- Department of Surgery, Section of Neurosurgery, Aga Khan University Hospital, Karachi, Sindh, Pakistan
- Medical College, Aga Khan University Hospital, Karachi, Sindh, Pakistan
- Medical College, Peoples University of Medical and Health Sciences for Women, Karachi, Sindh, Pakistan
- Department of Diagnostic Radiology, Queen’s University, Kingston General Hospital, Kingston, Canada
- Department of Neurology, Massachusetts General Hospital, Boston, United States
- Hyperfine, Inc., Guilford, United States.
Correspondence Address:
Syed Ather Enam, Department of Surgery, Section of Neurosurgery, Aga Khan University Hospital, Karachi, Sindh, Pakistan.
DOI:10.25259/SNI_162_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Altaf1, Muhammad Shakir1, Hammad Atif Irshad2, Shiza Atif2, Usha Kumari3, Omar Islam4, W. Taylor Kimberly5, Edmond Knopp6, Chip Truwit6, Khan Siddiqui6, S. Ather Enam1. Applications, limitations and advancements of ultra-low-field magnetic resonance imaging: A scoping review. 28-Jun-2024;15:218
How to cite this URL: Ahmed Altaf1, Muhammad Shakir1, Hammad Atif Irshad2, Shiza Atif2, Usha Kumari3, Omar Islam4, W. Taylor Kimberly5, Edmond Knopp6, Chip Truwit6, Khan Siddiqui6, S. Ather Enam1. Applications, limitations and advancements of ultra-low-field magnetic resonance imaging: A scoping review. 28-Jun-2024;15:218. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12968
Abstract
Background: Ultra-low-field magnetic resonance imaging (ULF-MRI) has emerged as an alternative with several portable clinical applications. This review aims to comprehensively explore its applications, potential limitations, technological advancements, and expert recommendations.
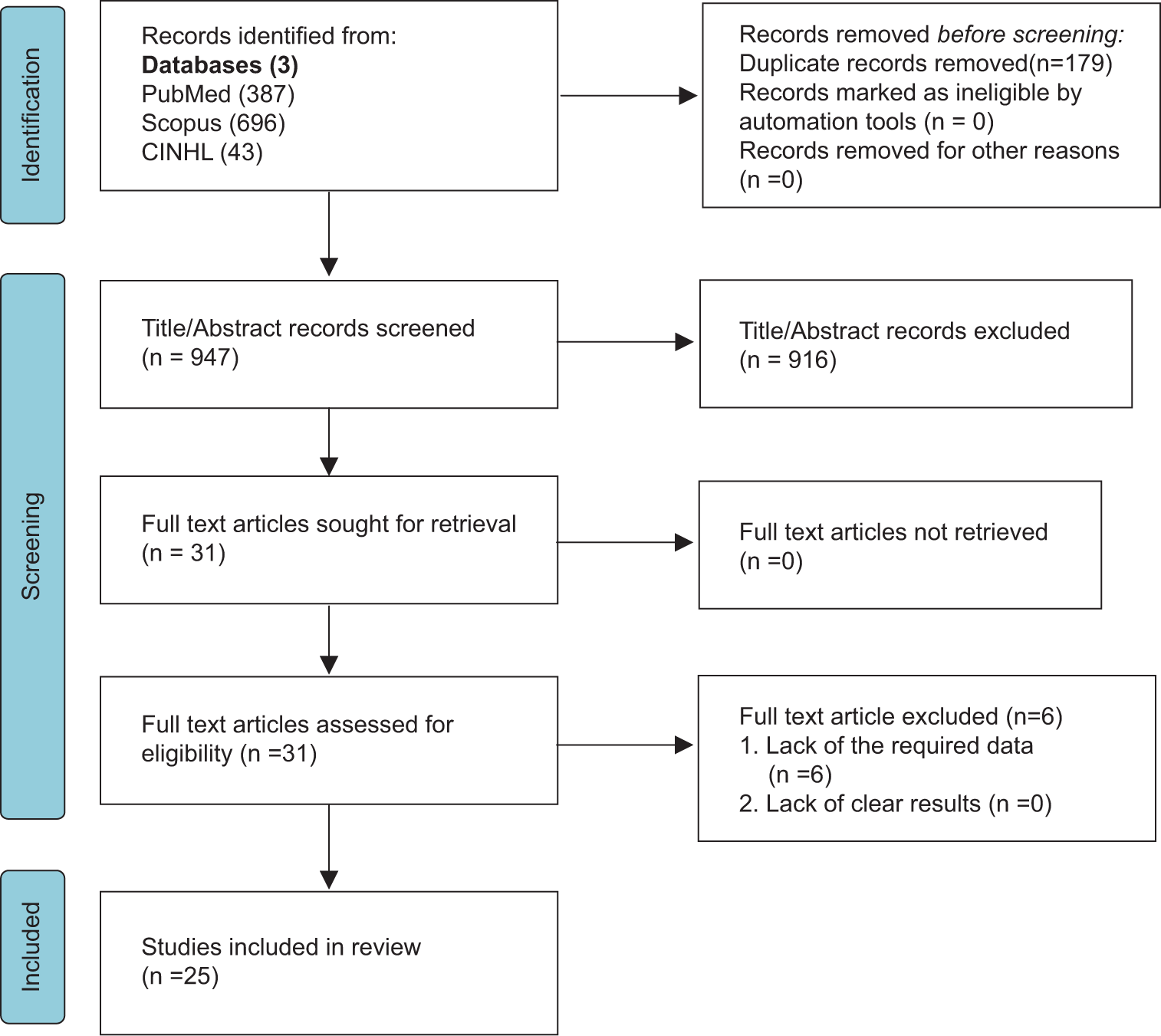
Methods: A review of the literature was conducted across medical databases to identify relevant studies. Articles on clinical usage of ULF-MRI were included, and data regarding applications, limitations, and advancements were extracted. A total of 25 articles were included for qualitative analysis.
Results: The review reveals ULF-MRI efficacy in intensive care settings and intraoperatively. Technological strides are evident through innovative reconstruction techniques and integration with machine learning approaches. Additional advantages include features such as portability, cost-effectiveness, reduced power requirements, and improved patient comfort. However, alongside these strengths, certain limitations of ULF-MRI were identified, including low signal-to-noise ratio, limited resolution and length of scanning sequences, as well as variety and absence of regulatory-approved contrast-enhanced imaging. Recommendations from experts emphasize optimizing imaging quality, including addressing signal-to-noise ratio (SNR) and resolution, decreasing the length of scan time, and expanding point-of-care magnetic resonance imaging availability.
