- Department of Neurosurgery, Clinical Neurosciences Center, University of Utah, Salt Lake City, Utah, USA
Correspondence Address:
Min S. Park
Department of Neurosurgery, Clinical Neurosciences Center, University of Utah, Salt Lake City, Utah, USA
DOI:10.4103/sni.sni_28_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jian Guan, Michael Karsy, William T. Couldwell, Richard H. Schmidt, Philipp Taussky, Min S. Park. Association of travel distance and cerebral aneurysm treatment. 06-Sep-2017;8:210
How to cite this URL: Jian Guan, Michael Karsy, William T. Couldwell, Richard H. Schmidt, Philipp Taussky, Min S. Park. Association of travel distance and cerebral aneurysm treatment. 06-Sep-2017;8:210. Available from: http://surgicalneurologyint.com/surgicalint-articles/association-of-travel-distance-and-cerebral-aneurysm-treatment/
Abstract
Background:The management of cerebral aneurysms requires a significant level of expertise, and large areas of the country have limited access to such advanced neurosurgical care. The objective of this study was to examine the impact of longer travel distance on aneurysm management.
Methods:Adult patients treated for cerebral aneurysms from January 1, 2013 to January 1, 2016, were retrospectively identified. Demographic data, socioeconomic data, aneurysm characteristics, and postoperative outcomes were evaluated with univariate and multivariable analysis to determine factors that influenced treatment prior to or after rupture.
Results:Two hundred fifty aneurysms (87 ruptured) were treated during the study period. Patients treated after rupture were more likely than those treated before rupture to live in areas with lower median household income (62% vs. 45%, P = 0.009), to live further from the treatment center (68% vs. 40%, P P P = 0.002), lower income (1.899, 95% CI 1.003–3.596, P = 0.049), and aneurysm location (P = 0.035) remained significantly associated with treatment after rupture.
Conclusions:Patients who must travel further to receive advanced neurovascular care are more likely to receive treatment for their aneurysms only after they rupture. Further inquiry is needed to determine how to better provide neurosurgical treatment to patients living in underserved areas.
Keywords: Aneurysm clipping, cerebral aneurysm, endovascular treatment, flow diversion, travel distance
INTRODUCTION
Cerebral aneurysms are estimated to be present in more than 3% of the population,[
The shortage of healthcare professionals is not limited to neurosurgery, and significant discussion is ongoing in both the medical literature[
