- Department of Neurosurgery, Desert Regional Medical Center, Palm Springs, California, United States.
- Kentucky College of Osteopathic Medicine, University of Pikeville, Pikeville, Kentucky, United States.
- School of Medicine, University of California Riverside, Riverside, California, United States.
- School of Medicine, University of New Mexico, Albuquerque, New Mexico, United States.
Correspondence Address:
Brian Fiani
School of Medicine, University of New Mexico, Albuquerque, New Mexico, United States.
DOI:10.25259/SNI_153_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Brian Fiani1, Taylor Reardon2, Jacob Selvage2, Alden Dahan3, Mohamed H. El-Farra3, Philine Endres3, Taha Taka3, Yasmine Suliman3, Alexander Rose4. Awake spine surgery: An eye-opening movement. 10-May-2021;12:222
How to cite this URL: Brian Fiani1, Taylor Reardon2, Jacob Selvage2, Alden Dahan3, Mohamed H. El-Farra3, Philine Endres3, Taha Taka3, Yasmine Suliman3, Alexander Rose4. Awake spine surgery: An eye-opening movement. 10-May-2021;12:222. Available from: https://surgicalneurologyint.com/surgicalint-articles/10792/
Abstract
Background: Awake surgery is performed in multiple surgical specialties, but historically, awake surgery in the field of neurosurgery was limited to craniotomies. Over the past two decades, spinal surgeons have pushed for techniques that only require regional anesthesia as they may provide reduced financial burdens on patients, faster recovery times, and better outcomes. The list of awake spine surgeries that have been found in the literature include: laminectomies/discectomies, anterior cervical discectomy and fusions (ACDFs), lumbar fusions, and dorsal column (DC) stimulator placement.
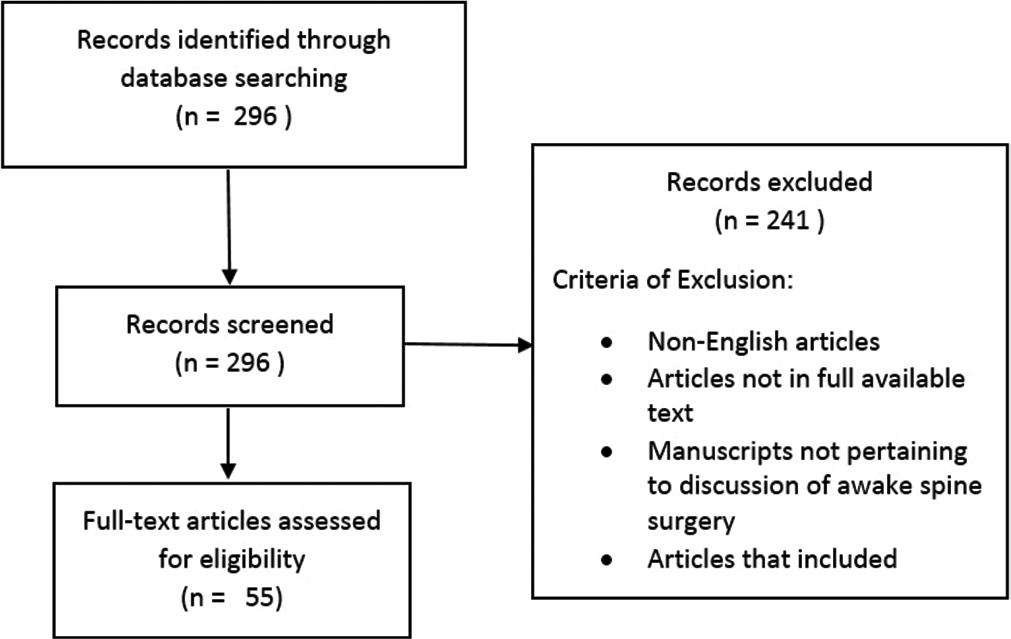
Methods: An extensive review of the published literature was conducted through PubMed database with articles containing the search term “awake spine surgery.” No date restrictions were used.