Conclusion: This review summarizes the potential of ULF-MRI. The technology’s adaptability in intensive care unit settings and its diverse clinical and surgical applications, while accounting for SNR and resolution limitations, highlight its significance, especially in resource-limited settings. Technological advancements, alongside expert recommendations, pave the way for refining and expanding ULF-MRI’s utility. However, adequate training is crucial for widespread utilization.
Keywords: Global health, Healthcare innovation, Medical imaging, Technology, Ultra-low-field magnetic resonance imaging
INTRODUCTION
The development of low-cost magnetic resonance imaging (MRI) technologies at ultra-low-field (ULF) strengths, that is, <0.1 T, has received attention recently.[
Across the globe, the accessibility and availability of imaging technologies paint a diverse landscape, starkly contrasting between well-resourced nations and those striving to overcome developmental hurdles.[
At the heart of this imaging mosaic lies MRI, a stalwart in medical diagnostics, which largely replaced CT mainly due to its enhanced sensitivity, lack of radiation exposure, and superior soft-tissue contrast, facilitating the detection of varied pathologies, including small infarcts.[
As technology advances, so does the pursuit for more refined and accessible diagnostic tools. This quest gave birth to ULF MRI, an innovative approach that resonates with the core principles of imaging while carving a unique niche in the medical landscape. Despite improving accessibility to magnetic resonance, ULF strengths are still progressing toward sufficient imaging quality for clinical applications.[
The potential benefits of ULF-MRI include its footprint, affordability, and ease of transportation to the patient’s location. In contrast, conventional MRI offers its own merits, such as the ability to perform contrast examinations and a low signal-to-noise ratio (SNR), but it has limitations, such as its large size, high cost, and the requirement for patients to remain immobile in a confined space, which can cause discomfort or even claustrophobia for some patients.[
ULF-MRI, with its potential to address some of the limitations of traditional MRIs, has garnered attention for its possible role in revolutionizing diagnostic imaging. As with any pioneering technology, the literature surrounding ULFMRI is still in its nascent stages. However, a comprehensive assessment of its advantages and limitations has not been conducted for clinicians. Therefore, this scoping review aims to explore existing evidence and identify knowledge gaps for ULF-MRI to provide a singular source with the latest information. A noticeable gap exists in comprehensively understanding its full potential, applications, and comparative efficacy in various clinical scenarios. Bridging this gap is crucial to harnessing the full capabilities of ULFMRI and translating them into tangible improvements in patient care, which is one of the objectives of this review.
