- Department of Neurosurgery, Centro Hospitalar Universitário Lisboa Norte EPE, Avenida Professor Egas Moniz,
- Department of Neurosurgery, CUF Infante Santo Hospital, Travessa do Castro, Lisbon, Portugal.
Correspondence Address:
Nuno Cubas Farinha
Department of Neurosurgery, Centro Hospitalar Universitário Lisboa Norte EPE, Avenida Professor Egas Moniz,
DOI:10.25259/SNI_651_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nuno Cubas Farinha1, Joaquim Cruz Teixeira2, José Hipólito Reis1, Domingos Coiteiro1. Arteriovenous fistula of the filum terminale masqueraded as a failed back surgery syndrome – A case report and review of literature. 10-Feb-2021;12:53
How to cite this URL: Nuno Cubas Farinha1, Joaquim Cruz Teixeira2, José Hipólito Reis1, Domingos Coiteiro1. Arteriovenous fistula of the filum terminale masqueraded as a failed back surgery syndrome – A case report and review of literature. 10-Feb-2021;12:53. Available from: https://surgicalneurologyint.com/surgicalint-articles/10575/
Abstract
Background: The filum terminale arteriovenous fistulas (FTAVFs) are a very rare type of spinal vascular malformation. Clinically, these lesions could present with a progressive ascending myelopathy also called FoixAlajouanine syndrome. Due to the rarity of these vascular malformation, some can be misdiagnosed, submitted to unnecessary spinal surgery, and even masqueraded as a failed back surgery syndrome. Based on the present case and related literature, we review all the cases with similar history and describe factors that should raise awareness for diagnosis of this spinal vascular malformation.
Case Description: We present a case of a patient with a FTAVF at the level of L5-S1 that presented with a FoixAlajouanine syndrome. He had been previously submitted to a lumbar decompressive laminectomy without sustained improvement. After the identification and surgical treatment of the vascular malformation, he had progressive neurological improvement.
Conclusion: FTAVF is a very rare spinal intradural spinal vascular malformation that can be masqueraded as a failed back surgery syndrome. In these cases, signs of ascending myelopathy should prompt awareness and vascular voids must be carefully evaluated in MRI.
Keywords: Failed back surgery syndrome, Filum terminale, Microsurgery, Myelopathy, Spinal arteriovenous fistula
INTRODUCTION
The filum terminale arteriovenous fistulas (FTAVFs) are a very rare type of spinal vascular malformation accounting for approximately 3% of cases.[
We describe a case of a patient with a FTAVF presented with a Foix-Alajouanine syndrome that had been previously misdiagnosed and had undergone a lumbar laminectomy for lumbar stenosis. We review all the FTAVF with similar history described in the literature. This literature search was performed on PubMed using the key words “arteriovenous fistula of the filum terminale,” “FTAVF,” “previous surgery,” “lumbosacral surgery,” and “failed back surgery syndrome.” We also describe factors that should raise awareness for diagnosis of this spinal vascular malformation.
CASE DESCRIPTION
A 73-year-old man was evaluated at the neurosurgical outpatient clinic with an 18-month history of intermittent back pain and progressive gait disturbance due to diminished strength in both legs. Seven years before, the patient had similar neurogenic claudication as main symptom and a lumbar CT scan was done solely, which showed stenosis at the L4-L5 level as the key feature. He underwent lumbar decompressive laminectomy in another institution, with transient improvement at that time.
During the following months, the symptoms slowly progressed and the patient became unable to walk without assistance. He also developed urinary sphincter disturbance with incontinence episodes. The neurological examination showed a bilateral lower extremity motor weakness with a motor strength grade 3/5 bilateral in hip flexion and extension, and a Grade 4/5 bilateral in knee extension, ankle dorsiflexion, knee flexion, great toe extension, and ankle plantar flexion. The patient also had hypoesthesia from L4 dermatome downward bilaterally, abnormally increased patellar and ankle reflexes bilaterally, and extensor plantar reflexes.
A lumbar MRI was performed, demonstrating prominent vascular voids near conus medullaris but no significant high T2 signal involving the spinal cord [
Figure 1:
Preoperative images: (a) MRI T2 sagittal showing multiple vascular voids near conus medullaris (arrow). (b) MRI T2 axial revealing two hypointense structures on the left (arrow) that were confirmed to be the arterial feeder and draining vein of the filum terminale arteriovenous fistula (FTAVF) after the DSA. (c) CT angiogram showing the contrast enhancement of the FTAVF (arrow) and multiple vascular voids around the conus medullaris and lower spinal cord (arrow head). (d) Dorsolumbar DSA showing the FTAVF at L5-S1 (arrow) with a descending arterial feeder from left D10 and an ascending draining vein.
