- Department of Neurosurgery, Lady Reading Hospital,
- Department of General Surgery, Hayatabad Medical Complex, Peshawar, Pakistan.
Correspondence Address:
Muhammad Shaheer Akhtar, Department of Neurosurgery, Lady Reading Hospital, Peshawar, Pakistan.
DOI:10.25259/SNI_237_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Riaz Ur Rehman1, Muhammad Shaheer Akhtar1, Amna Bibi2. Anterior transcervical release with posterior atlantoaxial fixation for neglected malunited type II odontoid fractures. 08-Apr-2022;13:132
How to cite this URL: Riaz Ur Rehman1, Muhammad Shaheer Akhtar1, Amna Bibi2. Anterior transcervical release with posterior atlantoaxial fixation for neglected malunited type II odontoid fractures. 08-Apr-2022;13:132. Available from: https://surgicalneurologyint.com/surgicalint-articles/11518/
Abstract
Background: Type 2 odontoid fractures are associated with a high rate of nonunion without surgical treatment. If neglected, they may become fixed in an abnormal position, causing progressive myelopathy. Conventionally, odontoidectomy or transoral release is performed to relieve symptoms in such cases. Here, were report our experience with a transcervical approach for odontoid release (i.e., of a chronically fractured dens) followed by a posterior C1–C2 fusion.
Methods: The 11 patients (2017–2021) retrospectively included; in this study, all had a history of remote trauma and the radiological appearance of an old odontoid fracture that was displaced and could not be reduced with traction. There were eight males and three females who averaged 52.6 years of age.
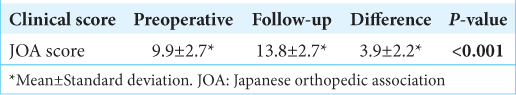
Results: All 11 patients underwent anterior retropharyngeal release with a C4–C5 level incision followed by a posterior C1–C2 fusion. The mean Japanese orthopedic association on presentation was 9.9 ± 2.7 which improved to 13.8 ± 2.7 on final follow-up (P
Conclusion: Anterior release through a retropharyngeal approach coupled with posterior C1–C2 instrumentation proved to be an effective alternative to the traditional transoral approach to treat a chronic malunited odontoid fracture.
Keywords: Atlantoaxial instability, IAAD, Irreducible atlantoaxial dislocation, Irreducible dislocation, Odontoid fracture
INTRODUCTION
C2 fractures comprise 9–20% of all cervical spine fractures.[
MATERIALS AND METHODS
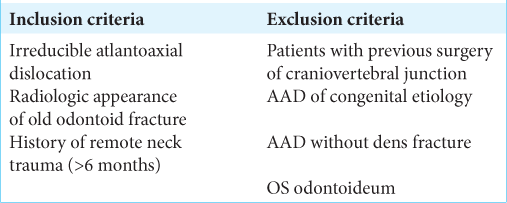
Demographics and patient presentations
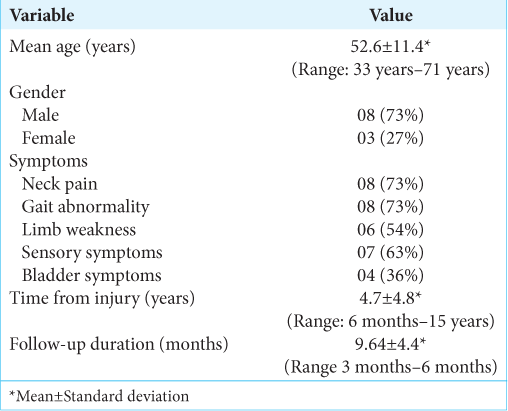
Of the 11 patients included in this study, there were eight males and three females. The mean age was 52.6 years (33–71 years). All patients had a history of head or neck trauma, and the mean time from injury to presentation was 4.7 years (range: 6 months–15 years) [
Statistical analysis
Data analysis was performed using the IBM SPSS 21. JOA scores were compared using a paired sample t-test. P < 0.05 was considered significant.
