- Sindh Medical College, Jinnah Sindh Medical University, Sindh, Pakistan.
- Department of Neurosurgery, Aga Khan University Hospital, Karachi, Sindh, Pakistan.
Correspondence Address:
Muhammad Ehsan Bari
Department of Neurosurgery, Aga Khan University Hospital, Karachi, Sindh, Pakistan.
DOI:10.25259/SNI_27_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ummey Hani1, Muhammad Ehsan Bari2, Syed Sarmad Bukhari2. Arteriovenous malformation with associated multiple flow-related distal anterior cerebral artery aneurysms: A case report with poor outcomes. 08-Aug-2020;11:232
How to cite this URL: Ummey Hani1, Muhammad Ehsan Bari2, Syed Sarmad Bukhari2. Arteriovenous malformation with associated multiple flow-related distal anterior cerebral artery aneurysms: A case report with poor outcomes. 08-Aug-2020;11:232. Available from: https://surgicalneurologyint.com/surgicalint-articles/10196/
Abstract
Background: Low-grade arteriovenous malformations (AVMs) associated with multiple flow-related distal anterior cerebral artery (DACA) aneurysms are rare occurrences. Here, we present a case of a frontal AVM with three associated DACA aneurysms arising from a single feeder.
Case Description: A 36-year-old male presented to us in the ER with acute-onset dysphasia and altered mental status. Head computed tomography and angiogram showed a spontaneous intracerebral hemorrhage with intraventricular extension and revealed a Spetzler Martin Grade II AVM, being fed by two feeders, with the major feeder from the DACA bearing three flow-related aneurysms. As the patient awaited digital subtraction angiography, his Glasgow Coma Scale dropped and he underwent emergency embolization with Onyx. This was followed by external ventricular drainage. The patient’s neurological status did not improve, and he died following a complicated clinical course.
Conclusion: Multiple DACA aneurysms are a case of both clinical and anatomical rarity and to avoid complications in the clinical course, one must be judicious about the time spent between symptom onset and embolization.
Keywords: Embolization, Intracranial aneurysm, Intracranial arteriovenous malformation
INTRODUCTION
Flow-related aneurysms in the region of distal anterior cerebral artery (DACA) are a rare occurrence, accounting for 9% of the total intracranial aneurysms with multiple aneurysms on the same vessel are rarer.[
