- Department of Neurosurgery, Post Graduate Institute of Medical Education and Research, Chandigarh, India
- Department of Otolaryngology and Head Neck Surgery, Post Graduate Institute of Medical Education and Research, Chandigarh, India
- Department of Histopathology, Post Graduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Sandeep Mohindra
Department of Histopathology, Post Graduate Institute of Medical Education and Research, Chandigarh, India
DOI:10.4103/2152-7806.173562
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohindra S, Kapoor A, Kursa GK, Mohindra S, Saikia U. Apoplexy in an intradural clival chordoma causing intraventricular bleed. Surg Neurol Int 07-Jan-2016;7:
How to cite this URL: Mohindra S, Kapoor A, Kursa GK, Mohindra S, Saikia U. Apoplexy in an intradural clival chordoma causing intraventricular bleed. Surg Neurol Int 07-Jan-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/apoplexy-in-an-intradural-clival-chordoma-causing-intraventricular-bleed/
Abstract
Background:A few cases depicting apoplexy in a chordoma have been reported. Rarely, this intratumoral bleed may spillover into intracerebral or intraventricular regions.
Case Description:The authors report an intradural variety of clival chordoma presenting with apoplexy and spillover of blood into lateral ventricle. Clinical presentation, radiological scans, and relevant literature is also described.
Conclusions:In a stable case of clival chordoma, intratumoral bleed or apoplexy may cause rapid neurological worsening and warranting urgent surgical intervention.
Keywords: Apoplexy, chordoma, intraventricular bleed
INTRODUCTION