Results: The search yielded 293 related articles. Cross-checking of articles was conducted to exclude of duplicate articles. The articles were screened for their full text and English language availability. We finalized those articles pertaining to the topic. Findings have shown that lumbar laminectomies performed with local anesthesia have shown shorter operating time, less postoperative nausea, lower incidence of urinary retention and spinal headache, and shorter hospital stays when compared to those performed under general anesthesia. Lumbar fusions with local anesthesia showed similar outcomes as patients reported better postoperative function and fewer side effects of general anesthesia. DC stimulator placement performed with local anesthesia is advantageous as it allows real time patient feedback for surgeons as they directly test affected nerves. However, spontaneous movement during the placement of DC stimulators is associated with higher failure rates when compared to general anesthesia (29.7% vs. 14.9%). Studies have shown that the use of local anesthesia during ACDFs has no significant differences when compared to general anesthesia, and patient’s report better tolerated pain with general anesthesia.
Conclusion: The use of awake spine surgery is beneficial for those who cannot undergo general anesthesia. However, it is limited to patients who can tolerate prone positioning with no central airway (i.e., normal BMI with a healthy airway), have no pre-existing mental health conditions (e.g., anxiety), and require a minimally invasive procedure with a short operating time. Future studies should focus on long-term efficacies of these procedures that provide further insight on the indications and limitations of awake spine surgery.
Keywords: Conscious sedation, Enhanced recovery after surgery, Minimally invasive, Neural feedback, Neuroanesthesia
INTRODUCTION
Awake surgery is performed in multiple surgical specialties including: obstetrics, orthopedics, neurosurgery, and cardiothoracic surgery.[
The objectives of this literature review are to provide a contemporary analysis of awake spine surgery procedures with published outcomes, discuss the benefits and limitations of awake spine surgery, and identify who are the ideal candidates for awake spine surgery.
COMMONLY PERFORMED AWAKE SPINE SURGERIES
Laminectomy/discectomy