MATERIALS AND METHODS
Operational definitions
The definition of “low-field” is not consistent; it is sometimes used for values below 1.5T and other times confined to the range of 0.01T–0.1T.[
ULF: ≤0.1T Low field (LF): ≤0.1T and ≤0.3T High field (HF): >1.0T and ≤3T Ultra-HF: ≥7T
This review has been designed to overview existing evidence, identify gaps in knowledge, and pave the way for future research. Our review adhered to the guidelines laid out by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRIMA-ScR).[
Search strategy
A comprehensive and systematic literature search was performed using multiple databases, including PubMed, CINAHL, and Scopus, from inception to May 31, 2023. The search included the Medical Subject Headings database and utilized the following keywords: “Ultra-Low Field MRI,” “Portable MRI,” or “Hyperfine MRI.” Searches were limited to abstract, title, and keywords. Backward reference searches (examining references of found articles) and reference snowballing (using citations to identify additional papers) were also performed to obtain the maximum number of articles. There was no restriction on language or date to ensure that the most current and relevant data were included in the study. The search also included ResearchGate and Google Scholar and recognized repositories of Gray Literature to capture unpublished studies on this topic.
Study selection
This review considered cross-sectional and cohort studies, both randomized and nonrandomized trials, case series, case reports, and technical reports that discussed ULF-MRI. We excluded review articles, editorials, letters to the editor, meeting abstracts, book chapters, guidelines, animal studies, and studies lacking full text. Search results were imported into Mendeley to remove duplicates, and two reviewers (AA and MS) independently screened titles and abstracts based on the inclusion criteria. A third reviewer was consulted (HAI) to discuss disagreements. After title and abstract screening, the full text was screened independently, with conflicts resolved by discussion with a third reviewer (HAI).
Data extraction
For each study that met the inclusion criteria, relevant data were extracted, including study design, sample size, study setting, applications, limitations, recommendations, and adverse events related to ULF-MRI. Two reviewers (SA and UK) independently extracted per the column headings using a predefined sheet. Any disagreements on the placement of information in the headings between the reviewers were resolved by consulting an additional reviewer (HAI). Missing data were systematically handled; studies with incomplete data were still included, and attempts were made to contact authors for clarification. However, the analysis relied on available data, with any implications of missing data acknowledged within review limitations.
Data analysis
The analysis in this review was conducted through a systematic approach. Extracted data from selected studies were collated and synthesized to identify patterns, themes, and key findings. A qualitative content analysis was used to categorize and group information, allowing for an overview of the landscape while highlighting trends, gaps, and insights related to ULF-MRI applications, limitations, and recommendations across the studies.
RESULTS
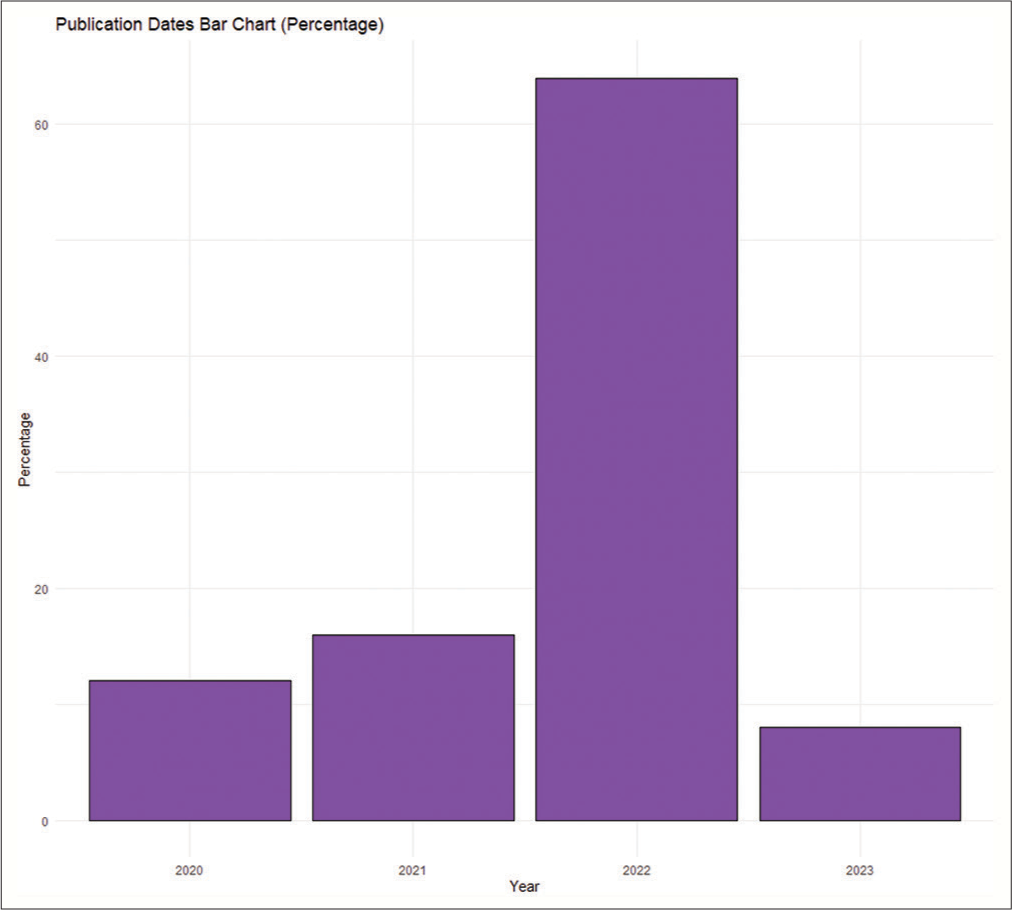
A total of 25 articles were included after the title, abstract, and full-text screening. The flow diagram for article screening and selection is depicted in