Originating from the remnant notochord, chordomas are usually located in extradural bony structures of the skull base. These arise from spheno-occipital synchondrosis and slowly erode surrounding structures depicting locally invasive nature and propensity for aggressive recurrences. Vascular event or apoplexy may be a rare presentation of such a skull base neoplasm.[
CASE DESCRIPTION
A 26-year-old male presented with complaints of diplopia for past 3 years and gradually progressive right-sided hemiparesis for 6 months duration. For the past 2 weeks, he was having a severe headache and worsening of sensorium. On examination, the patient was conscious but drowsy. He had left-sided 3rd and 6th cranial nerve palsies, and right-sided spastic hemiparesis. The patient was carrying magnetic resonance imaging (MRI) performed 6 months back, showing an extra-axial mass on the left side, arising from clivus [Figure
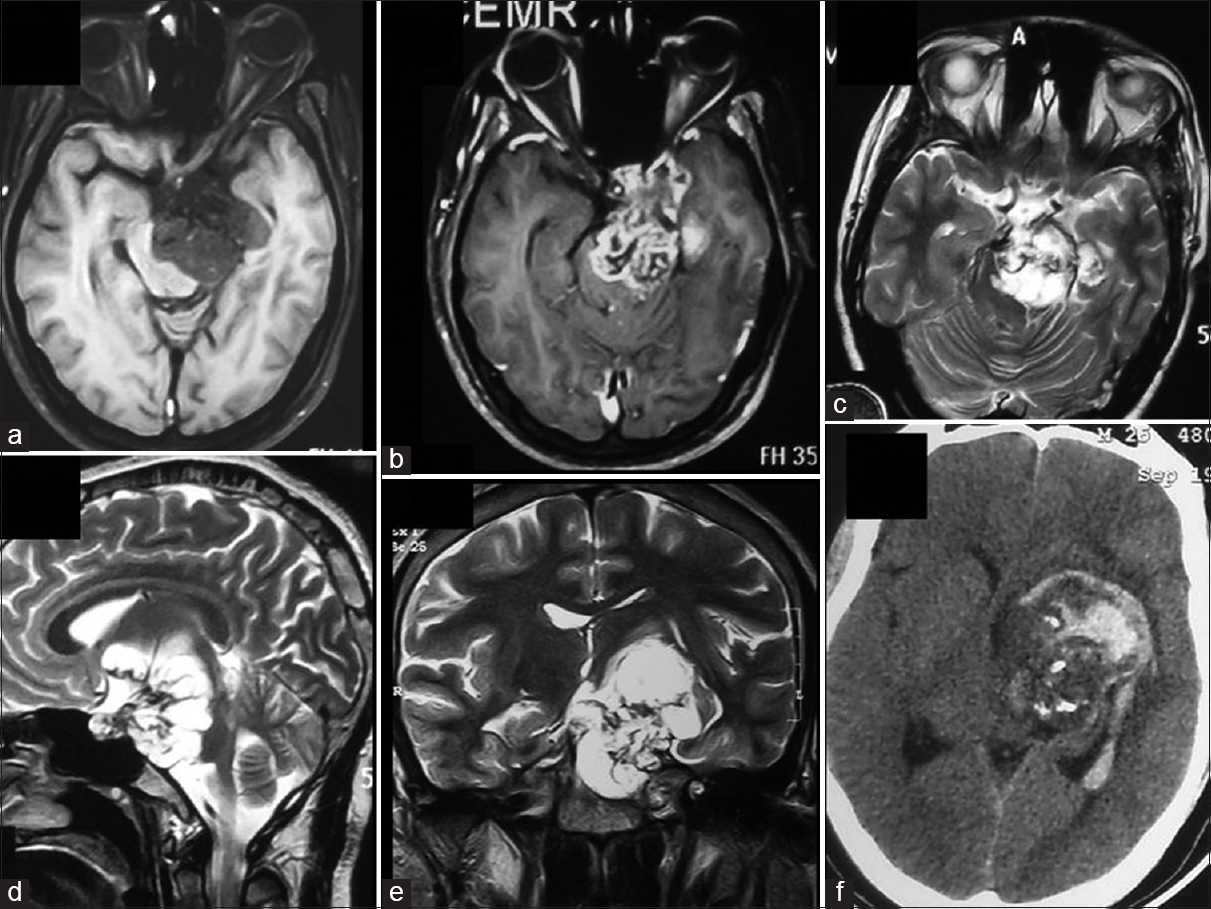
Figure 1
Magnetic resonance imaging scan, axial section of T1-weighted 1 (a), T1-weighted 1 with contrast (b) and T2-weighted 2 (c) showing an enhancing mass on the left side of clivus. Sagittal section of T2-weighted 1 (d) and coronal section of T2-weighted 1 (e) showing an extraosseous, intradural variety of chordoma, displacing pons and midbrain. Axial section, plain computed tomography scan (f) showing apoplectic chordoma with spillage of bleed into occipital horn of lateral ventricle
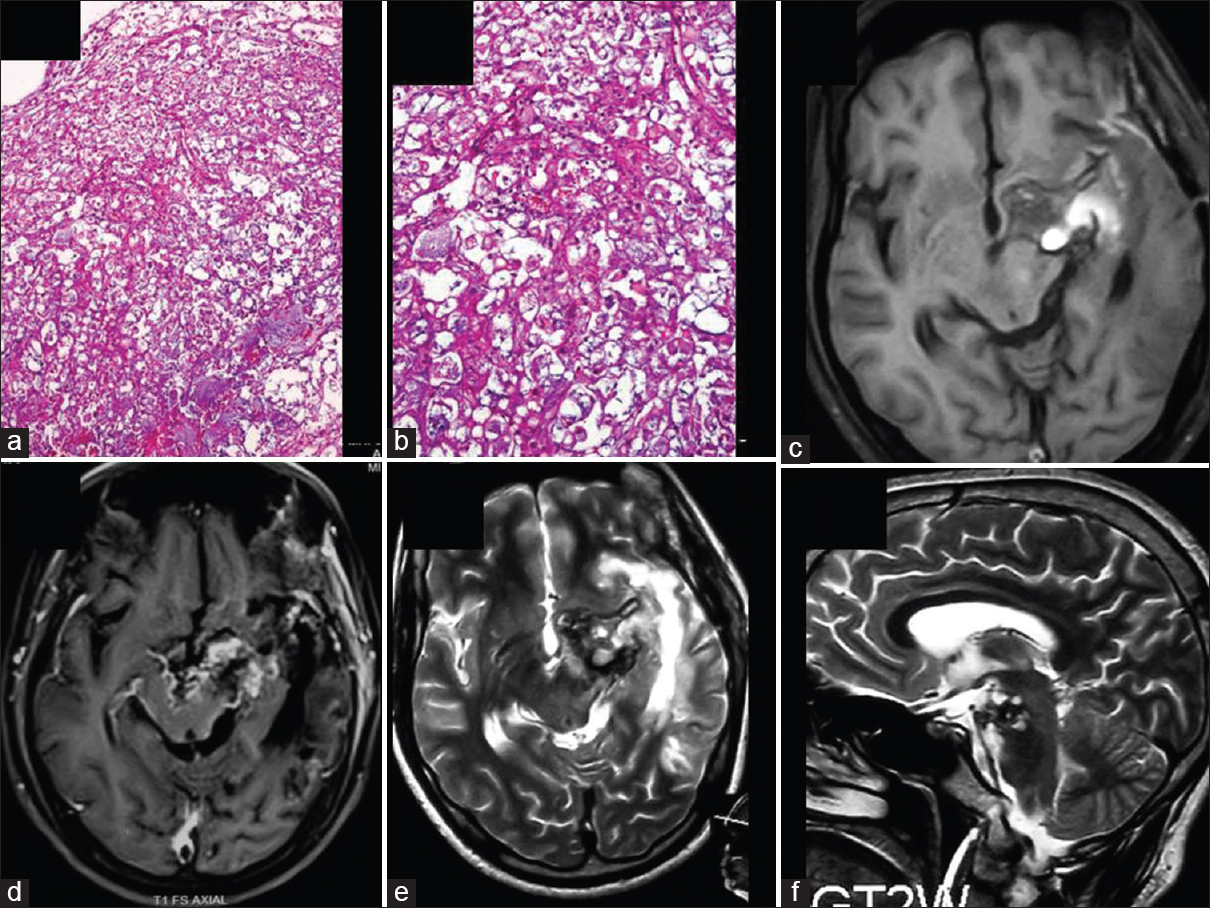
Figure 2
Histopathological photomicrograph (a) showing a cellular tumor arranged in chords and lobules in a myxoid stroma (H and E, ×200). (b) Tumor cells, large sized, having abundant, vacuolated cytoplasm indicating physaliphorous cell (H and E, ×400). Follow-up magnetic resonance imaging scan, axial section of T1-weighted 1 (c), T1-weighted 1 with contrast (d), axial section of T2-weighted 1 (e) and sagittal section of T2-weighted 1 (f) showing subtotal excision of tumor
DISCUSSION
