- Pars Advanced and Minimally Invasive Medical Manners Research Center, Pars Hospital, Iran University of Medical Sciences, R&D Committee Office, Pars Advanced and Minimally Invasive Medical Manners Research Center, Tehran, Iran, Islamic Republic of Iran.
DOI:10.25259/SNI_157_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abolfazl Rahimizadeh, Saeed Ehteshami, Ava Rahimizadeh, Mona Karimi. Anterior sacral meningocele complicated by rectothecal fistula and rectorrhea: A Case report and review of the literature. 16-May-2020;11:117
How to cite this URL: Abolfazl Rahimizadeh, Saeed Ehteshami, Ava Rahimizadeh, Mona Karimi. Anterior sacral meningocele complicated by rectothecal fistula and rectorrhea: A Case report and review of the literature. 16-May-2020;11:117. Available from: https://surgicalneurologyint.com/surgicalint-articles/10033/
Abstract
Background: Anterior sacral meningocele (ASM) is a rare congenital anomaly. It is characterized by herniation of the dura through a defect in the anterior sacrum. Rarely, however, it may extend to the rectal area through a rectothecal fistula with or without rectorrhea.
Case Description: Here, we present a case of ASM associated with a rectothecal fistula and rectorrhea. Surgical closure of the ostium of the cyst through a posterior approach resulted in long-term improvement
Conclusion: An ASM with both rectothecal fistula and rectorrhea is extremely rare.
Keywords: Anterior sacral meningocele, En block sacrum laminotomy, Mini plate, MRI, Rectothecal fistula, Sacrum reconstruction
INTRODUCTION
Anterior sacral meningocele (ASM) is a rare congenital anomaly characterized by dural herniation through a defect in the anterior sacrum.[
Here, we present a 24-year-old female with ASM, a rectothecal fistula, and rectorrhea, who was successfully treated with a single-stage posterior approach.
CASE REPORT
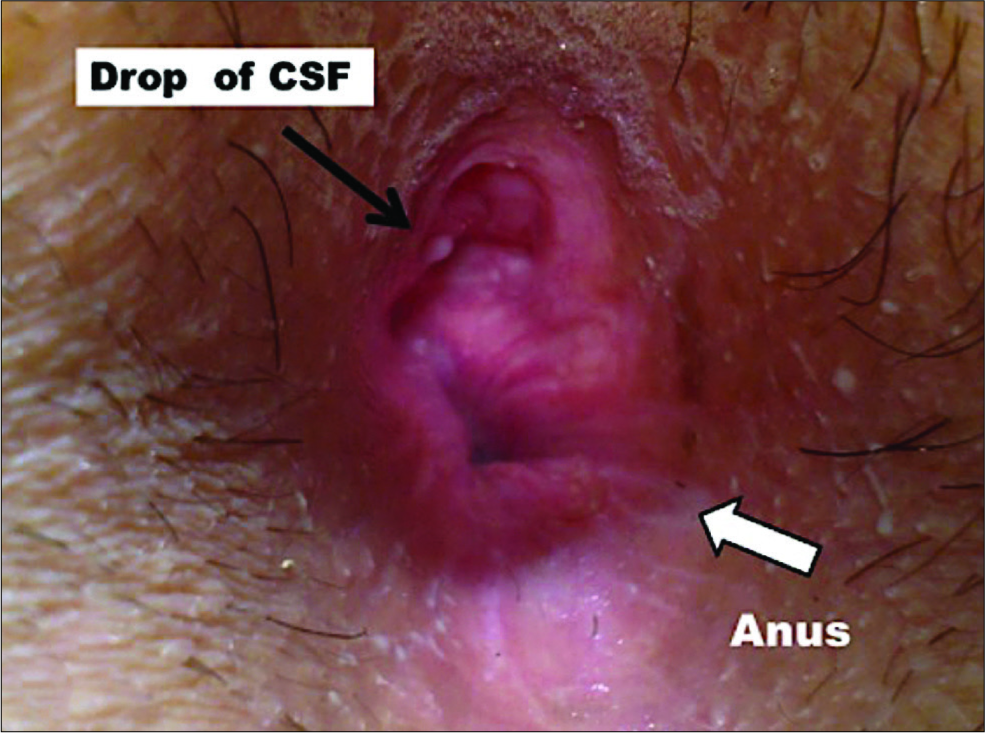
