- Neurosurgery Unit, Department of Head and Neck Sugery, Garibaldi Hospital, Catania, Italy,
- Department of Neurosurgery, Health Sciences North, Northern Ontario School of Medicine, Sudbury, Ontario, Canada,
- Department of Medicine, University of Cambridge, Cambridge CB2 OQQ, United Kingdom,
- Department of Neurosurgery, Trauma Center, Gamma Knife Center, Cannizzaro Hospital, Catania, Italy
- Psychology Center Orestano-Pittera, “l’Intreccio” Association, San Giovanni la Punta (CT), Italy
- Neurosurgical Clinic, AOUP “Paolo Giaccone”, Post Graduate Residency Program in Neurologic Surgery, Department of Biomedicine Neurosciences and Advanced Diagnostics, School of Medicine, University of Palermo, Palermo, Italy,
- Department of Neurosurgery, Neurosurgery Clinic, Birgunj, Nepal,
- Department of Medical Physics, University Hospital of Bologna, Bologna, Italy
- Department of Neurosurgery, Policlinico “Tor Vergata”, University of Rome “Tor Vergata”, Rome, Italy.
Correspondence Address:
Gianluca Scalia, Neurosurgery Unit, Department of Head and Neck Sugery, Garibaldi Hospital, Catania, Italy.
DOI:10.25259/SNI_1021_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gianluca Scalia1, Stefano Maria Priola2, Sruthi Ranganathan3, Tejas Venkataram4, Valeria Orestano5, Salvatore Marrone6, Bipin Chaurasia7, Rosario Maugeri6, Domenico Gerardo Iacopino6, Lidia Strigari8, Maurizio Salvati9, Giuseppe Emmanuele Umana4. Assessing the impact of mixed reality-assisted informed consent: A study protocol. 15-Mar-2024;15:88
How to cite this URL: Gianluca Scalia1, Stefano Maria Priola2, Sruthi Ranganathan3, Tejas Venkataram4, Valeria Orestano5, Salvatore Marrone6, Bipin Chaurasia7, Rosario Maugeri6, Domenico Gerardo Iacopino6, Lidia Strigari8, Maurizio Salvati9, Giuseppe Emmanuele Umana4. Assessing the impact of mixed reality-assisted informed consent: A study protocol. 15-Mar-2024;15:88. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12806
Abstract
Background: Informed consent is a crucial aspect of modern medicine, but it can be challenging due to the complexity of the information involved. Mixed reality (MR) has emerged as a promising technology to improve communication. However, there is a lack of comprehensive research on the impact of MR on medical informed consent. The proposed research protocol provides a solid foundation for conducting future investigations and developing MR-based protocols that can enhance patients’ understanding and engagement in the decision-making process.
Methods: This study will employ a randomized controlled trial design. Two arms will be defined: MR-assisted informed consent (MRaIC) as the experimental arm and conventional informed consent (CIC) as the control arm consent, with 52 patients in each group. The protocol includes the use of questionnaires to analyze the anxiety levels and the awareness of the procedure that the patient is going to perform to study the impact of MRaIC versus CIC before medical procedures.
Results: The study will evaluate the impact of MR on patients’ information comprehension, engagement during the process of obtaining informed consent, emotional reactions, and consent decisions. Ethical concerns will be addressed.
Conclusion: This study protocol provides a comprehensive approach to investigate the impact of MR on medical informed consent. The findings may contribute to a better understanding of the effects of MR on information comprehension, engagement during the process of obtaining informed consent, psychological experience, consent decisions, and ethical considerations. The integration of MR technology has the potential to enhance surgical communication practices and improve the informed consent process.
Keywords: Informed consent, Mixed reality, Patient engagement, Surgical interventions, Surgical outcomes
INTRODUCTION
Informed consent is a fundamental ethical and legal requirement in medical practice to ensure that patients have a comprehensive understanding of the risks, benefits, and alternatives associated with a particular surgical or medical procedure. However, traditional methods of delivering information to patients may be limited in their effectiveness.[
Mixed reality (MR) belongs, alongside augmented reality (AR) and virtual reality (VR), to the extended realities group and involves a fusion of real-world and virtual elements. In AR, there exists an overlap but still a separation between physical and digital elements, which can only be visualized. Conversely, in VR, the user is entirely immersed in a virtual space with exclusively digital elements. MR represents an advancement from AR and is distinguished by active interaction with the digital objects displayed within the real world, offering new possibilities to address the challenges in conventional communication techniques improving the informed consent process.[
This study protocol aims to investigate the impact of MR on patient understanding and experiences during communications involving surgical/medical management for their condition, with the goal of improving surgical outcomes and patient experiences.