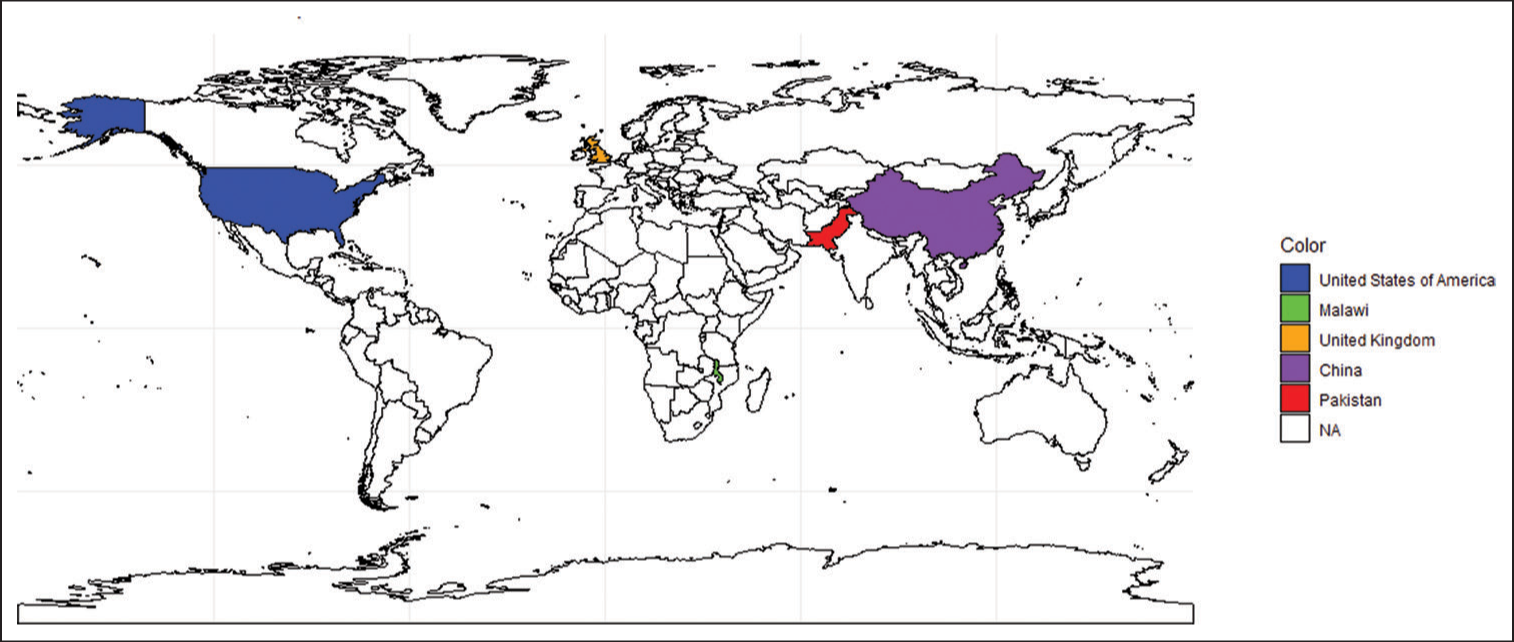
The analysis of the included studies revealed several distinct themes showcasing diverse applications of ULF-MRI in the field of medical imaging. First, ULF-MRI proves to be an effective tool in intensive care units (ICUs). It is particularly useful for patients who exhibit neurological alterations, experience seizures, have unexplained encephalopathy, or show abnormal head CT scans.[
Some of the studies have identified and highlighted inherent limitations of ULF-MRI technology. These limitations encompass various aspects of the technology’s functionality. These include challenges such as a low SNR,[
A notable theme surfaces through valuable recommendations by experts to improve ULF-MRI functionality. Stemming from comprehensive analysis, these tailored recommendations address identified limitations, driving advancements in ULF-MRI. Improvements encompass imaging acquisition and quality, introducing novel sequences, and AI-driven improvements.[
DISCUSSION
This review discusses the applications, limitations, technological advancements, and recommendations associated with ULF-MRI. The findings underscore the substantial impact of ULF-MRI in various clinical settings, such as pediatrics and adult ICU, particularly to challenges posed by the COVID-19 pandemic and even resource-constrained settings. Notably, ULF-MRI showcased its proficiency in improving bedside scanning experiences and offering diverse clinical applications spanning epilepsy, MS, and ischemic stroke. Technological progress is evident through innovative reconstruction methods and integration with machine learning techniques. In addition, the review identified vital recommendations for further refining and expanding the potential of ULF-MRI.
Among applications, portable imaging technologies offer a range of benefits in ICU settings that traditional MRIs do not. For example, ULF MRI enables more frequent monitoring, facilitating real-time observation of changes and the adjustment of treatment plans.[
ULF MRI’s adaptability facilitates its smooth integration into a range of ICU settings, ensuring patient-centric care. The minimization of disturbances is noteworthy, as portable imaging helps in developing settings that are conducive to patients’ recovery.[
Early detection and diagnosis are improved through these technologies, enabling quick interventions and, hence, better patient outcomes.[
Figure 5:
The Swoop® Portable Magnetic Resonance Imaging (MRI) System™ (Hyperfine, Inc., Guilford, CT, USA). This illustration showcases the practical utilization of the Hyperfine Swoop, a portable MRI scanner with low magnetic field strength, within a clinical context. The system’s mobility allows it to be transported to a patient’s bedside, where it can be connected to a standard wall outlet for power. The operation of the scanner is managed through a wireless tablet. The system boasts a field strength of 0.064T, employs a permanent magnet, and carries a weight of approximately 1400 pounds. On the Left: Connected to a power outlet and used through a wireless tablet. On the Right (Top and Bottom): Use of the system in a practical setting.
Traditional MRI machines require specialized facilities, trained technicians, and high maintenance costs.[
Portable neuroimaging devices often have lower maintenance requirements and can be operated with simpler infrastructure with no need to be kept in protected rooms due to their lower magnetic field strength.[