RESULTS
Surgery
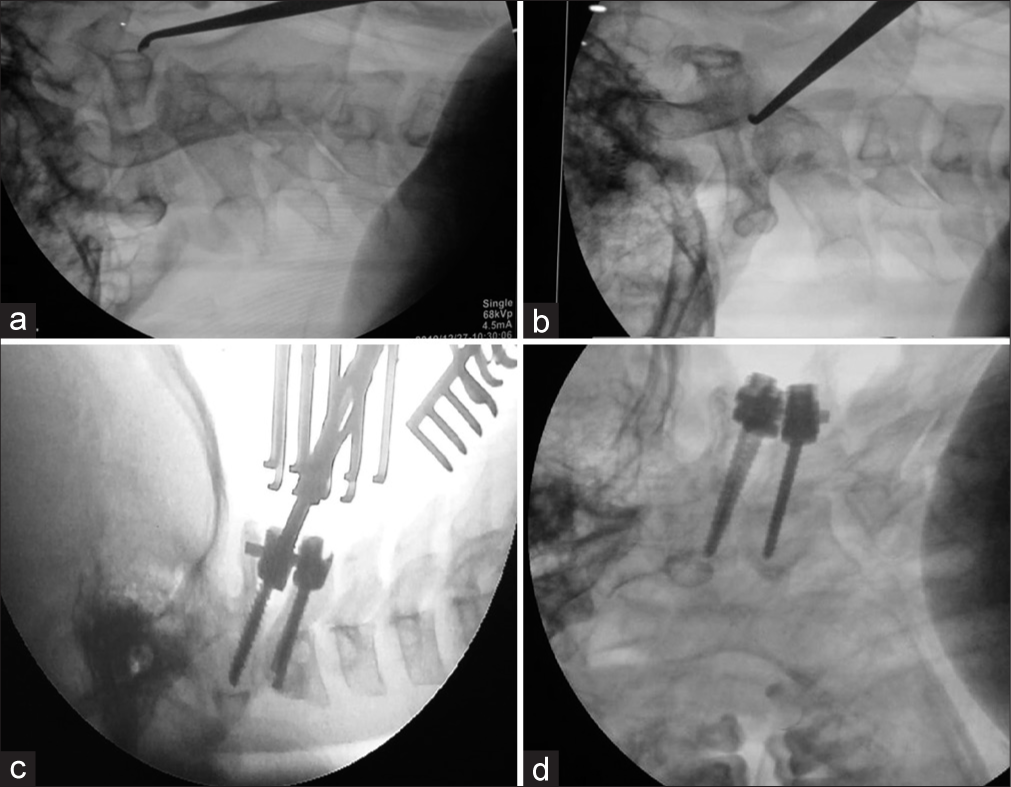
Eleven patients (2017–2021) underwent transcervical odontoid release followed by C1–C2 posterior fixation [
Figure 1:
(a) Intraoperative X-ray with patient in supine position. Anterior arch of atlas confirmed with lateral image. (b) Small curette inserted between C2 vertebral body and lower surface of fractured odontoid after release. The surfaces are being prepared for fusion. (c and d) Patient in prone position. C1 Lateral mass and C2 pedicle screws inserted.