Spinal anesthesia for lumbar surgery is becoming increasingly popular, as it can be performed with a variety of techniques and medication, and often yields better patient outcomes than general anesthesia. Early reports of the use of spinal anesthesia for lumbar laminectomy or discectomy have been promising. In one case-controlled study of 400 lumbar laminectomies, spinal anesthesia allowed for shorter operation time, less postoperative nausea, and lower incidence of urinary retention and spinal headache when compared to general anesthesia.[
Anterior cervical discectomy and fusion (ACDF)
Advances in awake spine surgery for ACDF are lagging behind their lumbar counterparts.[
Lumbar fusion
Consistent with the current focus and drive of decreasing the morbidity and negative outcomes of neurological surgery, lumbar fusion surgery has more recently been performed without generalized anesthesia in an effort to improve outcomes and accelerate recovery. The operative procedure has been discussed previously in the literature[
Dorsal column (DC) stimulator placement
DC stimulation has been proven as a successful treatment option in managing neuropathic pain through its mechanism of delivering doses of electrical current. DC stimulator placement has been performed in awake and nonawake methods. While awake surgery offers the surgeon the ability to directly test the affected nerves, increasing the likelihood of a desirable outcome, nonawake surgery is associated with reduced instances of spontaneous movements.[
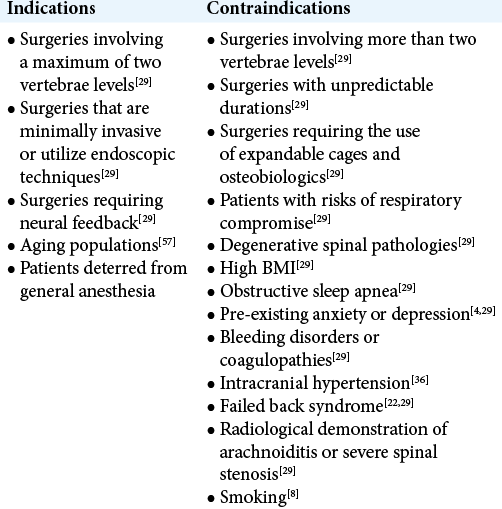
INDICATIONS
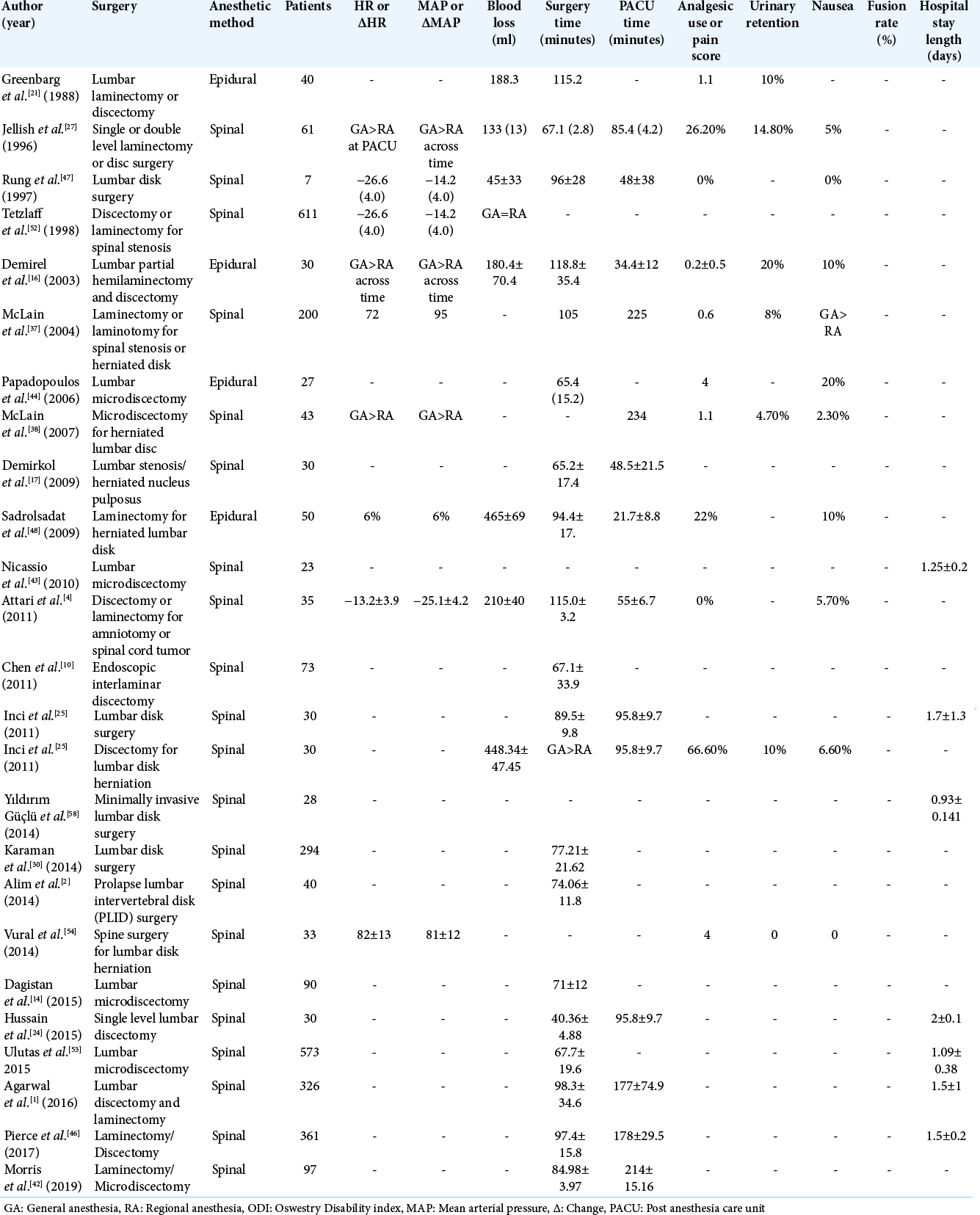
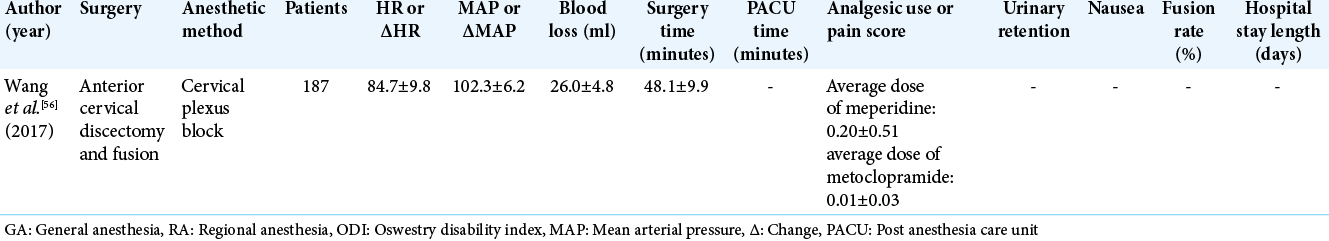
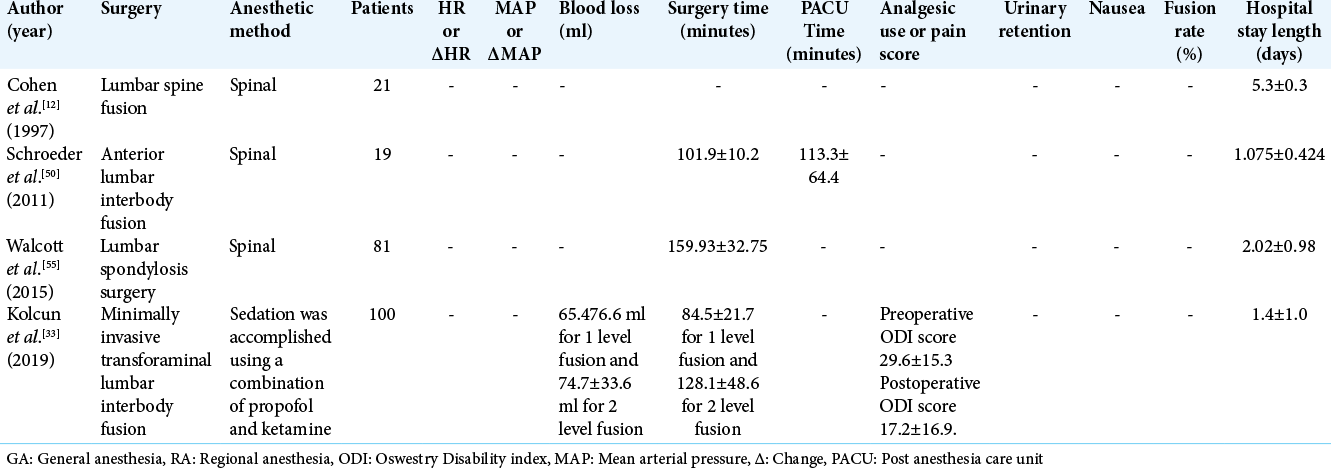
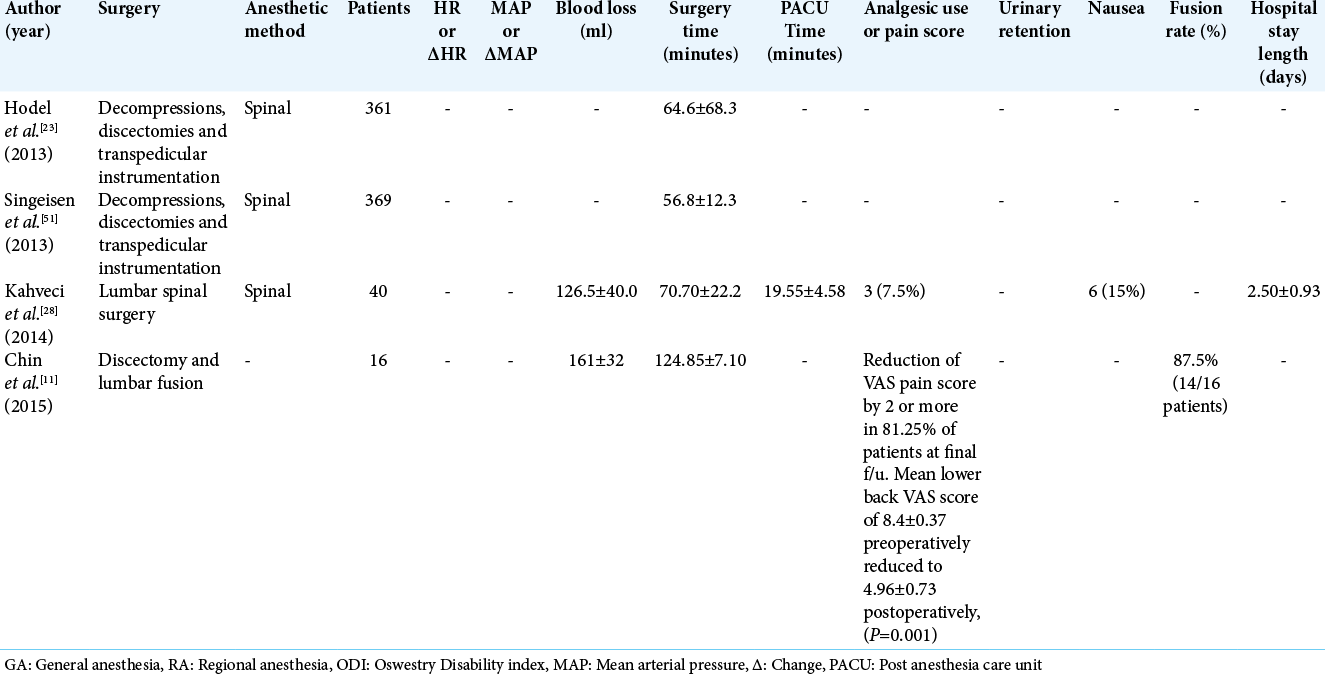
Awake spinal surgery is an alternative surgical technique with indications that increase the population of patients eligible for spinal procedures. There are procedures that were not listed previously, such as decompressions, that can be performed using awake protocols. The findings of these studies, along with multi-procedure data sets, are shown in [
CONTRAINDICATIONS
While the use of spinal anesthesia expands the patient population eligible for spinal surgery, it is still limited by contraindications of any surgical procedure. The option of spinal anesthesia is eliminated outright by patient’s refusal, coagulopathy, or infection within proximity of the surgical site.[
An operating complication of using spinal anesthesia is the occurrence of a hypotensive crisis during the procedure, and high-risk patients should considering pursuing other anesthetic options. Most notably, chronic alcohol consumption, or administration of spinal anesthesia in an acute setting, increases the occurrence of a hypotensive episode ×3 that of a patient with no risk factors. While individually these are not direct contraindications, combinations of these comorbidities increase the risk of a hypotensive episode and other pathologies that ultimately suggests the use of general anesthesia over localized.[