CASE PRESENTATION
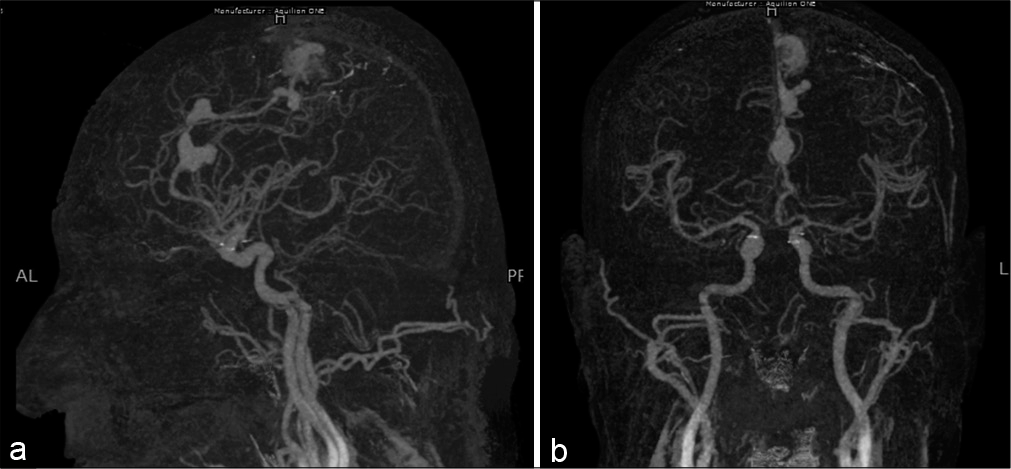
A 36-year-old male with no known comorbidities presented to the emergency room with the complaints of sudden onset aphasia, persistent vomiting, and bilateral lower limb weakness for the past 1 day. On examination, he had a Glasgow Coma Scale (GCS) of 11/15 (E3V2M6). His proximal and distal lower limb powers were 3/5. Rest of the examination was unremarkable. His history was significant for an episode of seizure 1 month back, with symptoms of altered mental state during the fit that resolved spontaneously within a few minutes. Computed tomography (CT) angiogram [
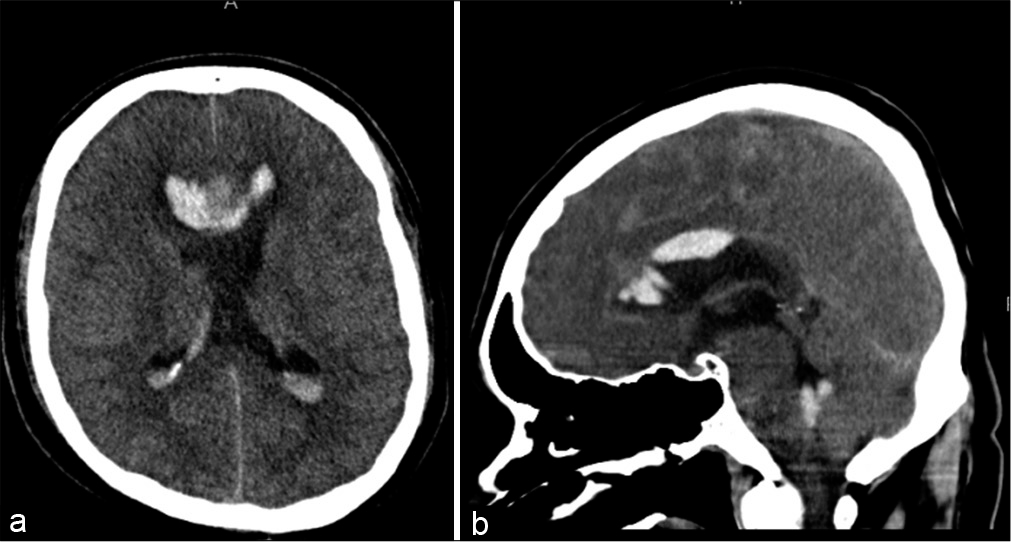
The patient was awaiting digital subtraction angiography for almost 2 days when his GCS suddenly dropped to 5/15, with pupils bilaterally equal, dilated, and nonreactive. He underwent emergency intubation and was shifted to the intensive care unit (ICU). Head CT without contrast and CT angiogram revealed redemonstration of subarachnoid hemorrhage from the proximal largest aneurysm with intraventricular extension predominantly along the corpus callosum, with effaced basal cisterns and an interval increase in both hydrocephalus and cerebral edema [
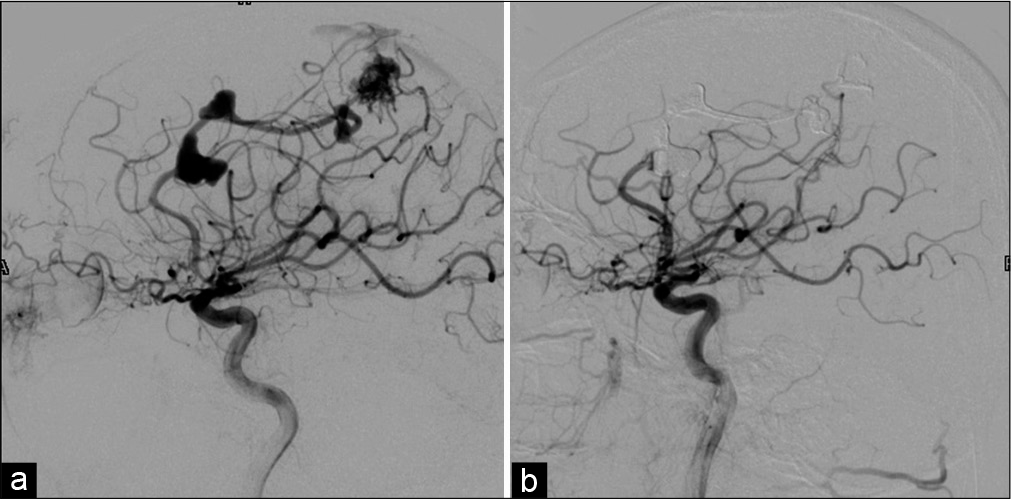
Angiography revealed a Spetzler-Martin Grade 2 AVM, being fed by two vessels, and draining into the superior sagittal sinus through the superficial cortical veins. The major feeder arose from left callosomarginal artery and a minor feeder from the left MCA. The nidus measured 18 × 14 mm in diameter. The angiogram also revealed multiple flow aneurysms on the feeder from left callosomarginal artery, with the largest aneurysm, 14 × 8 mm in size, at the callosomarginal bifurcation. Pericallosal artery, with a relatively sluggish blood flow, was seen arising from its neck, because of which this aneurysm was not embolized. The nidus and rest of the flow aneurysms were embolized using the onyx [
The immediate postprocedural period was uneventful and uncomplicated. The patient, nevertheless, did not regain consciousness and was shifted to the ICU on controlled mechanical ventilation for further management and observation. Postoperative angiogram did not reveal any significant spasm. However, the patient’s neurological status did not improve, and he died in the hospital following a complicated clinical course.