Therapeutic options were discussed with the patient, who decided to undergo surgery. Reopening and extension of the previous laminectomy down to S1 was performed, to expose the fistula. After durotomy, the direct connection between the artery of the filum terminale and the arterialized vein was evident, forming the arteriovenous fistula (AVF) at the level of L5-S1 [
Figure 2:
Intraoperative images: (a) image of the artery of the filum terminale directly connected to an arterialized vein, which corresponds to the arteriovenous fistula (arrow). The normal filum terminale (asterisk) is seen distally (left correspond to cranial and right is caudal). (b) Intraoperative neurophysiological examination testing a cauda equina root and (c) the filum terminale. (d) Intraoperative ICG video angiography confirming the exact shunt location of the filum terminale arteriovenous fistula.
Surgery and immediate postoperative period were uneventful. Over the following weeks, both sensory and motor deficits, progressively improved. Ten days after surgery, the patient recovered the voluntary control of the urinary sphincter and the urinary catheter was removed. He underwent physiotherapy and was able to walk unassisted 6 months after surgery.
DISCUSSION
Spinal intradural AVFs represent a rare spinal vascular malformation category.[
The etiology of FTAVFs is unknown. Some authors consider it as a congenital malformation,[
FTAVFs can present with an ascending congestive myelopathy;[
The ascending congestive myelopathy caused by spinal AVF is also known as Foix-Alajouanine syndrome.[
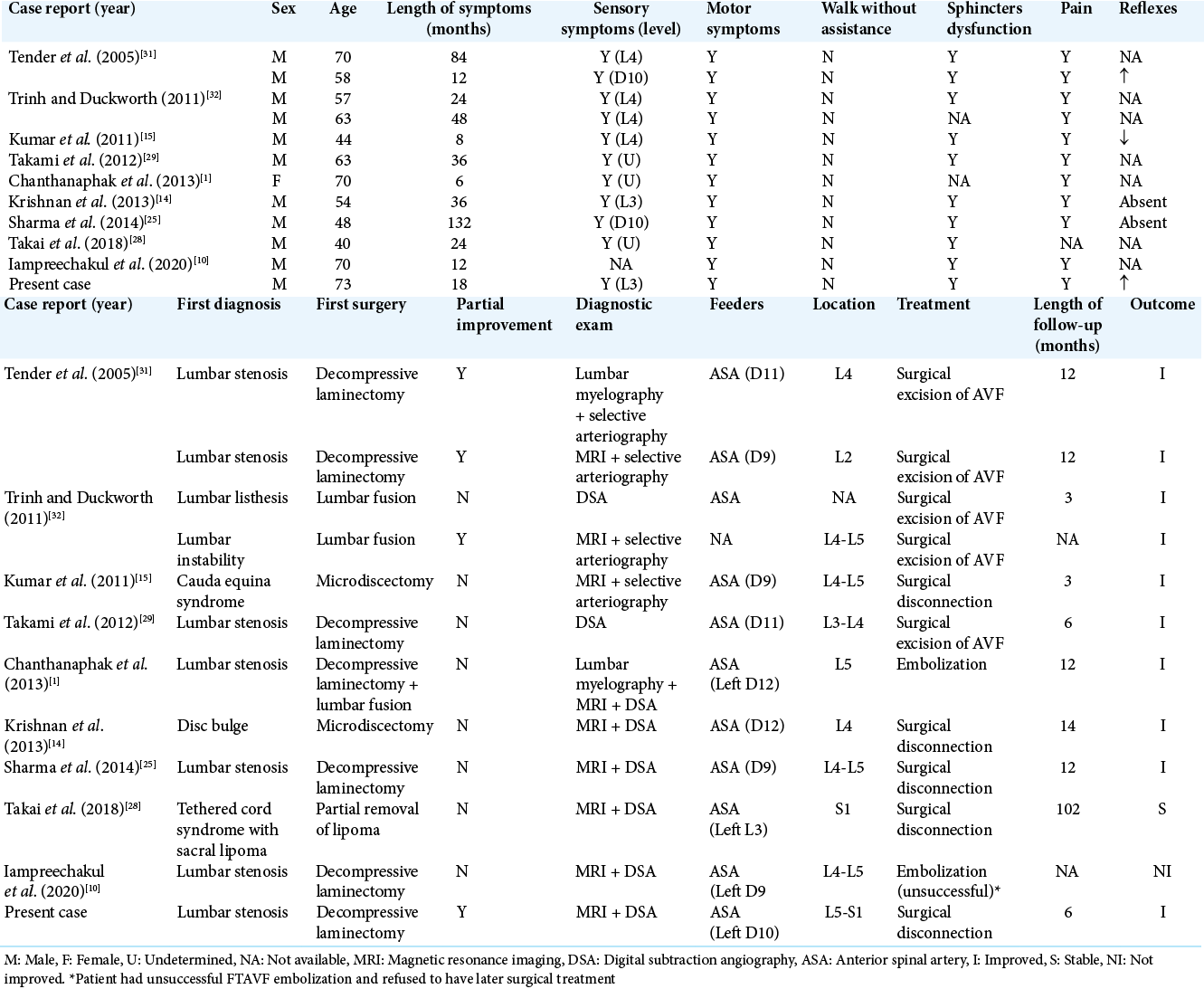
According to our review, there are 66 cases of FTAVF reported in the literature.[
Like the other cases with similar history, our case highlights the importance of clinical awareness to signs such as paraparesis with gait disturbance and sphincter disturbance, in patients with previous surgery for lumbar degenerative disease. Due to the fact that these neurological signs are very rare in this type of pathology, the MRI scans must be carefully analyzed, especially the T2 sequence to search for vascular voids. Although rare, FTAVF is a diagnose that should be considered in cases of failed back surgery syndrome.