Other operational concerns stem from the short and often variable duration of action of local anesthetic, which can result in the patient feeling mild discomfort or pain during the procedure.[
ADVANTAGES AND LIMITATIONS
Awake spine surgery offers numerous benefits to the patient. The most glaring benefit is the elimination of general anesthesia and its associated risks and potential negative outcomes. General anesthesia is associated with side-effects such as postsurgery delirium, opioid use and bleeding complications, with further exacerbation in elderly patients and patients with multiple comorbidities.[
Neurosurgeons can also benefit greatly from utilizing awake methods for spine procedures. With patients awake, they are able to provide real-time feedback of any tension, discomfort, or neurologic sequelae due to operating in close proximity to neural structures.[
While there are many advantages to implementing awake spine procedures into practice, there are limitations that must be considered. Compared to general anesthesia, local anesthesia has a limited duration of action, thus narrowing the window of time to operate for the surgeon. In addition, this reduced time narrows the spectrum of possible surgical techniques that could be performed with local anesthesia.[
PATIENT SELECTION
Candidates for spinal anesthesia should be able to tolerate lying prone for the duration of the surgery and not indicate possible difficulties in airway management. Although there has been an extensive amount of research done on new techniques for awake spine surgery, there have been no direct studies to look at ideal candidates. For that reason, candidates should be selected with the limitations of these techniques in mind. Patients who are morbidly obese have a high BMI, have pre-existing respiratory issues (e.g., COPD or obstructive sleep apnea), should be excluded from the study. Furthermore, patients with pre-existing anxiety should also be excluded as they may be unable to tolerate the operation due to the unpleasant loud sounds produced by the instruments. Finally, due to the operative time limitation of local anesthetics, many types of spinal procedures at this time cannot be performed with this technique. For these reasons, the ideal candidate would be a patient with a healthy BMI, no respiratory issues, no pre-existing mental health issues (e.g., anxiety), and a nonsevere stenosis that requires operation on one or two spinal levels.[
