- Department of Cerebrovascular Surgery, Saitama Medical University International Medical Center, Hidaka, Japan.
- Department of Neurosurgery, Ohkawara Neurosurgical Hospital, Muroran, Japan.
- Department of Neurosurgery, Muroran City General Hospital, Muroran, Japan.
Correspondence Address:
Yushiro Take, Department of Cerebrovascular Surgery, Saitama Medical University International Medical Center, Hidaka, Japan.
DOI:10.25259/SNI_309_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yushiro Take1,2, Manabu Osakabe2, Mai Okawara2, Hiroyuki Yamaguchi2, Hiroshi Ohyama3, Takahiro Maeda2, Hiroki Kurita1. Association between population changes and the number of endovascular thrombectomies. 16-Jun-2023;14:207
How to cite this URL: Yushiro Take1,2, Manabu Osakabe2, Mai Okawara2, Hiroyuki Yamaguchi2, Hiroshi Ohyama3, Takahiro Maeda2, Hiroki Kurita1. Association between population changes and the number of endovascular thrombectomies. 16-Jun-2023;14:207. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12365
Abstract
Background: Randomized controlled trials have demonstrated the efficacy of mechanical thrombectomy (MT) for acute ischemic stroke. However, few studies indicate an association between the number of mechanical thrombectomies and population changes. We aimed to clarify the association between population changes and the number of mechanical thrombectomies for proper allocation of limited medical resources.