MATERIALS AND METHODS
Patient cohort
After obtaining approval from the institutional review board with a waiver of informed consent, we queried a clinical database to obtain information about patients 18 years and older who underwent treatment for cerebral aneurysm between January 1, 2013, and January 1, 2016. Patients were excluded if geographic, demographic, or socioeconomic data were unavailable. All endovascular procedures were performed by one of two endovascular neurosurgeons, and all open surgical procedures were performed by one of four neurosurgeons. All procedures were performed at a quaternary referral center that provides care to the American Intermountain West—a geographic region comprising the states of Utah, Nevada, and parts of Idaho, Arizona, Colorado, Montana, and New Mexico and serving a population of more than 3 million.[
Data collection
Demographic, geographic, socioeconomic, aneurysm- related, and postoperative information was collected on all patients. Demographic data included age, race/ethnicity (dichotomized into Caucasian and non-Caucasian), sex, marital status, and insurance type (divided into private, Medicaid/self-pay, and Medicare). Each patient's ZIP code was collected. The U.S. Census data (
Aneurysm-related data included rupture status at time of treatment, treatment modality, aneurysm size (dichotomized based on a cutoff size of 7 mm), and aneurysm location. Treatment modality was dichotomized into open clipping or endovascular (consisting of coiling with or without stent assistance and flow diversion). Aneurysm location was divided into seven categories based on those used in previous papers.[
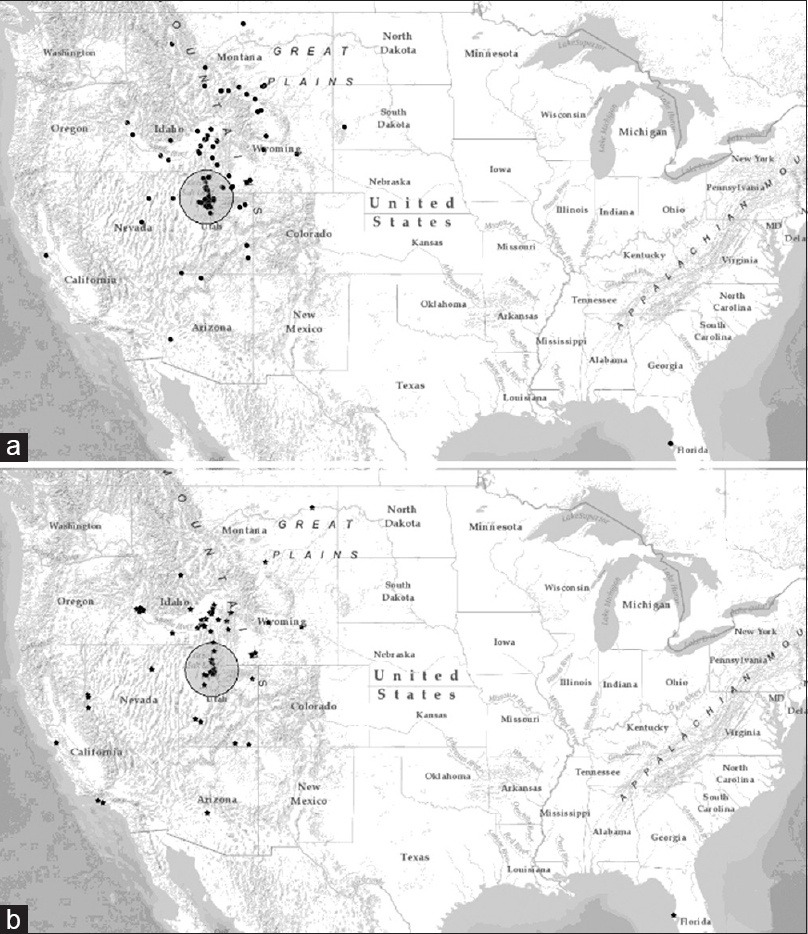
Mapping of aneurysm distribution was performed using ArcGIS (ESRI 2011. ArcGIS Online: Release 10.3. Redlands, CA: Environmental Systems Research Institute,
Statistical analysis
Continuous variables were analyzed using Student's t-test, and categorical variables were analyzed using Chi-squared analysis. Univariate and multivariable analysis were first performed to compare patients with ruptured aneurysms and those with unruptured aneurysms (i.e., to assess timing of treatment). Variables were selected for this multivariable model based on factors that reached a P < 0.2 on univariate analysis. Univariate analysis was then used to compare patients who lived less than or greater than the median hospital travel distance. In all analyses, P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS V20.0 (IBM Corporation, Armonk, NY).