CONCLUSION
In a field dominated by general anesthesia, “awake spine surgery” is a new method that utilizes regional anesthesia and minimally invasive surgical techniques. At present, the field of spinal surgery neglects to provide suitable options for patients who are otherwise not eligible for general anesthesia. However, awake spine surgery can attend to this patient population and make surgery more accessible to a wider patient population. Its advantages lie in its ability to provide live neural feedback during surgery and reduce the side effects associated with general anesthesia. Thus far, multiple studies have shown its ability to reduce surgical costs, postoperative stays and in-hospital complications while providing patients with an overall greater quality of life. Moving forward, future studies should focus on expanding the evidence available supporting this technique and defining its long-term efficacy. Larger cohort studies will be crucial in more narrowly defining its limitations and contraindications to ensure the safety of patients.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agarwal P, Pierce J, Welch WC. Cost analysis of spinal versus general anesthesia for lumbar diskectomy and laminectomy spine surgery. World Neurosurg. 2016. 89: 266-71
2. Alim SM, Hossain MM, Rahman MM, Roy SS, Chowdhury MS. Comparative study in prolapse lumbar intervertebral disc (PLID) surgery by spinal vs general anaesthesia. J Bangladesh Soc Anaesthesiol. 2014. 23: 47-50
3. Ames WA, Songhurst L, Gullan RW. Local anaesthesia for laminectomy surgery. Br J Neurosurg. 1999. 13: 598-600
4. Attari MA, Mirhosseini SA, Honarmand A, Safavi MR. Spinal anesthesia versus general anesthesia for elective lumbar spine surgery: A randomized clinical trial. J Res Med Sci. 2011. 16: 524-9
5. Bajwa SJ, Kulshrestha A. Anaesthesia for laparoscopic surgery: General vs regional anaesthesia. J Minim Access Surg. 2016. 12: 4-9
6. Basil GW, Wang MY. Trends in outpatient minimally invasive spine surgery. J Spine Surg. 2019. 5: S108-14
7. Bauer BA, Cutshall SA, Anderson PG, Prinsen SK, Wentworth LJ, Olney TJ. Effect of the combination of music and nature sounds on pain and anxiety in cardiac surgical patients: A randomized study. Altern Ther Health Med. 2011. 17: 16-23