Methods: We retrospectively analyzed data from 162 patients who underwent MT for large vessel occlusion at our hospitals and compared the number of mechanical thrombectomies per 100,000 person/year to population changes in five regions covered by our hospitals within 2015–2016 and 2017–2019. We performed a simple linear regression analysis to determine the association between population changes and the number of mechanical thrombectomies.
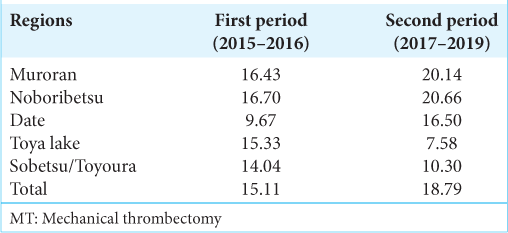
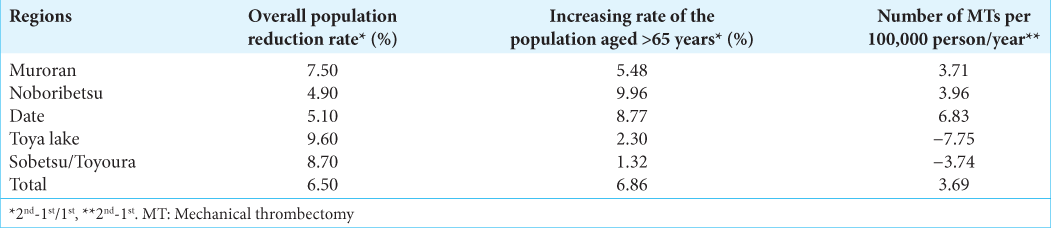
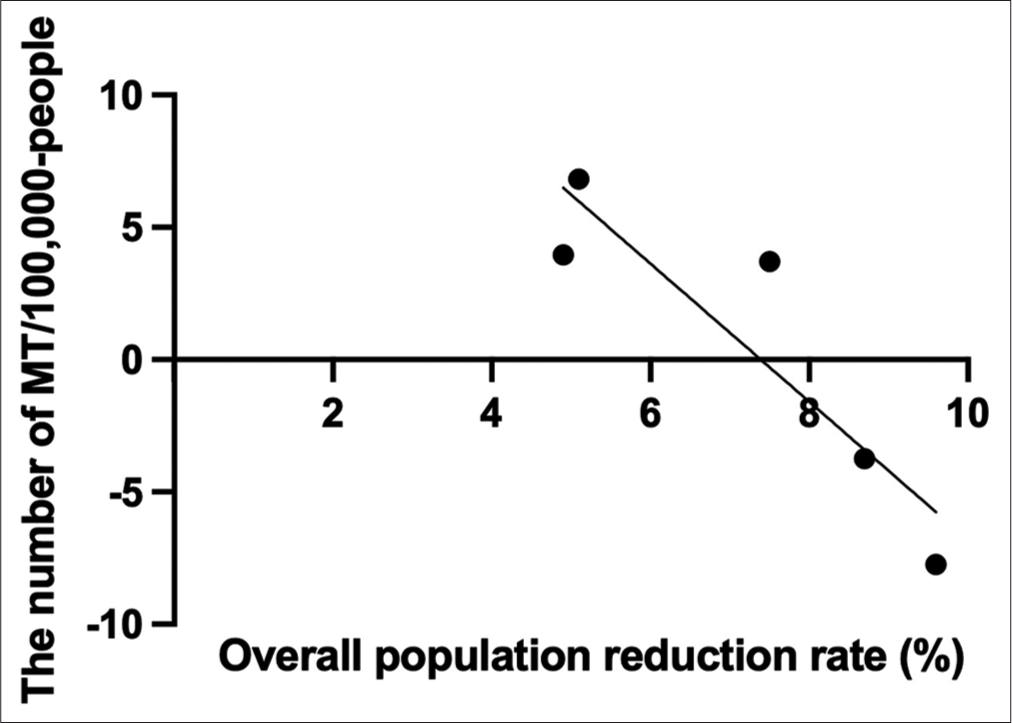
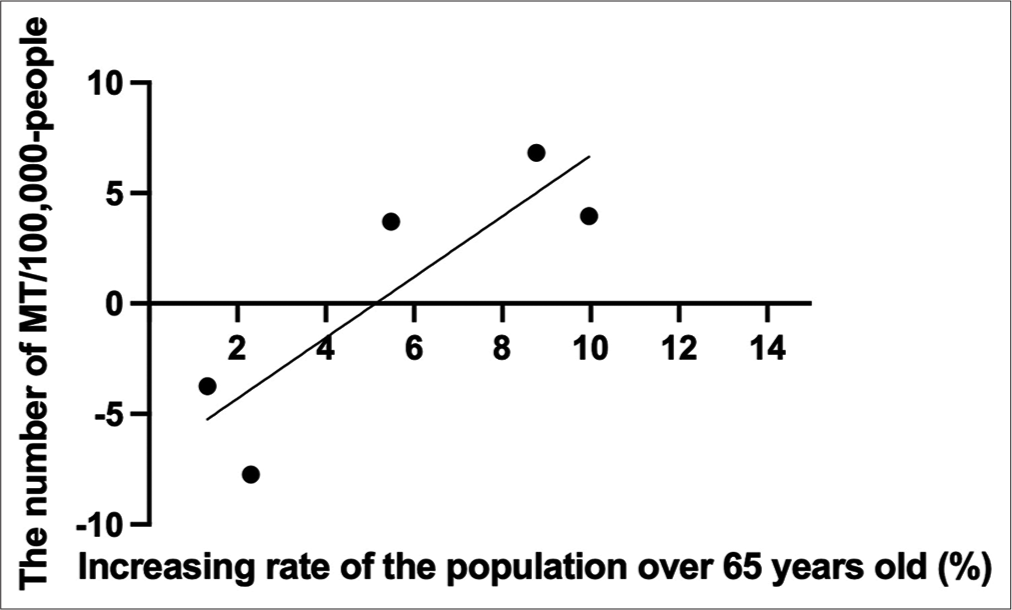
Results: Overall, the number of mechanical thrombectomies increased from 15.1 to 19. However, a significant decrease was noted in Toya Lake and Sobetsu/Toyoura. Furthermore, there was a significant negative linear correlation between the overall population reduction rate and the number of mechanical thrombectomies and a positive linear correlation between the increased proportion of the population aged >65 years and the number of mechanical thrombectomies.