The interruption of the FTAVF can be done by both surgical and endovascular techniques.[
The outcome of interrupted FTAVF is dependent on several factors such as duration of symptoms, pretreatment disability, and success of the procedure to close the fistula.[
CONCLUSION
FTAVF is a very rare spinal intradural spinal vascular malformation that can be misdiagnosed, submitted to unnecessary spinal surgery, and even masqueraded as a failed back surgery syndrome. Signs of ascending myelopathy should prompt awareness and the MRI must be carefully evaluated for vascular voids in these cases.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chanthanaphak E, Pongpech S, Jiarakongmun P, Kobkitsuksakul C, Chi CT, Terbrugge KG. Filum terminale arteriovenous fistulas: The role of endovascular treatment. J Neurosurg Spine. 2013. 19: 49-56
2. Ding D, Law AJ, Scotter J, Brew S. Lumbar disc herniation exacerbating venous hypertension from a spinal perimedullary arteriovenous fistula of the filum terminale. J Neurol Sci. 2016. 369: 276-7
3. Fischer S, Perez MA, Bassiouni H, Hopf N, Bäzner H, Henkes H. Arteriovenous fistula of the filum terminale: Diagnosis, treatment, and literature review. Clin Neuroradiol. 2013. 23: 309-14
4. Foix C, Alajouanine T. La myélite nécrotique subaigüe. Rev Neurol. 1926. 33: 1-42
5. Giordan E, Bortolotti C, Lanzino G, Brinjikji W. Spinal arteriovenous vascular malformations in patients with neural tube defects. AJNR Am J Neuroradiol. 2018. 39: 597-603
6. Giordan E, Brinjikji W, Ciceri E, Lanzino G. Arteriovenous fistulae of the filum terminale. J Neurointerv Surg. 2018. 10: 191-7
7. Giordan E, Brinjikji W, Lanzino G. Coexistence of perimedullary arteriovenous fistula and arteriovenous fistula of filum terminale in the same patient. J Neurosurg Sci. 2019. 63: 237-8
8. Hong T, Park JE, Ling F, TerBrugge KG, Tymianski M, Zhang HQ. Comparison of 3 different types of spinal arteriovenous shunts below the conus in clinical presentation, radiologic findings, and outcomes. AJNR Am J Neuroradiol. 2017. 38: 403-9
9. Hong T, Yu JX, Liu W, Bian LS, Yang F, Ma YJ. Filum terminale arteriovenous fistulas with multiple shunt points: A report of two exceptional cases. World Neurosurg. 2018. 118: 235-9
10. Iampreechakul P, Tirakotai W, Wangtanaphat K, Lertbutsayanukul P, Siriwimonmas S. Filum terminale arteriovenous fistula in association with degenerative lumbosacral spinal canal stenosis: Report of 3 cases and review of the literature. World Neurosurg. 2020. 138: 231-41
11. Jellema K, Tijssen CC, van Gijn J. Spinal dural arteriovenous fistulas: A congestive myelopathy that initially mimics a peripheral nerve disorder. Brain. 2006. 129: 3150-64
12. Jin YJ, Kim KJ, Kwon OK, Chung SK. Perimedullary arteriovenous fistula of the filum terminale: Case report. Neurosurgery. 2010. 66: E219-20
13. Kim LJ, Spetzler RF. Classification and surgical management of spinal arteriovenous lesions: Arteriovenous fistulae and arteriovenous malformations. Neurosurgery. 2006. 59: 195-201
14. Krishnan P, Banerjee TK, Saha M. Congestive myelopathy (foix-alajouanine syndrome) due to intradural arteriovenous fistula of the filum terminale fed by anterior spinal artery: Case report and review of literature. Ann Indian Acad Neurol. 2013. 16: 432-6
15. Kumar A, Deopujari C, Mhatre M. Misdiagnosis in a case of non-compressive myelopathy due to a lumbar spinal intradural fistula supplied by the artery of adamkiewicz. Surg Neurol Int. 2011. 2: 12