Portable neuroimaging devices typically consume less power compared to their traditional counterparts.[
ULF-MRI operates at significantly lower magnetic field strengths compared to traditional HF MRI machines.[
In addition, it is crucial to discuss the limitations of ULFMRI. The limitations largely arise from the imaging performance of this modality. Low spatial resolution, a high degree of noise and artifacts in the images, and a lengthy scan time (particularly when various orientations of the images are required) are examples of these shortcomings. SNR, which is used for the assessment of noise and signal quality by comparing the actual image data (signal) to the background noise in the system, uses weak magnetic fields of <1T to produce less SNR, resulting in compromised imaging resolution.[
Nevertheless, a significant watershed moment in ULFMRI systems arose from the incorporation of artificial intelligence (AI) and deep learning in image reconstruction. The implementation of SNR-efficient data acquisition and reconstruction algorithms, including parallel imaging, compressed sensing, and machine learning-based image reconstruction methods, have allowed ULF-MRI to be clinically useful.[
Proponents argue that ULF-MRI expands access with simpler, low-cost systems in underserved regions. However, meaningful access mandates reliable diagnosis. A case report regarding a suspected stroke MRI conducted on the same day in the same patient using both 3T and 0.064T stated that even though the patient’s movement caused low-quality scanned images and lacked diagnostic precision needed, the results were still reliable and concordant with that of HF 3T MRI scanner.[
Machine learning has shown promise for improving ULFMRI technology. Be it in the form of image reconstruction, artifact minimization, contrast enhancement, or predictive modeling. One group developed an active electromagnetic interference cancellation system using analytical and deep learning models that eliminated the need for traditional RF shielding in a low-cost 0.55T ULF-MRI system.[
Recommendations
Further work is needed to incorporate ULF MRIs in a larger variety of clinical settings and to improve the diagnostic capability of these devices. Although ULF-MRI offers several advantages over traditional MRI scanners, such as lower cost, reduced power requirements, and improved patient comfort, the findings of this review suggest several important areas for future investigation based on the current limitations identified. First, it is recommended that future researchers focus on longitudinal studies to understand better the long-term feasibility and safety effects associated with the use of ULF-MRI. In addition, the studies that have been performed previously were mainly cross-sectional, cohort study designs, and case reports. There is a need for more randomized controlled trials to establish causality and determine the effectiveness of the new technology in a wide variety of use cases – some of which would not be possible with an HF MRI scanner. Furthermore, researchers are encouraged to explore diverse populations and settings and, therefore, enhance the generalizability of findings. It is also advised to employ rigorous research designs, utilize standardized measurement tools, and employ robust statistical analyses to increase the validity and reliability of research outcomes. These recommendations may serve as a guide for future researchers, enabling them to build on the existing knowledge base and contribute to the advancement of ULF MRIs.