DISCUSSION
DACA aneurysms are usually associated with anterior cerebral artery anomalies and coexist with unrelated multiple aneurysms at different locations.[
DACA aneurysms have an anatomic index that makes them difficult to occlude and hence, results in adverse outcomes. These aneurysms have broad bases and wide necks with originating branches. The small caliber of the parent artery, distal location of the aneurysm resulting in lack of anatomic landmarks, and a very small size[
Bleeding at presentation and rebleeding before and/or after intervention are associated with poor prognosis. Lee et al. reported the risk factors of spontaneous hemorrhage and rebleeding before treatment. These included AVMs with hemorrhage at initial presentation, deep venous drainage, and/or by a single draining vein, AVMs smaller than 2 cm in size, and coexisting aneurysms. Smaller AVMs are high risk for bleeding because of associated increased intra- arterial pressure.[
The endovascular management of AVMs and aneurysms has its own set of complications which need to be reviewed carefully in the context of each lesion’s unique anatomy. Li et al. described acute rerupture after coil embolization as rerupture within 3 days after treatment, resulting in the worst prognoses.[
In 2014, Platz et al. reported lower complication rates in AVMs treated by occlusion through surgery or liquid embolization agents, over coiling.[
CONCLUSION
The natural history of these lesions is rupture and rebleed if untreated. Their treatment is fraught with difficulties due to the management of two complex vascular pathologies. DACA aneurysms tend to be small with broader bases making them difficult to approach endovascularly. Their management should be expedient.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Crowley RW, Ducruet AF, Kalani MY, Kim LJ, Albuquerque FC, McDougall CG. Neurological morbidity and mortality associated with the endovascular treatment of cerebral arteriovenous malformations before and during the Onyx era. J Neurosurg. 2015. 122: 1492-7
2. de Castro-Afonso LH, Nakiri GS, Oliveira RS, Santos MV, Dos Santos AC, Machado HR. Curative embolization of pediatric intracranial arteriovenous malformations using Onyx: The role of new embolization techniques on patient outcomes. Neuroradiology. 2016. 58: 585-94
3. Hung AL, Yang W, Jiang B, Garzon-Muvdi T, Caplan JM, Colby GP. The effect of flow-related aneurysms on hemorrhagic risk of intracranial arteriovenous malformations. Neurosurgery. 2019. 85: 466-75
4. Kozyrev DA, Jahromi BR, Thiarawat P, Choque-Velasquez J, Ludtka C, Goehre F. Three distal anterior cerebral artery aneurysms in the same branch associated with five additional intracranial aneurysms. Surg Neurol Int. 2017. 8: 62
5. Lee KW, Lin YC, Lo CP, Liu CC. Intracerebral hemorrhage following endovascular embolization of brain arteriovenous malformation with a combination of Onyx and n-butyl cyanoacrylate: A case report. Clin Imaging. 2012. 36: 375-8
6. Lehecka M, Porras M, Dashti R, Niemelä M, Hernesniemi JA. Anatomic features of distal anterior cerebral artery aneurysms: A detailed angiographic analysis of 101 patients. Neurosurgery. 2008. 63: 219-28
7. Li K, Guo Y, Zhao Y, Xu B, Xu K, Yu J. Acute rerupture after coil embolization of ruptured intracranial saccular aneurysms: A literature review. Interv Neuroradiol. 2018. 24: 117-24
8. Orz Y. Surgical strategies and outcomes for distal anterior cerebral arteries aneurysms. Asian J Neurosurg. 2011. 6: 13-7
9. Platz J, Berkefeld J, Singer OC, Wolff R, Seifert V, Konczalla J. Frequency, risk of hemorrhage and treatment considerations for cerebral arteriovenous malformations with associated aneurysms. Acta Neurochir (Wien). 2014. 156: 2025-34
10. Şekerci Z, Şanli M, Ergün R, Oral N. Aneurysms of the distal anterior cerebral artery: A clinical series. Neurol Neurochir Pol. 2011. 45: 115-20
11. Signorelli F, Gory B, Pelissou-Guyotat I, Guyotat J, Riva R, Dailler F. Ruptured brain arteriovenous malformations associated with aneurysms: Safety and efficacy of selective embolization in the acute phase of hemorrhage. Neuroradiology. 2014. 56: 763-9
12. Van Rooij WJ, Jacobs S, Sluzewski M, Van der Pol B, Beute GN, Sprengers ME. Curative embolization of brain arteriovenous malformations with onyx: Patient selection, embolization technique, and results. AJNR Am J Neuroradiol. 2012. 33: 1299-304
13. Vergouwen MD, Jong-Tjien-Fa AV, Algra A, Rinkel GJ. Time trends in causes of death after aneurysmal subarachnoid hemorrhage: A hospital-based study. Neurology. 2016. 86: 59-63
14. Wisoff JH, Flamm ES. Aneurysms of the distal anterior cerebral artery and associated vascular anomalies. Neurosurgery. 1987. 20: 735-41