Objectives
The main objectives of this study protocol are as follows:
To evaluate the effectiveness of MR tools in enhancing patient comprehension during the informed consent process To assess patient satisfaction and engagement when using MR-assisted informed consent (MRaIC) using psychological tests and anxiety questionnaires.
MATERIALS AND METHODS
Study design
This study will employ a randomized controlled trial design. This could be done using a computer-based random number generator to ensure that the process is truly random. The allocation could be done in a 1:1 ratio, meaning an equal number of patients (n = 52) would be assigned to each group. The sample size of 52 participants for each arm was determined based on assumptions of a normal distribution, with guidance from a planned statistical analysis. Patients scheduled for surgical interventions will be randomly assigned to either the MR group or the control group. The MR group will receive the informed consent using MR technology, while the control group will receive the standard informed consent process without MR.
The first anxiety self-evaluation questionnaire [Supplement 1] should be answered before obtaining consent, both MRaIC and conventional informed consent (CIC). After completion of this first questionnaire, consent is taken for the two groups (MRaIC and CIC). Finally, a second questionnaire investigates the level of understanding of the patient about the diagnosis and the therapeutic strategy, which will be answered after consent [Supplement 1]. The anxiety levels pre- and post-consent will be calculated, and the changes in the anxiety levels will be compared between the two groups (MRaIC and CIC). A final consent satisfaction questionnaire is taken, which will be used to compare the differences between patients in the two groups (MRaIC and CIC) [Supplement 1].
Study participants
The study will include adult patients (aged 18 years and above) scheduled for elective surgical interventions or medical procedures. Patients with severe visual or cognitive impairments will be excluded. Patients who consent to participate in this study will be asked to sign a formal agreement and will be randomly allocated to one of the two groups (MRaIC and CIC).
MRa-IC
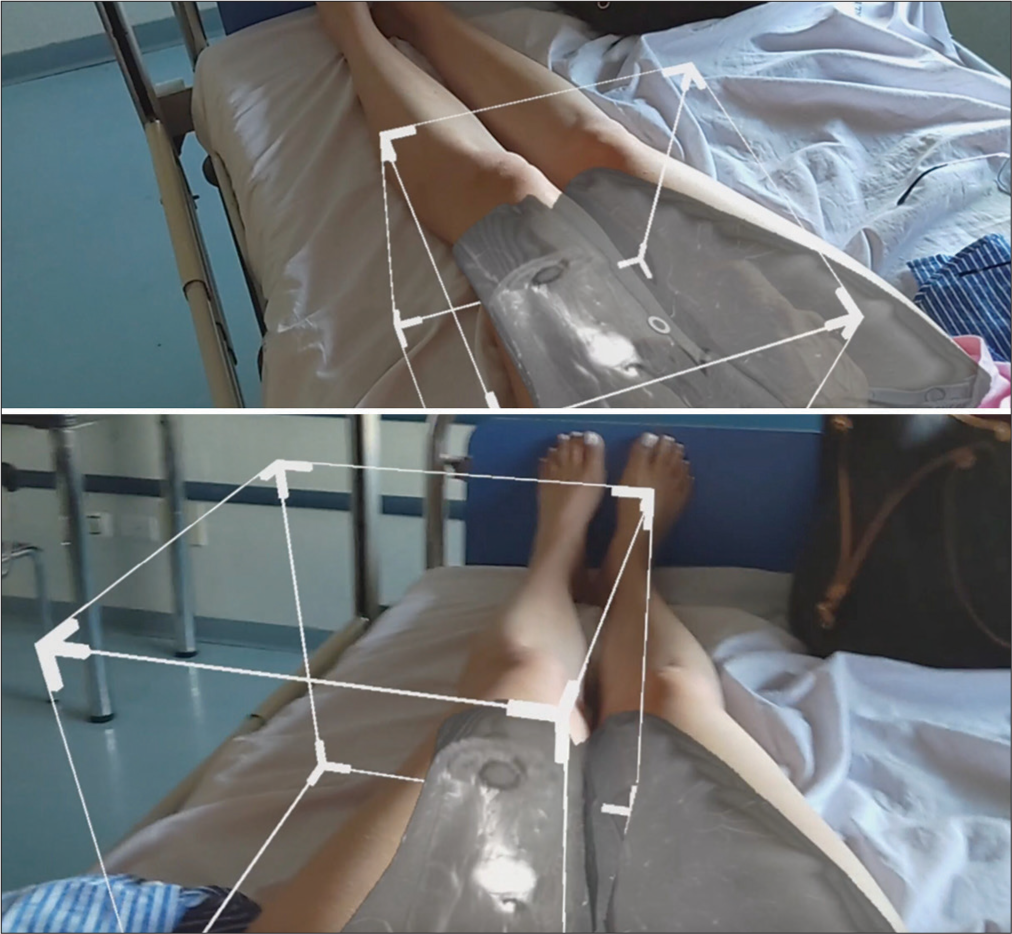
Dicom files (magnetic resonance imaging and computed tomography scans) of radiological imaging performed by the patient will be uploaded to a cloud manager VSI software powered by ApoQlar. The dataset will be anonymized, and a pseudonym will be automatically assigned to each patient. 3D holographic rendering will be produced. Microsoft HoloLens 2 will be used to share with the patient and family members holograms of radiological images. The hologram can be visualized independently or after superimposition on the affected anatomical part of the patient. With the assistance of the medical staff, patients can easily interact with the hologram, including scrolling through the image dataset, zooming in and out of the 3D holographic rendering, and moving around the 3D rendering. Video and audio files acquired during the informed consent process will be archived as part of the clinical files of the patient.
