- College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
- King Abdullah International Medical Research Center, Jeddah, Saudi Arabia
- Department of Neurosurgery, King Fahad General Hospital, Al-Madinah Al-Munawarah, Saudi Arabia
- Department of Surgery, Division of Neurosurgery, Ministry of the National Guard-Health Affairs, Jeddah, Saudi Arabia.
- Department of Pathology and Laboratory Medicine, Ministry of National Guard-Health Affairs, Jeddah, Saudi Arabia.
Correspondence Address:
Abdulaziz Hamzah, College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia.
DOI:10.25259/SNI_477_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abdulaziz Hamzah1,2, Alaa Adel Ashqar1,2, Maryam Alshanqiti3, Ahmed Lary1,2,4, Alaa Samkari1,2,5. Awake craniotomy for fenestration of motor cortex neuroglial cyst: A case report. 08-Sep-2023;14:323
How to cite this URL: Abdulaziz Hamzah1,2, Alaa Adel Ashqar1,2, Maryam Alshanqiti3, Ahmed Lary1,2,4, Alaa Samkari1,2,5. Awake craniotomy for fenestration of motor cortex neuroglial cyst: A case report. 08-Sep-2023;14:323. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12532
Abstract
Background: Neuroglial cysts (NCs) are uncommon benign cysts covered by an epithelial layer, accounting for
Case Description: We present a case of a 35-year-old male without prior medical history, who presented to the neurosurgery clinic with complaints of absence seizures. A neurological examination revealed subtle weakness in the left upper limb. Brain magnetic resonance imaging demonstrated a large cystic lesion in the posterior frontal and anterior parietal lobes of the right hemisphere. The patient underwent an awake craniotomy, during which a cystoventricular fenestration was performed on the motor cortex cyst. Histopathological examination confirmed the diagnosis of NC. At the 4-month follow-up, the patient experienced complete recovery, with normal strength (5/5) in all limbs and absence of seizure remission.
Conclusion: This case highlights the successful use of awake craniotomy for the fenestration of an NC in the motor cortex. Given the rarity of NCs, there is no consensus on the optimal treatment strategy. However, in this particular case, the patient achieved complete recovery without any new neurological deficits following the procedure.
Keywords: Awake craniotomy, Cyst fenestration, Glioependymal cyst, Neuroepithelial cyst, Neuroglial cyst
INTRODUCTION
Neuroglial cysts (NCs), also referred to as glioependymal cysts or neuroepithelial cysts, are benign cystic formations characterized by the presence of an epithelial lining. These cysts are considered rare, accounting for <1% of all intracranial cysts. They can emerge at various locations within the neuraxis.[
DESCRIPTION OF THE CASE
A 35-year-old male with no known medical illnesses presented to the neurosurgery clinic with a 2-month history of absence seizures with a frequency of 4–7 times a day. He had weakness in his left-hand grip, with a power examination of 4 ± 5. A satellite sign in the left upper limb was observed on the forearm-rolling test. Other than the left upper limb weakness, his remaining neurological examination was unremarkable.