RESULTS
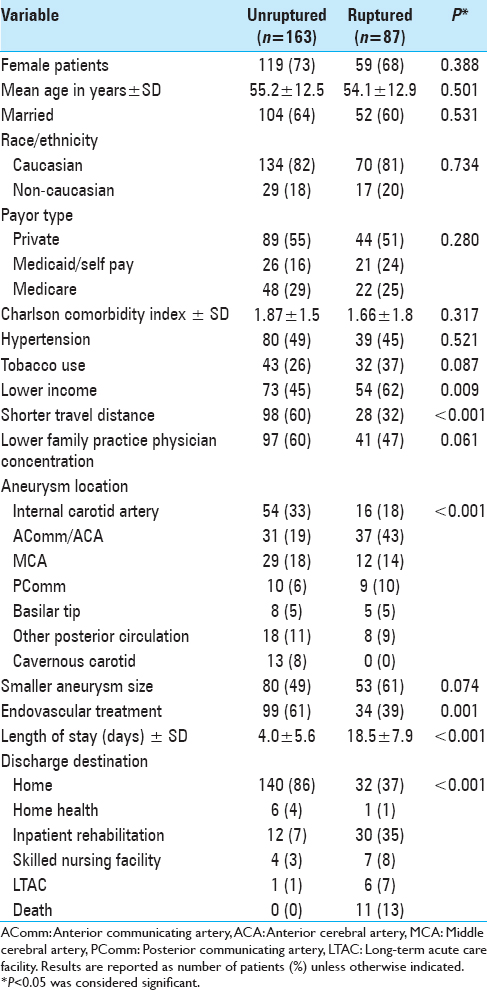
Demographic characteristics of patients in the ruptured and unruptured treatment groups were largely similar, with no significant differences between the groups in age, sex, marital status, race/ethnicity, CCI, or insurance type [
Aneurysm location differed significantly between the ruptured and unruptured groups (P < 0.001). Ruptured aneurysms were significantly more likely to arise from the anterior communicating artery, anterior cerebral artery, or posterior communicating artery, whereas those treated prior to rupture were more likely to arise from the internal carotid artery. Ruptured aneurysms were also significantly more likely to be treated with open clipping than were unruptured aneurysms (61% vs. 39%, P < 0.001).
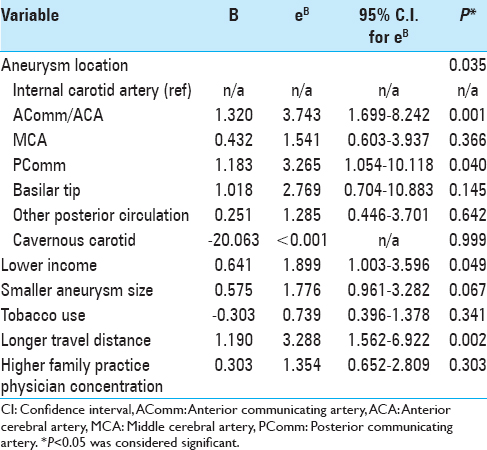
Patients treated for ruptured aneurysms had significantly longer hospital stays than those treated for unruptured aneurysms (18.5 ± 7.9 days vs. 4.0 ± 5.6 days, P < 0.001) and were significantly less likely to discharge home (P < 0.001). Variables selected for the multivariable model included tobacco use, aneurysm size, aneurysm location, median household income, travel distance, and local FPP concentration. Discharge destination, treatment modality, and length of stay met criteria, but were not included in our model as we thought that it was unlikely these variables had an impact on aneurysm treatment timing. In our multivariable model, aneurysm location (P < 0.035,
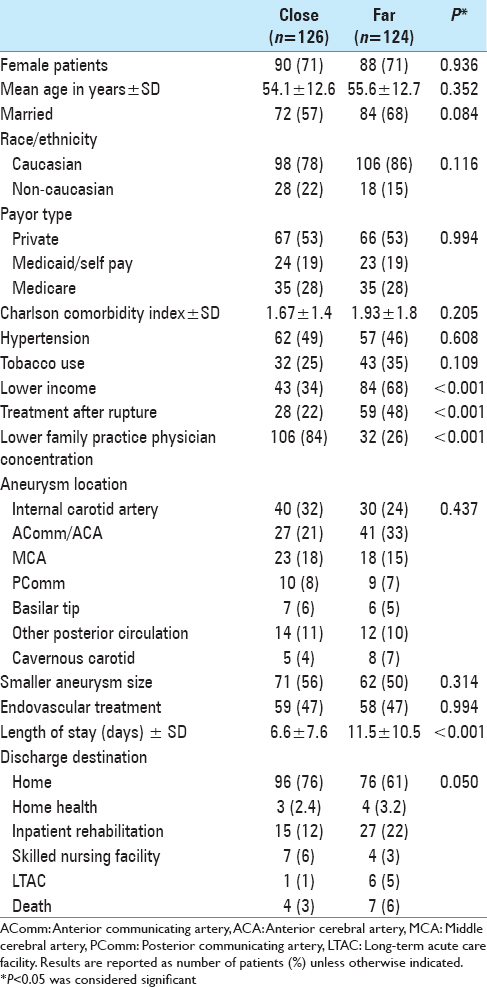
Patients who were “far” from our medical center were similar in all assessed demographic factors when compared with the “close” group, including age, sex, race/ethnicity, and marital status [
DISCUSSION
Aneurysmal subarachnoid hemorrhage is a devastating pathology that can result in permanent disability even in survivors.[
The need to travel long distances to obtain medical care is a common problem in the United States.[
Our study suggests that patients who must travel significant distances to receive neurosurgical care for cerebral aneurysms are more than three times as likely to be treated for a ruptured aneurysm as those who live in closer proximity to a comprehensive neurovascular center. This difference is independent of other factors including socioeconomic status, aneurysm characteristics, and other demographic variables. Patients in our cohort who lived further from our center actually tended to have more ready access to primary care physicians, as indicated by a lower average FPP-to-patient ratio (1 FPP to 2572 patients in the longer distance group vs. 1 FPP to 3433 patients in the shorter distance group), possibly because of a higher population density in urban areas. With regard to timing of cerebral aneurysm treatment; however, there was no significant benefit to living in a region with a higher concentration of primary care physicians. Prior studies have supported the idea that a simple increase in physician number is not sufficient to improve patient outcomes[
