syndrome of acute bilateral basal ganglia lesions in patients with diabetic uremia. J Clin Neurosci. 2011. 18: 1266-8
4. Lütjens G, Capelle HH, Krauss JK. Akinetic mutism and parkinsonism due to subdural and intraventricular tension pneumocephalus. J Neurol Surg A Cent Eur Neurosurg. 2013. 74: e116-8
5. Mammis A, Agarwal N, Eloy JA, Liu JK. Intraventricular tension pneumocephalus after endoscopic skull base surgery. J Neurol Surg A Cent Eur Neurosurg. 2013. 74: e96-9
6. Martínez-Capoccioni G, Serramito-García R, Cabanas-Rodríguez E, García-Allut A, Martín-Martín C. Tension pneumocephalus as a result of endonasal surgery: An uncommon intracranial complication. Eur Arch Otorhinolaryngol. 2014. 271: 1043-9
7. Pillai P, Sharma R, MacKenzie L, Reilly EF, Beery PR, Papadimos TJ. Traumatic tension pneumocephalus – Two cases and comprehensive review of literature. Int J Crit Illn Inj Sci. 2017. 7: 58-64
8. White YS, Bell DS, Mellick R. Sequelae to pneumoencephalography. J Neurol Neurosurg Psychiatry. 1973. 36: 146-51