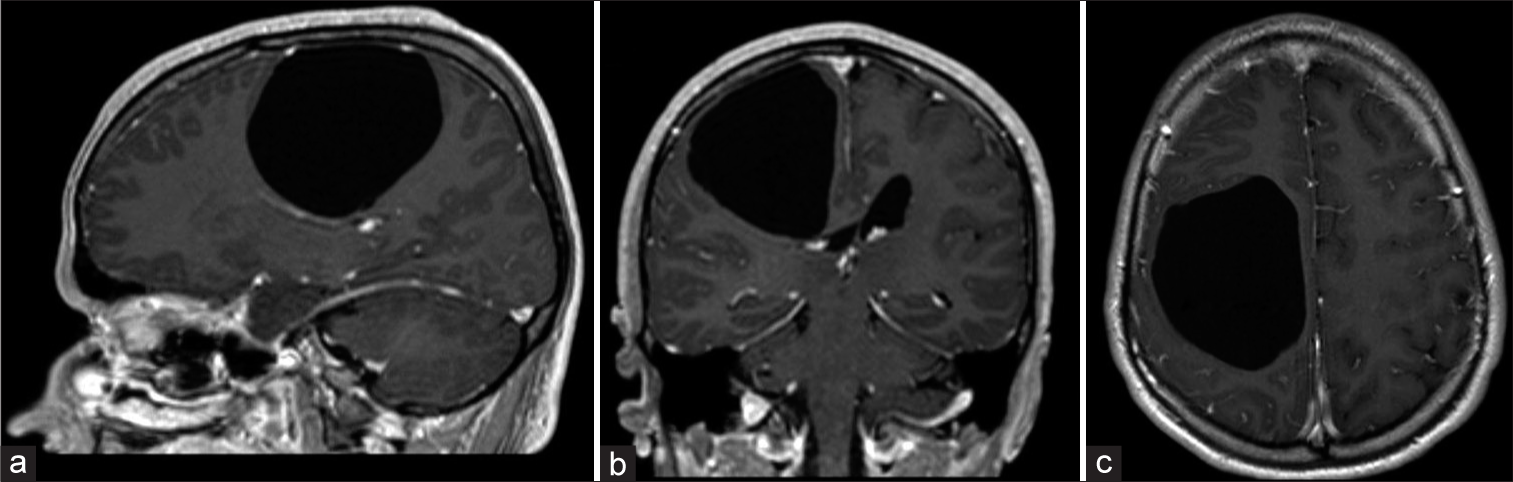
Brain magnetic resonance imaging (MRI) with contrast showed a large nonenhancing right cystic intra-axial lesion involving the posterior frontal and anterior parietal lobes measuring 6.7 × 6.1 × 5.3 cm AP × TS × CC (anteroposteriorly, transversely, and coronal). [
Surgical technique
Phase one (asleep)
Operative preparation and nerve block
After general anesthesia, scalp sterilization commenced. A nerve block was used on the right side on the supraorbital, supratrochlear, zygomaticotemporal, auriculotemporal, and greater occipital and lesser occipital nerves. The supraorbital, supratrochlear, zygomaticotemporal, and auriculotemporal were also blocked on the left side. Local anesthetic was also applied on the sites of Mayfield pins.
Position and incision
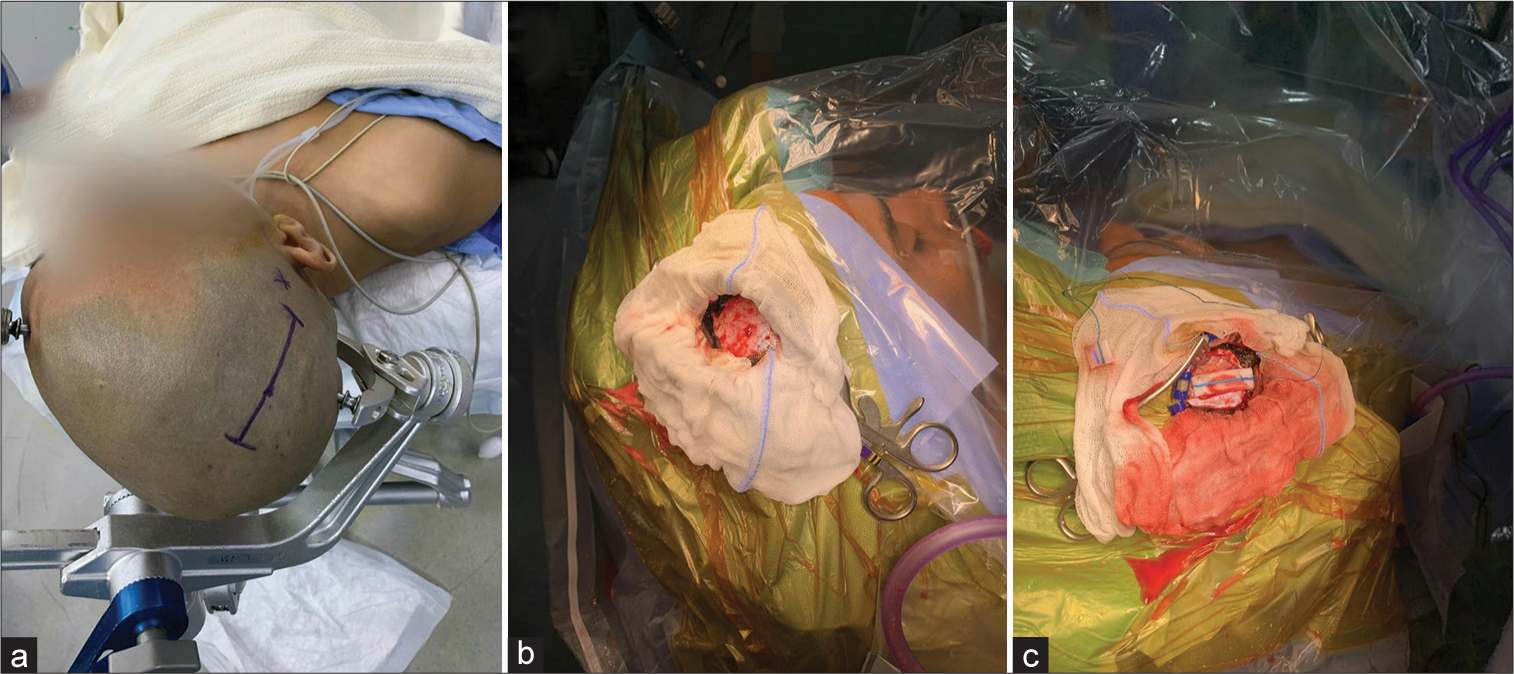
The patient was positioned supine, and his head was flexed and tilted slightly to the left. A three-point Mayfield skull clamp was placed. The incision was marked to be straight, extending from the midline to 2 cm just above the ear pinna. Intra-operative images are illustrated in
Exposure
After retracting the pericranium, two burr holes were placed on the incision’s superior and inferior poles, dissecting the dura, and a craniotomy was completed. The dura was opened in a curvilinear fashion with the base posteriorly. The brain was bulging, and furosemide bolus was given. The first phase of the operation had finished.
Phase two (awake)
The patient was roused from sleep for the second phase of the operation, and a neurological assessment was conducted. His results were consistent with the preoperative baseline, and a series of tests were conducted to evaluate the language, the left upper limb, and the left lower limb. These tests were repeated throughout the phase with no abnormalities detected.
Surgical technique
Using neuronavigation to pinpoint the thinnest and most superficial part of the cyst, the surgical team performed coagulation of the pia and a corticectomy. A ventricular cannula was inserted into the cyst, and 10 cc of clear fluid resembling cerebrospinal fluid (CSF) was released. The cyst deflated, and a second corticectomy was done to inspect the cyst wall. A thin, whitish membrane was observed, and a biopsy sample was taken. Multiple septations were found, which were fenestrated and connected. The cyst was fenestrated to the ventricle.
Phase three (asleep) and closing
The operation moved to the third “asleep” phase of the awake craniotomy, and the patient was sedated again. Hemostasis was achieved; then, the dura was approximated primarily by silk, followed by fibrin sealant and a hemostatic agent. Microplates and screws fixed the bone, and bone dust was used to plug the burr holes. Pericranium was approximated, and subcutaneous tissue was sutured. The skin was closed by staplers.