Data collection
Questionnaires will be collected to capture a comprehensive understanding of the impact of MR on surgical/medical informed consent. All data, including patients’ radiological images and visual and audio recordings of meetings, will be anonymized. Radiological images will be collected and stored in the Microsoft VSI clouded database. Data uploaded in the cloud will be automatically deleted after 30 days. Questionnaires and video-audio recordings of the informed consent will be stored as part of the clinical files. A Data Processing Agreement is signed by Health Sciences North and ApoQlar GmbH. Ethical Committee approval obtained by Health Sciences North, Canada Project Number: 21-042.
Statistical analysis
Descriptive statistics will be used to summarize patient characteristics and outcomes. Qualitative data from interviews will be analyzed thematically to identify key themes and patterns.
To compare the MR and control group, non-parametric methods will be applied to ordinal data, such as Likert scale data involving the determination of the ranking for patient understanding, engagement, and satisfaction. The Statistical Package for the Social Sciences software or R-package will be used for statistical analysis. P < 0.05 will be considered statistically significant.
Ethical considerations
Health Sciences North has obtained Ethical Committee approval, Canada Project Number: 21–42. This study will adhere to ethical guidelines and obtain relevant institutional review board approvals in case of a multi-center study. Informed consent will be obtained from all participants prior to their inclusion in the study. Confidentiality and privacy of participant data will be ensured throughout the research process.
RESULTS
Expected outcomes
We anticipate that the use of MR in the informed consent process will lead to improved patient understanding and engagement, reducing preoperative anxiety by promoting patient engagement and strengthening the relationship between patients and medical professionals. By providing a visual and interactive representation of the entire surgical procedure and relevant anatomy, patients may have a clearer understanding of the risks, benefits, and alternatives involved in the procedure. This can contribute to more informed decision-making, potentially enhancing patient satisfaction. Beyond improved patient satisfaction, heavy documentation performed in this study can avoid illicit conduct by doctors, patients, lawyers, and insurance companies, which could lead to a reduction in insurance costs. However, evaluating the impact of this study on insurance costs will require a longer follow-up of 5–10 years. Finally, a potential drawback of the use of MR could involve patients who do not want detailed information about the surgical procedure or are afraid of either the realistic visualization of the procedure or the representation of their condition. Since this differs in each patient, the impact of MR technology can be highly varied.
DISCUSSION
The findings from this study may contribute to the growing body of literature on the use of MR in healthcare.[
One of the potential benefits of using MR in the informed consent process is the ability to provide patients with a more immersive and interactive experience.[
Engagement is another crucial aspect of the informed consent process. Unlike traditional methods of presenting information, such as written documents or verbal explanations, which may not fully engage patients or capture their attention, MR technology has the potential to create a more engaging and memorable experience by allowing patients to interact with the virtual environment actively.[
Video 1
Beyond the benefits of MR use in obtaining informed consent, the challenges of using MR need to be acknowledged. These challenges may include (1) technical limitations, (2) financial constraints, (3) lack of trained personnel, (4) access limitations, and (5) patient receptiveness. Technical limitations can include specialized equipment and software. Second, financial constraints are a minor issue since the costs are exiguous and can be split, involving all the specialties of the hospital. In fact, the total cost could range from tens of thousands to hundreds of thousands of euros for each hospital.[
Future research should explore the long-term effects of using MR in the informed consent process. While this study focuses on immediate outcomes such as patient understanding, engagement, and satisfaction, it is necessary to assess the impact on patient outcomes and clinical decision-making over time. Longitudinal studies can provide insights into the durability of the effects of MR on informed consent and its potential impact on patient compliance, postoperative outcomes, and overall healthcare costs. In addition, the potential applications of MR in other areas of healthcare should be explored. Beyond surgical interventions, MR technology can be utilized in various medical scenarios, such as patient education, preoperative planning, and rehabilitation. Investigating the efficacy and acceptability of MR in different healthcare contexts can provide a more comprehensive understanding of its utility and benefits.