There are several possible explanations for our study's findings. Patients who live further away from a cerebrovascular care center may simply be less likely to be evaluated for a cerebrovascular lesion. The most common symptom leading to discovery of unruptured cerebral aneurysms within our cohort was headache, with the majority of patients being initially evaluated by a family practitioner or a neurologist. In practices where cerebrovascular lesions are rarely encountered, vessel imaging may not be available or commonly employed in the evaluation of such a nonspecific finding. Patients living further away from a treatment center may also defer elective aneurysm treatment for logistical reasons—an unwillingness or inability to travel dozens if not hundreds of miles for the initial intervention and then for any required follow-up. Patients in our cohort who were from areas with lower median household income were also more likely to be treated after aneurysm rupture than electively, a finding which has previously been described,[
The location of the aneurysm in the circulation also significantly affected the chance of treatment after rupture in our cohort, with both posterior communicating artery lesions and anterior communicating artery lesions more than three times as likely as internal cerebral artery aneurysms to receive intervention only after hemorrhage. The dangers of posterior communicating artery aneurysms are well documented and accepted.[
Our study has several limitations. The first is its retrospective nature, which increases its vulnerability to confounders. One possible confounder is aneurysm treatment at other facilities—specifically the possibility that elective aneurysms are preferentially treated locally, while patients with subarachnoid hemorrhage are referred to high-volume centers. The literature, however, does not appear to support this, with the most recent national data suggesting that a similar percentage of unruptured and ruptured aneurysms are treated at low-volume centers.[
Socioeconomic status has been demonstrated time and again to be associated with a variety of healthcare quality measures,[
We examined a relatively small cohort of patients at a single center, thus limiting our power and the generalizability of our findings. The latter may especially be true given the nature of how healthcare providers are distributed throughout the nation. We were unable to assess the absolute incidence of unruptured aneurysms present in the population from which our hospital draws, nor do we have access to information on what proportion of these aneurysms are detected in each location. As a result, we are unable to make firm conclusions as to what impact travel distance has on rates of aneurysm diagnosis or rates of referral—only that of the cases referred to our center requiring treatment, a higher proportion of those from distant locations are treated following rupture. Finally, we did not examine specific characteristics of patients within the ruptured aneurysm group, such as time from rupture to presentation, presenting acuity (i.e., Hunt and Hess grade, World Federation of Neurological Surgeons grade), and rate of loss to follow-up. Subsequent studies examining these factors would undoubtedly be informative.