A 24-year-old female complained of intermittent watery discharge from her anus over the past 12 months. On examination, she had a fistula posterior to the anus through which a drop of clear watery liquid extruded utilizing a Valsalva maneuver [
Surgery
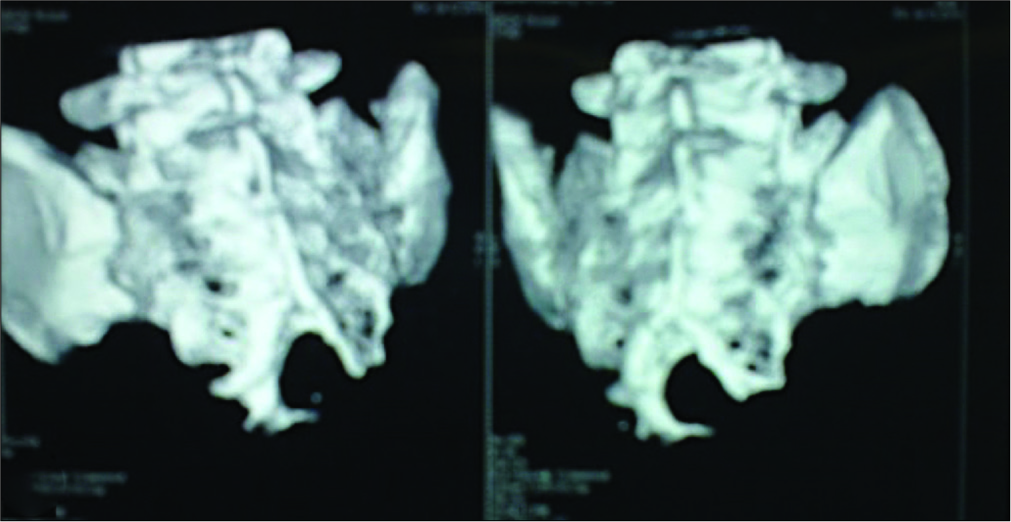
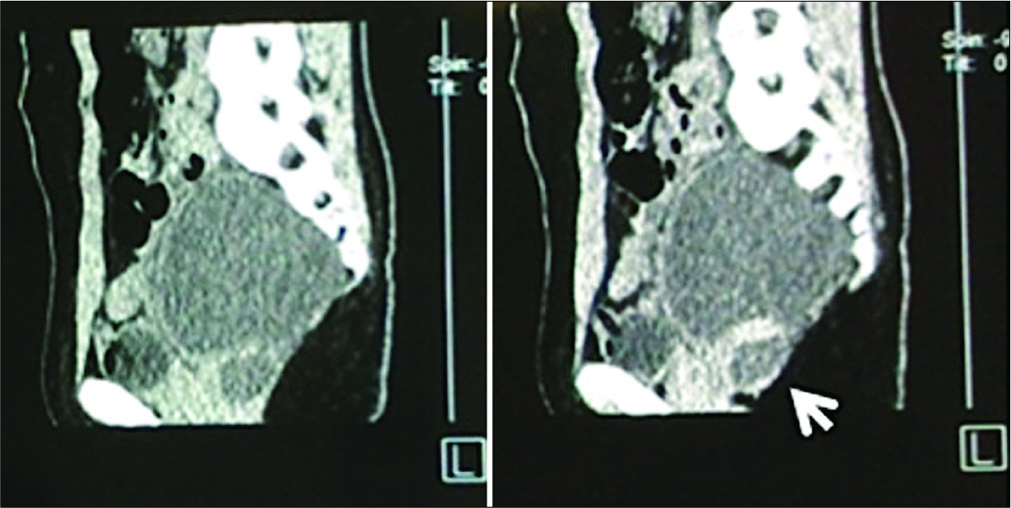
Through a midline posterior incision from S1 to sacral hiatus, en block laminotomies were performed. At the caudal side of the thecal sac and the level of the scimitar defect, a narrow-necked ostium of the meningocele was identified, explored, ligated, and sectioned. Before the closure of the neck of the meningocele, CSF was aspirated. The bony defect was covered with the bone flap and affixed with mini plates [
Postoperative course
The postoperative course was uneventful; there were no complications. At 10-year follow-up, the rectal examination disclosed spontaneous closure of the fistula. The MRI also confirmed the complete resolution of the previously noted meningocele/fistula [
DISCUSSION
ASM is a rare congenital anomaly characterized by herniation of a meningocele sac into the presacral space through a sacral defect.[
Currarino syndrome
This congenital anomaly may be a part of Currarino’s triad, in which ASM coexists with sacral agenesis and anorectal malformation. Furthermore, associated with this anomaly are the following; duplication of the uterus, epidermoid or dermoid cysts, lipomas, and teratomas.[
Clinical picture
As ASM is not typically associated with cutaneous abnormalities or posterior spina bifida, many patients with ASM remain asymptomatic or show minor symptoms (e.g., constipation, dysuria, and dysmenorrhea pressure on the rectum, urinary bladder/female genital organ findings).[
In such cases, with rectothecal fistula and rectorrhea, leakage of watery fluid in the anorectal region may point to the proper diagnosis.[
Imaging
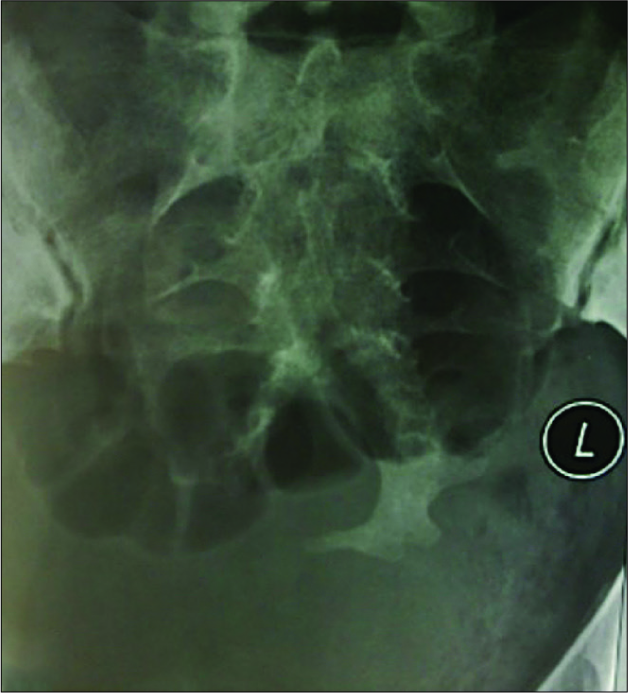
On plain radiographs, the scimitar sacrum, seen in 50% of cases, is the pathognomonic finding for ASM.[
Management
Surgical intervention for ASM is typically warranted.[