Chordomas usually present with gradually progressive clinical symptoms as these lesions slowly spread centrifugally to involve multiple cranial nerve palsies at the skull base. Occasionally, such a gradual deterioration may be hastened by apoplexy, taking clinicians by a surprise. The apoplectic chordoma may present with intratumoral bleed, subarachnoid bleed, and even intraventricular bleed.[
CONCLUSIONS
Apoplexy in a chordoma is a rare phenomenon. Such an event may cause downward spiraling of the clinical status of an otherwise stable patient. The radiological scans, operative, and pathological findings support hemorrhagic infarction due to rapid tumor growth or rupture of the thin-walled vessels within the tumor.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Kim SK, Kim YH, Park CK, Kim MA, Park SH. Intracranial intradural chordoma presenting with intraventricular hemorrhage. Clin Neurol Neurosurg. 2012. 114: 1189-92
2. Koga N, Kadota Y, Hatashita S, Hosaka Y, Sugimura J, Sakakibara T. A case of clivus chordoma showing hemorrhage in the posterior fossa. No Shinkei Geka. 1988. 16: 1417-21
3. Lee HJ, Kalnin AJ, Holodny AI, Schulder M, Grigorian A, Sharer LR. Hemorrhagic chondroid chordoma mimicking pituitary apoplexy. Neuroradiology. 1998. 40: 720-3
4. Levi AD, Kucharczyk W, Lang AP, Schutz H. Clival chordoma presenting with acute brain stem hemorrhage. Can J Neurol Sci. 1991. 18: 515-8
5. Nakau R, Kamiyama H, Kazumata K, Andou M. Subarachnoid hemorrhage associated with clival chordoma – Case report. Neurol Med Chir (Tokyo). 2003. 43: 605-7
6. Simonsen J. Fatal subarachnoid haemorrhage originating in an intracranial chordoma. Acta Pathol Microbiol Scand. 1963. 59: 13-20
7. Uda T, Ohata K, Takami T, Hara M. An intradural skull base chordoma presenting with acute intratumoral hemorrhage. Neurol India. 2006. 54: 306-7