Postoperative follow-up
At mean follow-up of 9.6 postoperatively months, CT scans showed good alignment and reduction [
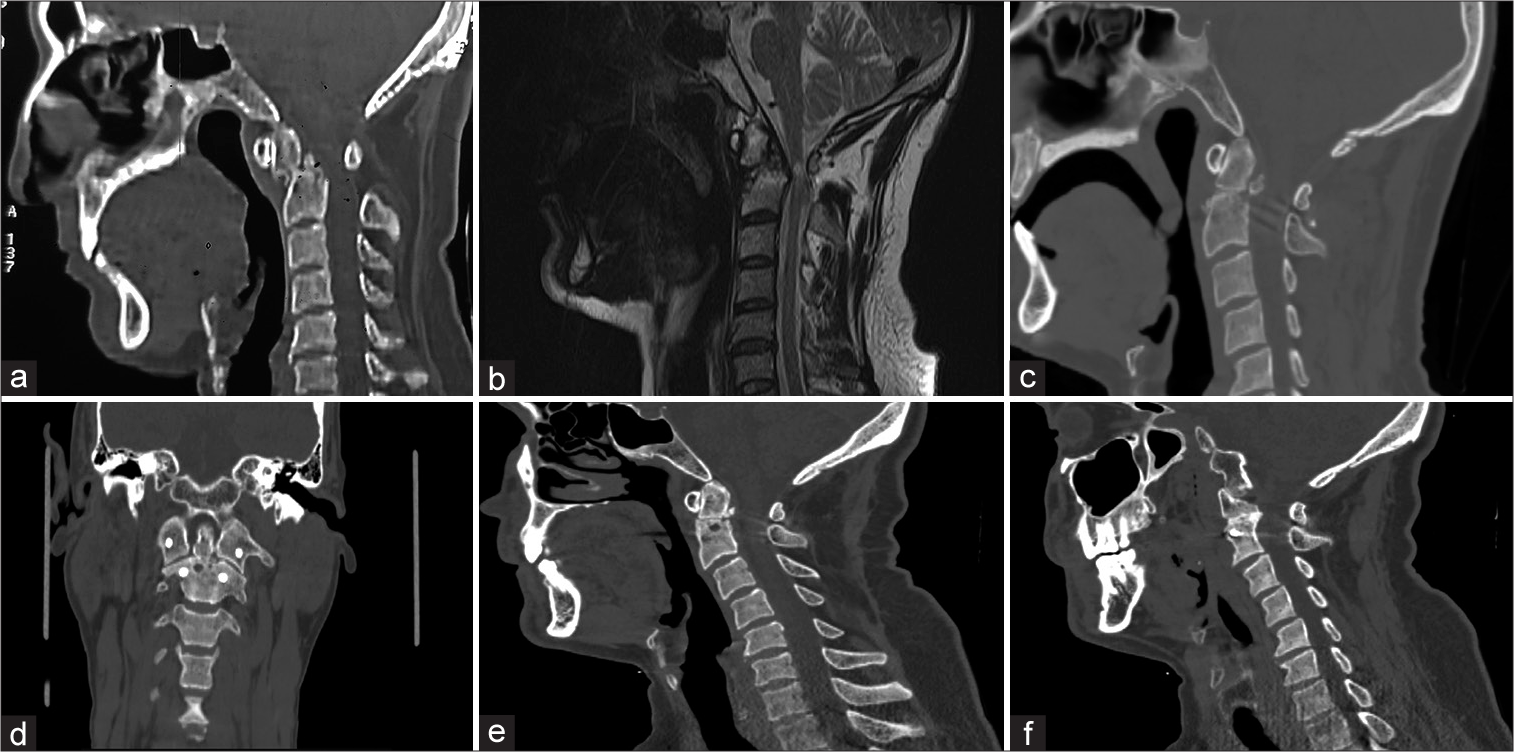
Figure 2:
A 60-year-old male with a history of bike accident 7 year ago presented on a wheel chair with a history of progressive weakness and numbness in all four limbs for the past 6 months. (a and b) Preoperative CT and MRI shows old type 2 odontoid fracture with anterolisthesis of C1/odontoid complex on C2 body and some bony fusion with significant cord compression and signal changes. (c and d) Sagittal and coronal CT scan taken in the immediate postoperative period showing alignment of the released odontoid. (e and f) Sagittal and parasagittal CT cuts taken at 1-year postoperative show that the alignment is maintained.
Figure 3:
A 56-year-old man presented with clumsy hands, difficulty micturition, and gait disturbance for the past 1 year. The patient had a history of motor vehicle accident with neck injury 15 years ago. (a) Extension lateral radiograph, (b) midsagittal CT scan shows old odontoid type 2 fracture fixed in anterolisthesis and resultant spinal canal narrowing, (c) immediate postoperative X-ray to confirm alignment and screw position and (d and e) coronal and sagittal CT scan taken at 6 months follow-up showing the alignment is maintained.