Limitations
Limitations of this scoping review include variations in the study methodologies of the included studies, potential biases from selected literature, and the qualitative nature of the data synthesis. Moreover, despite the steps taken, the data synthesis is subjective and restricted to predefined headings. In addition, the sample sizes of included studies were generally small (<100), and therefore, the use of larger cohorts in the future is crucial for increased generalizability. Potential confounders, such as the status of the patients and their comorbidities within each study, were also not considered. These factors, while considered, could impact the depth and scope of the findings presented.
CONCLUSION
This review has unveiled the remarkable potential of ULF MRI across a spectrum of clinical applications. The findings underscore its significant role in enhancing patient experiences in ICU settings, its diverse clinical utility spanning various medical and surgical conditions, and its integration with innovative reconstruction methods and machine learning techniques. ULF-MRI can be particularly useful in resource-limited settings to bridge the gap in diagnostic modalities. Future work should address its limitations in imaging quality and further facilitate its clinical adoption.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
Edmond Knopp is the Vice President of Medical Affairs at Hyperfine Inc. Chip Truwit is the Vice President of Scientific Affairs at Hyperfine Inc. Khan Siddiqui is the Chief Medical Officer at Hyperfine Inc.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Altaf A, Baqai MW, Urooj F, Alam MS, Aziz HF, Mubarak F. Intraoperative use of ultra-low-field, portable magnetic resonance imaging-first report. Surg Neurol Int. 2023. 14: 212
2. Altaf A, Baqai MW, Urooj F, Alam MS, Aziz HF, Mubarak F. Utilization of an ultra-low-field, portable magnetic resonance imaging for brain tumor assessment in lower middle-income countries. Surg Neurol Int. 2023. 14: 260
3. Arnold TC, Baldassano SN, Litt B, Stein JM. Simulated diagnostic performance of low-field MRI: Harnessing open-access datasets to evaluate novel devices. Magn Reson Imaging. 2022. 87: 67-76
4. Arnold TC, Freeman CW, Litt B, Stein JM. Low-field MRI: Clinical promise and challenges. J Magn Reson Imaging. 2023. 57: 25-44
5. Arnold TC, Tu D, Okar SV, Nair G, By S, Kawatra KD. Sensitivity of portable low-field magnetic resonance imaging for multiple sclerosis lesions. Neuroimage Clin. 2022. 35: 103101
6. Beekman R, Crawford A, Mazurek MH, Prabhat AM, Chavva IR, Parasuram N. Bedside monitoring of hypoxic ischemic brain injury using low-field, portable brain magnetic resonance imaging after cardiac arrest. Resuscitation. 2022. 176: 150-8
7. Chetcuti K, Chilingulo C, Goyal MS, Vidal L, O’Brien NF, Postels DG. Implementation of a low-field portable MRI scanner in a resource-constrained environment: Our experience in Malawi. AJNR Am J Neuroradiol. 2022. 43: 670-4