Study limitations
Hawthorne effect
The use of MR technology may introduce a Hawthorne effect, where participants may alter their behavior or responses due to the awareness of being observed or receiving a novel intervention. This effect could potentially influence the outcomes related to patient understanding, engagement, and satisfaction.
Learning curve
The learning curve associated with using MR technology for both patients and health-care providers may influence the findings of this study. Participants may require some time to become familiar with the MR application, potentially affecting the outcomes during the initial stages of the study. Adequate training and support should be provided to minimize the impact of the learning curve.
Follow-up period
The study protocol should determine the appropriate follow-up period to assess the long-term effects of using MR in the informed consent process. Depending on the nature of the surgical interventions, it may be necessary to extend the follow-up period beyond the immediate postoperative stage to capture potential changes in patient outcomes and experiences over time.
Resource constraints
The implementation of MR technology may require additional resources, including technological infrastructure, personnel, and financial investments. The study protocol should consider the potential limitations and challenges associated with resource availability, as this may impact the feasibility and scalability of integrating MR into the informed consent process.
CONCLUSION
The findings from this research may contribute to the advancement of knowledge in the field of healthcare technology and inform evidence-based decision-making regarding the integration of MR into surgical practice. Ultimately, the goal is to enhance patient understanding, engagement, and participation in the informed consent process, leading to improved patient outcomes and satisfaction in the surgical journey. By conducting this study, we can pave the way for the responsible and effective implementation of MR in obtaining clinical informed consent, thus fostering patient-centered, holistic care in the digital era.
Ethical approval
The research/study was approved by the Institutional Review Board at Health Sciences North/Horizon Santé-Nord, Sudbury, Ontario, number 21-042, dated 09/01/2023.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Videos available on:
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
CONSENT INSTRUMENT
List an expected discomfort of the surgery. List an expected benefit of the surgery. List an expected major and minor risk of the surgery. List one consequence of not having your surgery soon. List one alternative to the surgery. Do you understand why you need the surgery? Do you know enough about the surgery that you could basically explain to another person how it will occur? Was the surgical procedure explained to you? Did you understand the explanation of the surgery? Were you informed of the risks of the surgery? Were you informed of the benefits of the surgery? Do you understand the risks of the surgery? Do you understand the benefits of the surgery? Were you informed of the rare possibility of a life-threatening complication from the surgery? Did you know that you could refuse the surgery? Were you given the opportunity to refuse the surgery? Ti è stata data l'opportunità di rifiutare l'intervento? Were you informed about alternatives to the surgery? Sei stato informato sulle alternative all'intervento? Were you informed about possible consequences of not having the surgery? Are you able to locate where your disease is? Riesci a localizzare dove si trova la tua malattia? Did you get all the information you need to make a good decision about the surgery?
PATIENT SATISFACTION
I am satisfied that I was adequately informed about the issues important to my decision. The decision I made was the best decision possible for me personally. I am satisfied that my decision was consistent with my personal values. I expect to successfully carry out (or continue to carry out) the decision I made. I am satisfied that this was my decision to make. I am satisfied with my decision.