CONCLUSIONS
In this single-institution cohort, patients living further from our medical center were more likely to undergo treatment for their cerebral aneurysm emergently after rupture than electively. Further studies are needed to better define this association and to determine strategies to provide advanced neurosurgical care to remote regions of the country.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. . The International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms-risk of rupture and risks of surgical intervention. N Engl J Med. 1998. 339: 1725-1733
2. Agarwal S, Menon V, Jaber WA. Outcomes after acute ischemic stroke in the United States: Does residential ZIP code matter?. J Am Heart Assoc. 2015. 4: e001629-
3. Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med. 1999. 341: 1359-67
4. Attar MA, Hanrahan K, Lang SW, Gates MR, Bratton SL. Pregnant mothers out of the perinatal regionalization's reach. J Perinatol. 2006. 26: 210-4
5. Becker G, Newsom E. Socioeconomic status and dissatisfaction with health care among chronically ill African Americans. Am J Public Health. 2003. 93: 742-8
6. Bijlenga P, Ebeling C, Jaegersberg M, Summers P, Rogers A, Waterworth A. Risk of rupture of small anterior communicating artery aneurysms is similar to posterior circulation aneurysms. Stroke. 2013. 44: 3018-26
7. Bonita R, Thomson S. Subarachnoid hemorrhage: Epidemiology, diagnosis, management, and outcome. Stroke. 1985. 16: 591-4
8. Brinjikji W, Lanzino G, Kallmes DF, Cloft HJ. Cerebral aneurysm treatment is beginning to shift to low volume centers. J Neurointerv Surg. 2014. 6: 349-52
9. Brinjikji W, Rabinstein AA, Lanzino G, Cloft HJ. Racial and ethnic disparities in the treatment of unruptured intracranial aneurysms: A study of the Nationwide Inpatient Sample 2001-2009. Stroke. 2012. 43: 3200-6
10. Chalouhi N, Hoh BL, Hasan D. Review of cerebral aneurysm formation, growth, and rupture. Stroke. 2013. 44: 3613-22
11. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987. 40: 373-83
12. Dusick JR, Gonzalez NR. Management of arterial vasospasm following aneurysmal subarachnoid hemorrhage. Semin Neurol. 2013. 33: 488-97
13. Dyer B, Strong T. How to tackle America's physician shortage. Fortune. 2015. p.
14. Etminan N, Brown RD, Beseoglu K, Juvela S, Raymond J, Morita A. The unruptured intracranial aneurysm treatment score: A multidisciplinary consensus. Neurology. 2015. 85: 881-9
15. Froelich JJ, Neilson S, Peters-Wilke J, Dubey A, Thani N, Erasmus A. Size and location of ruptured intracranial aneurysms: A 5-Year Clinical Survey. World Neurosurg. 2016. 91: 260-5
16. Geronimus AT, Bound J. Use of census-based aggregate variables to proxy for socioeconomic group: Evidence from national samples. Am J Epidemiol. 1998. 148: 475-86
17. Goldberg DS, French B, Forde KA, Groeneveld PW, Bittermann T, Backus L. Association of distance from a transplant center with access to waitlist placement, receipt of liver transplantation, and survival among US veterans. JAMA. 2014. 311: 1234-43
18. Gross BA, Lai PM, Du R. Impact of aneurysm location on hemorrhage risk. Clin Neurol Neurosurg. 2014. 123: 78-82
19. Haddad AQ, Singla N, Gupta N, Raj GV, Sagalowsky AI, Margulis V. Association of distance to treatment facility on quality and survival outcomes after radical cystectomy for bladder cancer. Urology. 2015. 85: 876-82
20. Last accessed on 2016 Mar 10. Available from: http://www.acshpri.org/documents/ACSHPRI_Surgical_Workforce_in_US_apr2010.pdf.