8. Cho SM, Wilcox C, Keller S, Acton M, Rando H, Etchill E. Assessing the SAfety and FEasibility of bedside portable low-field brain magnetic resonance imaging in patients on ECMO (SAFE-MRI ECMO study): Study protocol and first case series experience. Crit Care. 2022. 26: 119
9. DeBenedectis CM, Spalluto LB, Americo L, Bishop C, Mian A, Sarkany D. Health care disparities in radiology-a review of the current literature. J Am Coll Radiol. 2022. 19: 101-11
10. Deoni SC, Bruchhage MM, Beauchemin J, Volpe A, D’Sa V, Huentelman M. Accessible pediatric neuroimaging using a low field strength MRI scanner. Neuroimage. 2021. 238: 118273
11. Deoni SC, Burton P, Beauchemin J, Cano-Lorente R, De Both MD, Johnson M. Neuroimaging and verbal memory assessment in healthy aging adults using a portable low-field MRI scanner and a web-based platform: Results from a proof-of-concept population-based cross-section study. Brain Struct Funct. 2023. 228: 493-509
12. Deoni SC, Medeiros P, Deoni AT, Burton P, Beauchemin J, D’Sa V. Development of a mobile low-field MRI scanner. Sci Rep. 2022. 12: 5690
13. Deoni SC, O’Muircheartaigh J, Ljungberg E, Huentelman M, Williams SC. Simultaneous high-resolution T(2)-weighted imaging and quantitative T(2) mapping at low magnetic field strengths using a multiple TE and multi-orientation acquisition approach. Magn Reson Med. 2022. 88: 1273-81
14. Desroche CN, Johnson AP, Hore EB, Innes E, Silver I, Tampieri D. Feasibility and cost analysis of portable MRI implementation in a remote setting in Canada. Can J Neurol Sci. 2023. p. 1-10
15. Geethanath S, Vaughan JT. Accessible magnetic resonance imaging: A review. J Magn Reson Imaging. 2019. 49: e65-77
16. Global atlas of medical devices. Available from: https://apps.who.int/iris/handle/10665/255181 [Last accessed on 2023 Sep 14].
17. Guo Q, Ma C, Zhang X, Xu Y, Fan M, Yu P. SQUID-based magnetic resonance imaging at ultra-low field using the backprojection method. Concepts Magn Reson B Magn Reson Eng. 2020. 2020: 1-11
18. Heales CJ, Lloyd E. Play simulation for children in magnetic resonance imaging. J Med Imaging Radiat Sci. 2022. 53: 10-6
19. Hinrichs-Krapels S, Tombo L, Boulding H, Majonga ED, Cummins C, Manaseki-Holland S. Barriers and facilitators for the provision of radiology services in Zimbabwe: A qualitative study based on staff experiences and observations. PLoS Glob Public Health. 2023. 3: e0001796
20. Hovis G, Langdorf M, Dang E, Chow D. MRI at the bedside: A case report comparing fixed and portable magnetic resonance imaging for suspected stroke. Cureus. 2021. 13: e16904
21. Hricak H, Abdel-Wahab M, Atun R, Lette MM, Paez D, Brink JA. Medical imaging and nuclear medicine: A Lancet oncology commission. Lancet Oncol. 2021. 22: e136-72
22. Human health campus - database and statistics. Available from: https://humanhealth.iaea.org/HHW/DBStatistics/IMAGINEMaps3.html [Last accessed on 2023 Sep 14].