References
1. Aliwi I, Schot V, Carrabba M, Duong P, Shievano S, Caputo M. The role of immersive virtual reality and augmented reality in medical communication: A scoping review. J Patient Exp. 2023. 10: 23743735231171562
2. Balci D, Kirimker EO, Raptis DA, Gao Y, Kow AW. Uses of a dedicated 3D reconstruction software with augmented and mixed reality in planning and performing advanced liver surgery and living donor liver transplantation (with videos). Hepatobiliary Pancreat Dis Int. 2022. 21: 455-61
3. Brown R, Bylund CL, Siminoff LA, Slovin SF. Seeking informed consent to Phase I cancer clinical trials: Identifying oncologists’ communication strategies. Psychooncology. 2011. 20: 361-8
4. Cai EZ, Gao Y, Ngiam KY, Lim TC. Mixed reality intraoperative navigation in craniomaxillofacial surgery. Plast Reconstr Surg. 2021. 148: 686e-8
5. Gabay G, Bokek-Cohen Y. What do patients want? Surgical informed-consent and patient-centered care-An augmented model of information disclosure. Bioethics. 2020. 34: 467-77
6. Grant SC. Informed consent-we can and should do better. JAMA Netw Open. 2021. 4: e2110848
7. Hertzsprung N, Krantchev K, Picht T, Roethe AL, Rubarth K, Fuellhase J. Personalized surgical informed consent with stereoscopic visualization in neurosurgery-real benefit for the patient or unnecessary gimmick?. Acta Neurochir (Wien). 2023. 165: 1087-98
8. House PM, Pelzl S, Furrer S, Lanz M, Simova O, Voges B. Use of the mixed reality tool “VSI Patient Education” for more comprehensible and imaginable patient educations before epilepsy surgery and stereotactic implantation of DBS or stereo-EEG electrodes. Epilepsy Res. 2020. 159: 106247
9. Jain S, Gao Y, Yeo TT, Ngiam KY. Use of mixed reality in neurooncology: A single centre experience. Life (Basel). 2023. 13: 398
10. Krishnamurti T, Argo N. A patient-centered approach to informed consent: Results from a survey and randomized trial. Med Decis Making. 2016. 36: 726-40
11. Liberatore MJ, Wagner WP. Virtual, mixed, and augmented reality: A systematic review for immersive systems research. Virtual Real. 2021. 25: 1-27
12. McCloskey K, Turlip R, Ahmad HS, Ghenbot YG, Chauhan D, Yoon JW. Virtual and augmented reality in spine surgery: A systematic review. World Neurosurg. 2023. 173: 96-107
13. Mishra R, Narayanan MD, Umana GE, Montemurro N, Chaurasia B, Deora H. Virtual reality in neurosurgery: Beyond neurosurgical planning. Int J Environ Res Public Health. 2022. 19: 1719
14. Park J, Son W, Park KS, Kang DH, Lee J, Oh CW. Educational and interactive informed consent process for treatment of unruptured intracranial aneurysms. J Neurosurg. 2017. 126: 825-30
15. Perin A, Galbiati TF, Ayadi R, Gambatesa E, Orena EF, Riker NI. Informed consent through 3D virtual reality: A randomized clinical trial. Acta Neurochir (Wien). 2021. 163: 301-8
16. Pietrzykowski T, Smilowska K. The reality of informed consent: Empirical studies on patient comprehension-systematic review. Trials. 2021. 22: 57
17. Scott H, Griffin C, Coggins W, Elberson B, Abdeldayem M, Virmani T. Virtual reality in the neurosciences: Current practice and future directions. Front Surg. 2022. 8: 807195
18. Singhal I, Kaur G, Neefs D, Pathak A. A literature review of the future of oral medicine and radiology, oral pathology, and oral surgery in the hands of technology. Cureus. 2023. 15: e45804
19. Umana GE, Palmisciano P, Montemurro N, Scalia G, Radovanovic D, Cassar K, editors. Introducing mixed reality for clinical uses. Handbook of research on implementing digital reality and interactive technologies to achieve society 5.0. United States: IGI Global; 2022. p. 524-48
20. Umana GE, Scalia G, Yagmurlu K, Mineo R, Di Bella S, Giunta M. Multimodal simulation of a novel device for a safe and effective external ventricular drain placement. Front Neurosci. 2021. 15: 690705
21. Wagner D, Bear M. Patient satisfaction with nursing care: A concept analysis within a nursing framework. J Adv Nurs. 2009. 65: 692-701
22. Wrzesińska N, Rivas H, Boillat T, editors. Mixed and augmented reality in healthcare: When will it deliver its promises?. Digital health: Health informatics. Cham: Springer; 2023. p.
23. Yeung AW, Tosevska A, Klager E, Eibensteiner F, Laxar D, Stoyanov J. Virtual and augmented reality applications in medicine: Analysis of the scientific literature. J Med Internet Res. 2021. 23: e25499
24. Yu QJ, Pun J. Promoting patient engagement in medical informed consent-a qualitative study of Chinese doctors’ communication strategies. Health Commun. 2023. 38: 71-9