Figure 4:
A 37-year-old male with a history of neck pain and clicking, which started after a fall at a construction site 3 years ago presented with progressive upper and lower limb weakness and impaired bowel bladder function. (a and b) Sagittal, parasagittal preoperative views with fixed anterolisthesis of odontoid over C2 body and resultant canal narrowing. (c) Sagittal MRI shows extreme cord compression. (d and e) Flexion and extension radiographs show irreducibility atlantoaxial dislocation. (f) Intraoperative image of posterior C1–C2 fixation being done in the patient following release of odontoid. (g) Postoperative CT showing reduction of the displaced odontoid.
DISCUSSION
Type II odontoid fractures have a high rate of nonunion.[
Pros of retropharyngeal odontoid release
Several authors have reported on the utility of the retropharyngeal approach for the release of chronic angulated odontoid fractures. Hao et al. used an incision that was 2 cm below and parallel to the mandible for an anterior release.[
Need for accompanying posterior fusion
Following mobilization of the dens, the degenerated C1–C2 facet joints must be opened and released to achieve complete reduction of the AAD and instrumented fixation using a posterior approach. However, unlike patients with congenital AAD, posterior manipulation/fusion alone is usually ineffective in achieving the complete reduction of the malunited remote fractures. This is because the bony and fibrous adhesions between the odontoid and C2 body found intraoperatively, fixing the fractured dens in anterolisthesis, are not accessible using the posterior approach alone. These findings along with severe C1-2 facet joint degenerative changes justify the dual circumferential procedures, that is, release of both the anterior fixed odontoid malunion and the posterior C1-2 facet joint adhesions followed by posterior fusion.
CONCLUSION
Anterior release through a retropharyngeal approach coupled with posterior C1–C2 instrumentation proved to be an effective alternative to the traditional transoral approach to treat a chronic malunited odontoid fracture.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aggarwal RA, Rathod AK, Chaudhary KS. Irreducible atlanto-axial dislocation in neglected odontoid fracture treated with single stage anterior release and posterior instrumented fusion. Asian Spine J. 2016. 10: 349-54
2. Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine. 1997. 22: 1843-52
3. Hao DJ, He BR, Wu QN. One-stage anterior release and reduction with posterior fusion for treatment of irreducible atlantoaxial dislocation. Orthop Surg. 2009. 1: 305-10
4. Kirankumar MV, Behari S, Salunke P, Banerji D, Chhabra DK, Jain VK. Surgical management of remote, isolated type II odontoid fractures with atlantoaxial dislocation causing cervical compressive myelopathy. Neurosurgery. 2005. 56: 1004-12
5. Klimov V, Kosimshoev M, Evsyukov A, Stepanenko V, Rzaev J. Surgical treatment of neglected C2 odontoid process fracture with anterior atlantoaxial dislocation. Br J Neurosurg. 2020. 35: 1-5
6. Ren X, Gao F, Li S, Yang J, Xi Y. Treatment of irreducible atlantoaxial dislocation using one-stage retropharyngeal release and posterior reduction. J Orthop Surg (Hong Kong). 2019. 27: 1-5
7. Robinson Y, Robinson AL, Olerud C. Systematic review on surgical and nonsurgical treatment of type II odontoid fractures in the elderly. BioMed Res Int. 2014. 2014: 231948
8. Wang C, Yan M, Zhou HT, Wang SL, Dang GT. Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine. 2006. 31: E306-13
9. Wu YS, Chi YL, Wang XY, Xu HZ, Lin Y, Mao FM. Microendoscopic anterior approach for irreducible atlantoaxial dislocation: Surgical techniques and preliminary results. J Spinal Disord Tech. 2010. 23: 113-20
10. Yuan SL, Xu HM, Fu LC, Cao J, Yang JK, Xi YM. Sagittal atlantoaxial joint inclination and reduction index values for diagnosis and treatment of irreducible atlantoaxial dislocation. Indian J Orthop. 2018. 52: 190-5