In addition to the posterior approach, an aggressive anterior surgical procedure may be warranted to address life- threatening meningitis and/or gross contamination.[
CONCLUSION
ASM with a rectothecal fistula with or without rectorrhea is extremely rare and should be fully evaluated preoperatively with MR/3D CT and myelo-CT studies, so they can be effectively and safely surgically corrected.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bergeron E, Roux A, Demers J, Vanier LE, Moore L. A 40-year-old woman with cauda equina syndrome caused by rectothecal fistula arising from an anterior sacral meningocele. Neurosurgery. 2010. 67: E1464-75
2. Clatterbuck RE, Jackman SV, Kavoussi LR, Long DM. Laparoscopic treatment of an anterior sacral meningocele. Case illustration. J Neurosurg. 2000. 92: 246-
3. Fitzpatrick MO, Taylor WA. Anterior sacral meningocele associated with a rectal fistula. Case report and review of the literature. J Neurosurg. 1999. 91: 124-7
4. Koksal A, Canyigit M, Kara T, Ulus A, Gokbayir H, Sarisahin M. Unusual presentation of an anterior sacral meningocele: Magnetic resonance imaging, multidetector computed tomography, and fistulography findings of bacterial meningitis secondary to a rectothecal fistula. Jpn J Radiol. 2011. 29: 528-
5. Mankotia DS, Sawarkar DP, Singh PK, Kumar A, Verma SK, Chandra PS. Rare case of cerebrospinal fluid proctorrhea caused by anterior sacral meningocele with rectothecal fistula. World Neurosurg. 2018. 114: 323-5
6. Massimi L, Calisti A, Koutzoglou M, Di Rocco C. Giant anterior sacral meningocele and posterior sagittal approach. Childs Nerv Syst. 2003. 19: 722-8
7. Phillips JT, Brown SR, Mitchell P, Shorthouse AJ. Anaerobic meningitis secondary to a rectothecal fistula arising from an anterior sacral meningocele: Report of a case and review of the literature. Dis Colon Rectum. 2006. 49: 1633-5
8. Sánchez AA, Iglesias CD, López CD, Cecilia DM, Gómez JA, Barbadillo JG. Rectothecal fistula secondary to an anterior sacral meningocele. J Neurosurg Spine. 2008. 8: 487-9