Postoperative course
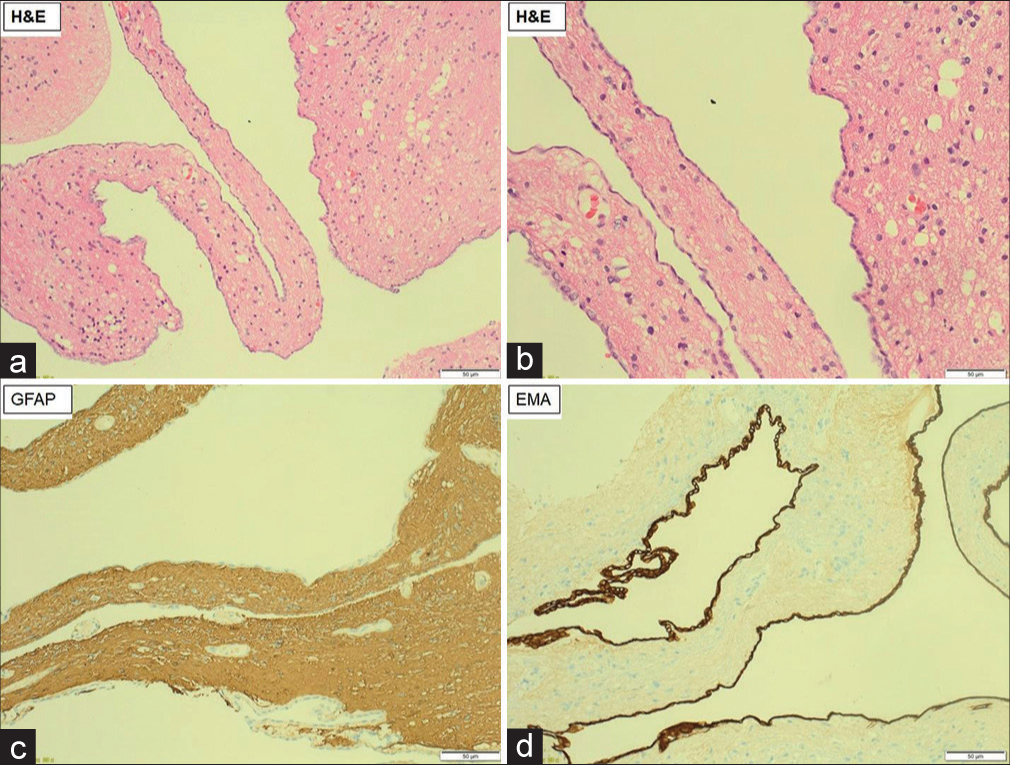
Histopathology specimen showed nonciliated cuboidal to simple squamous (nonkeratinizing) epithelial lining surrounded by gliosis and calcification. Immunohistochemistry study showed cytokeratins (CK)+, epithelial membrane antigen (EMA) focal weak+, S100+, glial fibrillary acidic protein (GFAP)-. The tissue diagnosis is a neuroepithelial cyst. [
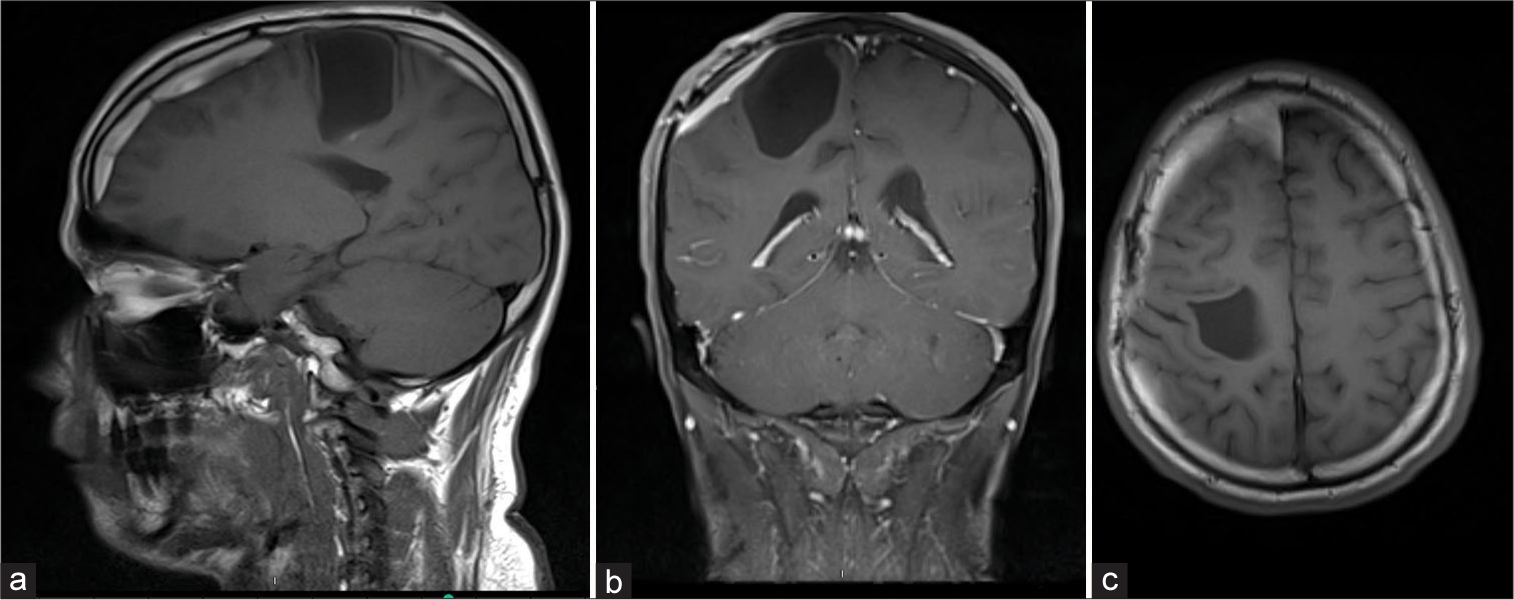
In a clinic follow-up appointment 4 months after the operation, the patient made a full recovery with a power of 5/5 in all limbs, no episodes of absence seizure since the surgery. Follow-up MRI showed interval reduction in the cystic lesion, measuring 3.7 × 3 × 3.5 cm compared to the preoperative 6.7 × 6.1 × 5.3 cm [
DISCUSSION
NCs are a rare type of intracranial cysts, comprising <1% of all cases.[
MRI is the imaging of choice for NCs, with features similar to most intracranial benign cystic lesions, which include smooth and rounded borders, a nonenhancing wall, and minimal mass effect even in large lesions. MRIs show NCs to be isointense to CSF in all sequences.[
The surgical principles used to treat arachnoid cysts can be applied to the management of NCs and other intracranial benign cysts. As this is a rare condition, a consensus on the treatment strategy has not been established. The most common procedure implemented in the literature was cystoventricular fenestration, and none reported awake craniotomy.[
CONCLUSION
This paper presents a case of a young adult with subtle motor weakness in his left upper limb and absence of seizure who made a full recovery after an awake craniotomy. This case highlights the importance of considering awake craniotomy as a treatment option for NCs located in the eloquent cortex. Further, research is needed to establish a consensus on the treatment strategy for NCs.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alvarado AM, Smith KA, Chamoun RB. Neuroendoscopic fenestration of glioependymal cysts to the ventricle: report of 3 cases. J Neurosurg. 2018. 131: 1615-9
2. Eyselbergs M, Vanhoenacker FM, De Cuyper K, Kools D. Epilectic seizure due to neuroglial cyst. JBR BTR. 2012. 95: 142-3
3. Robles LA, Paez JM, Ayala D, Boleaga-Duran B. Intracranial glioependymal (neuroglial) cysts: A systematic review. Acta Neurochir (Wien). 2018. 160: 1439-49