21. Hoh BL, Chi YY, Lawson MF, Mocco J, Barker FG. Length of stay and total hospital charges of clipping versus coiling for ruptured and unruptured adult cerebral aneurysms in the Nationwide Inpatient Sample database 2002 to 2006. Stroke. 2010. 41: 337-42
22. Krannich R, Krannich R, Luloff A, Field D.editors. A sociodemographic portrait of the intermountain west. People, places and landscapes: Social change in high amenity rural areas. Dordrecht, Netherlands: Springer; 2011. p. 27-43
23. Krieger N. Overcoming the absence of socioeconomic data in medical records: Validation and application of a census-based methodology. Am J Public Health. 1992. 82: 703-10
24. Lai PM, Dasenbrock H, Lin N, Du R. The impact of insurance status on the outcomes after aneurysmal subarachnoid hemorrhage. PLoS One. 2013. 8: e78047-
25. Latimer SF, Wilson FC, McCusker CG, Caldwell SB, Rennie I. Subarachnoid haemorrhage (SAH): Long-term cognitive outcome in patients treated with surgical clipping or endovascular coiling. Disabil Rehabil. 2013. 35: 845-50
26. Leake CB, Brinjikji W, Kallmes DF, Cloft HJ. Increasing treatment of ruptured cerebral aneurysms at high-volume centers in the United States. J Neurosurg. 2011. 115: 1179-83
27. Lin CC, Bruinooge SS, Kirkwood MK, Olsen C, Jemal A, Bajorin D. Association between geographic access to cancer care, insurance, and receipt of chemotherapy: Geographic distribution of oncologists and travel distance. J Clin Oncol. 2015. 33: 3177-85
28. Longstreth WT, Nelson LM, Koepsell TD, van Belle G. Cigarette smoking, alcohol use, and subarachnoid hemorrhage. Stroke. 1992. 23: 1242-9
29. Mayer ML, Beil HA, von Allmen D. Distance to care and relative supply among pediatric surgical subspecialties. J Pediatr Surg. 2009. 44: 483-95
30. Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S, Hashimoto N. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med. 2012. 366: 2474-82
31. Mukherjee D, Kosztowski T, Zaidi HA, Jallo G, Carson BS, Chang DC. Disparities in access to pediatric neurooncological surgery in the United States. Pediatrics. 2009. 124: e688-96
32. Murayama Y, Takao H, Ishibashi T, Saguchi T, Ebara M, Yuki I. Risk analysis of unruptured intracranial aneurysms: Prospective 10-year cohort study. Stroke. 2016. 47: 365-71
33. Park J, Woo H, Kang DH, Kim Y. Critical age affecting 1-year functional outcome in elderly patients aged ≥70 years with aneurysmal subarachnoid hemorrhage. Acta Neurochir (Wien). 2014. 156: 1655-61
34. Rosman J, Slane S, Dery B, Vogelbaum MA, Cohen-Gadol AA, Couldwell WT. Is there a shortage of neurosurgeons in the United States?. Neurosurgery. 2013. 73: 354-
35. Steinbrook R. Easing the shortage in adult primary care--is it all about money?. N Engl J Med. 2009. 360: 2696-9
36. . The Editorial Board. Bottlenecks in training doctors. The New York Times. 2014. p.
37. Thompson BG, Brown RD, Amin-Hanjani S, Broderick JP, Cockroft KM, Connolly ES. Guidelines for the Management of Patients With Unruptured Intracranial Aneurysms: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015. 46: 2368-400
38. Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systematic review and meta-analysis. Lancet Neurol. 2011. 10: 626-36
39. Voelker R. Experts say projected surgeon shortage a “looming crisis” for patient care. JAMA. 2009. 302: 1520-1
40. Watson DE, McGrail KM. More doctors or better care?. Healthc Policy. 2009. 5: 26-31
41. Weissman JS, Stern R, Fielding SL, Epstein AM. Delayed access to health care: Risk factors, reasons, and consequences. Ann Intern Med. 1991. 114: 325-31
42. Williams K, Schneider B, Lajos P, Marin M, Faries P. Supply and demand: Will we have enough vascular surgeons by 2030?. Vascular. 2016. 24: 414-20
43. Zacharia BE, Bruce SS, Carpenter AM, Hickman ZL, Vaughan KA, Richards C. Variability in outcome after elective cerebral aneurysm repair in high-volume academic medical centers. Stroke. 2014. 45: 1447-52