Conclusion: The number of mechanical thrombectomies may decrease in areas where the overall population reduction rate exceeds 8% or the increased rate of the population aged >65 years is
Keywords: Acute ischemic stroke, Aging population, Large vessel occlusion, Mechanical thrombectomy, Population changes
INTRODUCTION
Several randomized controlled trials, including MR CLEAN, ESCAPE, EXTEND-IA, SWIFT PRIME, and REVASCAT, have demonstrated the efficacy of mechanical thrombectomy (MT) for acute ischemic strokes (AIS) from large vessel occlusions (LVO).[
MATERIALS AND METHODS
We retrospectively analyzed the Japanese Diagnosis Procedure Combination (DPC) data of all 162 patients who underwent MT for LVO at our hospitals between 2015 and 2019. The DPC data include national administrative hospital discharge data that describe detailed clinical information used by various clinical studies.[
RESULTS
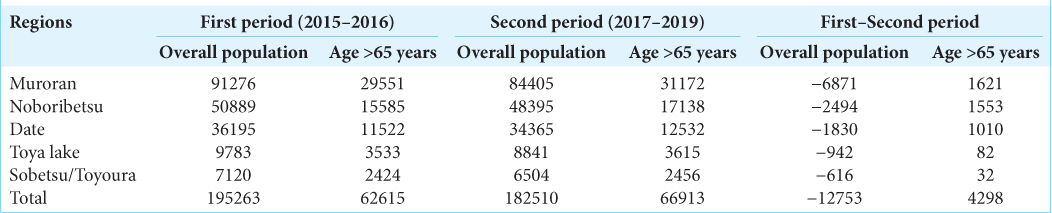
The entire region’s population decreased, and the population aged >65 increased [
DISCUSSION
We observed an association between population changes and the number of MTs. A previous study reported regional differences in the proportion of performed MTs, consistent with our findings.[
Another predictive factor for the number of MTs is the current number of MTs per 100,000 persons/year. Theoretically, the total number of patients with LVO eligible for MT is 10–20/100,000 person-years.[
Few studies have indicated an association between population changes and the number of MTs. Therefore, it is not easy to compare our results to other regions. However, the population will decline with an inverted pyramid age distribution in all countries except Sub-Saharan Africa, North Africa, and the Middle East.[
Limitations
This study has several limitations. First, it was a retrospective, two-center, and small-scale study, limiting the statistical strength of our findings. Second, the observation period is short because our hospitals started MTs in 2015. Third, the number of MTs might have increased by promoting MT therapy during the second period. In addition, the domestic guidelines for performing MT have changed based on the results of the DAWN and DEFUSE3 trials in 2018, which may have influenced the number of MTs performed during the second period.[
CONCLUSION
We observed an association between the population changes and the number of MTs. Our findings suggested that the number of MTs performed may decrease in areas where the overall population reduction rate exceeds 8% or the increase rate of the population aged >65 years is <4%. Based on these results, it is necessary to continue establishing a system for MT in most areas that have yet to reach these levels.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Adcock AK, Schwamm LH, Smith EE, Fonarow GC, Reeves MJ, Xu H. Trends in use, outcomes, and disparities in endovascular thrombectomy in US patients with stroke aged 80 years and older compared with younger patients. JAMA Netw Open. 2022. 5: e2215869
2. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018. 378: 708-18
3. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015. 372: 11-20
4. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015. 372: 1009-18
5. Chen RL, Balami JS, Esiri MM, Chen LK, Buchan AM. Ischemic stroke in the elderly: An overview of evidence. Nat Rev Neurol. 2010. 6: 256-65
6. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015. 372: 1019-30
7. Japan Medical Association. Japan Medical Analysis Platform. Available from: https://www.jmap.jp/cities/detail/medical_area/109 [Last accessed on 2023 Jun 01].
8. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015. 372: 2296-306
9. Lisabeth LD, Brown DL, Zahuranec DB, Kim S, Lim J, Kerber KA. Temporal trends in ischemic stroke rates by ethnicity, sex, and age (2000-2017): The brain attack surveillance in corpus Christi project. Neurology. 2021. 97: e2164-72
10. MacKenzie IE, Moeini-Naghani I, Sigounas D. Trends in endovascular mechanical thrombectomy in treatment of acute ischemic stroke in the United States. World Neurosurg. 2020. 138: e839-46
11. Nishimura A, Nishimura K, Onozuka D, Matsuo R, Kada A, Kamitani S. Development of quality indicators of stroke centers and feasibility of their measurement using a nationwide insurance claims database in Japan-J-ASPECT study―. Circ J. 2019. 83: 2292-302
12. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018. 378: 11-21
13. Omama S, Tanno K, Inoue Y, Ogasawara K, Fukuda T, Oikawa Y. The potential of a stroke registry using diagnosis procedure combination data from all hospitals in a Japanese prefecture. Cerebrovasc Dis. 2022. 51: 447-52
14. Rai AT, Seldon AE, Boo S, Link PS, Domico JR, Tarabishy AR. A population-based incidence of acute large vessel occlusions and thrombectomy eligible patients indicates significant potential for growth of endovascular stroke therapy in the USA. J Neurointerv Surg. 2017. 9: 722-6
15. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015. 372: 2285-95
16. United Nations Department of Economic and Social Affairs, Population Divisi, editors. World Population Prospects 2022: Summary of Results. 2022. p.
17. Vollset SE, Goren E, Yuan CW, Cao J, Smith AE, Hsiao T. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: A forecasting analysis for the global burden of disease study. Lancet. 2020. 396: 1285-306
18. Writing Group Members; Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ. Heart disease and stroke statistics-2016 update: A report from the American heart association. Circulation. 2016. 133: e38-360
19. Yagi M, Yasunaga H, Matsui H, Morita K, Fushimi K, Fujimoto M. Impact of rehabilitation on outcomes in patients with ischemic stroke: A nationwide retrospective cohort study in Japan. Stroke. 2017. 48: 740-6