23. Iglesias JE, Schleicher R, Laguna S, Billot B, Schaefer P, McKaig B. Quantitative brain morphometry of portable low-field-strength MRI using super-resolution machine learning. Radiology. 2023. 306:
24. Islam O, Lin AW, Bharatha A. Potential application of ultra-low field portable MRI in the ICU to improve CT and MRI access in Canadian hospitals: A multi-center retrospective analysis. Front Neurol. 2023. 14: 1220091
25. Iwan E, Yang J, Enders J, Napp AE, Rief M, Dewey M. Patient preferences for development in MRI scanner design: A survey of claustrophobic patients in a randomized study. Eur Radiol. 2021. 31: 1325-35
26. Koonjoo N, Zhu B, Bagnall GC, Bhutto D, Rosen MS. Boosting the signal-to-noise of low-field MRI with deep learning image reconstruction. Sci Rep. 2021. 11: 8248
27. Kuoy E, Glavis-Bloom J, Hovis G, Yep B, Biswas A, Masudathaya LA. Point-of-care brain MRI: Preliminary results from a single-center retrospective study. Radiology. 2022. 305: 666-71
28. Lau V, Xiao L, Zhao Y, Su S, Ding Y, Man C. Pushing the limits of low-cost ultra-low-field MRI by dual-acquisition deep learning 3D superresolution. Magn Reson Med. 2023. 90: 400-16
29. Liu Y, Leong AT, Zhao Y, Xiao L, Mak HK, Tsang AC. A low-cost and shielding-free ultra-low-field brain MRI scanner. Nat Commun. 2021. 12: 7238
30. Mazurek MH, Cahn BA, Yuen MM, Prabhat AM, Chavva IR, Shah JT. Portable, bedside, low-field magnetic resonance imaging for evaluation of intracerebral hemorrhage. Nat Commun. 2021. 12: 5119
31. McLean B, Thompson D. MRI and the critical care patient: Clinical, operational, and financial challenges. Crit Care Res Pract. 2023. 2023: 2772181
32. Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018. 18: 143
33. Nikpanah M, Willoughby WR, Campbell-Washburn AE, Denney TS, Malayeri AA, ver Hoef L. Low versus ultra-high field MRI: How to select your MRI fleet. Appl Radiol. 2023. 52: 28-41
34. Padormo F, Cawley P, Dillon L, Hughes E, Almalbis J, Robinson J. In vivo T1 mapping of neonatal brain tissue at 64 mT. Magn Reson Med. 2023. 89: 1016-25
35. Parag P, Hardcastle TC. Shortage of radiologists in low to middle-income countries in the interpretation of CT scans in trauma. Bangladesh J Med Sci. 2022. 21: 489-91
36. Prabhat AM, Crawford AL, Mazurek MH, Yuen MW, Chavva IR, Ward A. Methodology for low-field, portable magnetic resonance neuroimaging at the bedside. Front Neurol. 2021. 12: 760321
37. Runge SB, Christensen NL, Jensen K, Jensen IE. Children-centered care: Minimizing the need for anesthesia with a multi-faceted concept for MRI in children aged 4–6. Eur J Radiol. 2018. 107: 183-7
38. Sarracanie M, Salameh N. Low-field MRI: How low can we go? A fresh view on an old debate. Front Phys. 2020. 8: 172
39. Schellinger PD, Bryan RN, Caplan LR, Detre JA, Edelman RR, Jaigobin C. Evidence-based guideline: The role of diffusion and perfusion MRI for the diagnosis of acute ischemic stroke: Report of the therapeutics and technology assessment subcommittee of the American academy of neurology. Neurology. 2010. 75: 177-85
40. Shen FX, Wolf SM, Bhavnani S, Deoni S, Elison JT, Fair D. Emerging ethical issues raised by highly portable MRI research in remote and resource-limited international settings. Neuroimage. 2021. 238: 118210
41. Sheth KN, Mazurek MH, Yuen MM, Cahn BA, Shah JT, Ward A. Assessment of brain injury using portable, low-field magnetic resonance imaging at the Bedside of critically ill patients. JAMA Neurol. 2020. 78: 41-7
42. Sheth KN, Yuen MM, Mazurek MH, Cahn BA, Prabhat AM, Salehi S. Bedside detection of intracranial midline shift using portable magnetic resonance imaging. Sci Rep. 2022. 12: 1-11
43. Sien ME, Robinson AL, Hu HH, Nitkin CR, Hall AS, Files MG. Feasibility of and experience using a portable MRI scanner in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2023. 108: 45
44. Trotman-Dickenson B. Radiology in the intensive care unit (Part I). J Intensive Care Med. 2003. 18: 198-210
45. Turpin J, Unadkat P, Thomas J, Kleiner N, Khazanehdari S, Wanchoo S. Portable magnetic resonance imaging for ICU patients. Crit Care Explor. 2020. 2: e0306
46. Webb A, O’Reilly T. Tackling SNR at low-field: A review of hardware approaches for point-of-care systems. MAGMA. 2023. 36: 375-93
47. Wilcox C, Acton M, Rando H, Keller S, Sair HI, Chinedozi I. Safety of bedside portable low-field brain MRI in ECMO patients supported on intra-aortic balloon pump. Diagnostics (Basel). 2022. 12: 2871
48. Yuen MM, Prabhat AM, Mazurek MH, Chavva IR, Crawford A, Cahn BA. Portable, low-field magnetic resonance imaging enables highly accessible and dynamic bedside evaluation of ischemic stroke. Sci Adv. 2022. 8: eabm3952
49. Zhou B, Schlemper J, Dey N, Salehi SS, Sheth K, Liu C. Dual-domain self-supervised learning for accelerated non-Cartesian MRI reconstruction. Med Image Anal. 2022. 81: 102538