16. Lagman C, Chung LK, Chitale RV, Yang I. Dural arteriovenous fistula and foix-alajouanine syndrome: Assessment of functional scores with review of pathogenesis. World Neurosurg. 2017. 106: 206-10
17. Lakhdar F, Benzagmout M, Chakour K, Chaoui ME. Spinal arteriovenous fistulas of the filum terminale: Case report and literature. Asian J Neurosurg. 2019. 14: 1277-82
18. Lim SM, Choi IS, David CA. Spinal arteriovenous fistulas of the filum terminale. AJNR Am J Neuroradiol. 2011. 32: 1846-50
19. Macht S, Chapot R, Bieniek F, Hänggi D, Turowski B. Unique sacral location of an arteriovenous fistula of the filum terminale associated with diastematomyelia and lowered spinal cords. Neuroradiology. 2012. 54: 517-9
20. Meisel HJ, Lasjaunias P, Brock M. Modern management of spinal and spinal cord vascular lesions. Minim Invasive Neurosurg. 1995. 38: 138-45
21. Mourier KL, Gobin YP, George B, Lot G, Merland JJ. Intradural perimedullary arteriovenous fistulae: Results of surgical and endovascular treatment in a series of 35 cases. Neurosurgery. 1993. 32: 885-91
22. Rodesch G, Hurth M, Alvarez H, Tadié M, Lasjaunias P. Classification of spinal cord arteriovenous shunts: Proposal for a reappraisal-the bicêtre experience with 155 consecutive patients treated between 1981 and 1999. Neurosurgery. 2002. 51: 374-9
23. Rosenblum B, Oldfield EH, Doppman JL, di Chiro G. Spinal arteriovenous malformations: A comparison of dural arteriovenous fistulas and intradural AVM’s in 81 patients. J Neurosurg. 1987. 67: 795-802
24. Scullen T, Mathkour M, Amenta PS, Dallapiazza RF. Arteriovenous fistula of the filum terminale: A case report and review of the literature. World Neurosurg. 2019. 130: 42-9
25. Sharma P, Ranjan A, Lath R. Arteriovenous fistula of the filum terminale misdiagnosed and previously operated as lower lumbar degenerative disease. Asian Spine J. 2014. 8: 365-70
26. Shin MJ, Kim W, Baik SK, Kim SY, Kim SN. Cauda equina syndrome caused by spinal dural arteriovenous fistula. Ann Rehabil Med. 2011. 35: 928-33
27. Singh R, Lucke-Wold B, Gyure K, Boo S. A review of vascular abnormalities of the spine. Ann Vasc Med Res. 2016. 3: 1-17
28. Takai K, Komori T, Taniguchi M. Angioarchitecture of filum terminale arteriovenous fistulas: Relationship with a tethered spinal cord. World Neurosurg. 2019. 122: e795-804
29. Takami T, Yamagata T, Mitsuhashi Y, Hayasaki K, Ohata K. Direct surgery for spinal arteriovenous fistulas of the filum terminale with intraoperative image guidance. Spine (Phila Pa 1976). 2012. 37: E1524-8
30. Tanioka S, Toma N, Sakaida H, Umeda Y, Suzuki H. A case of arteriovenous fistula of the cauda equina fed by the proximal radicular artery: Anatomical features and treatment precautions. Eur Spine J. 2018. 27: 281-6
31. Tender GC, Vortmeyer AO, Oldfield EH. Spinal intradural arteriovenous fistulas acquired in late adulthood: Absent spinal venous drainage in pathogenesis and pathophysiology. Report of two cases. J Neurosurg Spine. 2005. 3: 488-94
32. Trinh VT, Duckworth EA. Surgical excision of filum terminale arteriovenous fistulae after lumbar fusion: Value of indocyanine green and theory on origins (a technical note and report of two cases). Surg Neurol Int. 2011. 2: 63
33. Wajima D, Nakagawa I, Park HS, Haku T, Wada T, Kichikawa K. A case of filum terminale arterial venous fistula needed a long arterial access for trans-arterial shunt obliteration. Interv Neuroradiol. 2017. 23: 221-7
34. Witiw CD, Fallah A, Radovanovic I, Wallace MC. Sacral intradural arteriovenous fistula treated indirectly by transection of the filum terminale: Technical case report. Neurosurgery. 2011. 69: E780-4