8. Brown MJ. Anesthesia for Elective Spine Surgery in Adults. Available from: https://www.uptodate.com/contents/anesthesia-for-elective-spine-surgery-in-adults [Last accessed on 2020 October 30].
9. Chang HK, Kolcun JP, Chang PY, Wang MY. Enhanced recovery after surgery awake minimally-invasive transforaminal lumbar interbody fusion: 2-dimensional operative video. Oper Neurosurg (Hagerstown). 2019. 16: 519
10. Chen HT, Tsai CH, Chao SC, Kao TH, Chen YJ, Hsu HC. Endoscopic discectomy of L5-S1 disc herniation via an interlaminar approach: Prospective controlled study under local and general anesthesia. Surg Neurol Int. 2011. 2: 93
11. Chin KR, Coombs AV, Seale JA. Feasibility and patient-reported outcomes after outpatient single-level instrumented posterior lumbar interbody fusion in a surgery center: Preliminary results in 16 patients. Spine (Phila Pa 1976). 2015. 40: E36-42
12. Cohen BE, Hartman MB, Wade JT, Miller JS, Gilbert R, Chapman TM. Postoperative pain control after lumbar spine fusion. Patient-controlled analgesia versus continuous epidural analgesia. Spine (Phila Pa 1976). 1997. 22: 1892-6
13. Collins LM, Vaghadia H. Regional anesthesia for laparoscopy. Anesthesiol Clin North Am. 2001. 19: 43-55
14. Dagistan Y, Okmen K, Dagistan E, Guler A, Ozkan N. Lumbar microdiscectomy under spinal and general anesthesia: A comparative study. Turk Neurosurg. 2015. 25: 685-9
15. De Rojas JO, Syre P, Welch WC. Regional anesthesia versus general anesthesia for surgery on the lumbar spine: A review of the modern literature. Clin Neurol Neurosurg. 2014. 119: 39-43
16. Demirel CB, Kalayci M, Ozkocak I, Altunkaya H, Ozer Y, Acikgoz B. A prospective randomized study comparing perioperative outcome variables after epidural or general anesthesia for lumbar disc surgery. J Neurosurg Anesthesiol. 2003. 15: 185-192
17. Demirkol O, Ozlu O, Utebey G, Er U. Comparing total intravenous anesthesia and spinal anesthesia in lumbar spinal surgery. Anestezi Derg. 2009. 17: 186-90
18. Fabregas N, Craen RA. Anaesthesia for minimally invasive neurosurgery. Best Pract Res Clin Anaesthesiol. 2002. 16: 81-93
19. Falowski SM, Celii A, Sestokas AK, Schwartz DM, Matsumoto C, Sharan A. Awake vs. asleep placement of spinal cord stimulators: A cohort analysis of complications associated with placement. Neuromodulation. 2011. 14: 130-4
20. Garg B, Ahuja K, Sharan AD. Awake spinal fusion. J Clin Orthop Trauma. 2020. 11: 749-52
21. Greenbarg PE, Brown MD, Pallares VS, Tompkins JS, Mann NH. Epidural anesthesia for lumbar spine surgery. J Spinal Disord. 1988. 1: 139-43
22. Gu J, Hao C, Yan X, Xuan S. Applied analysis of ultrasound-guided ilioinguinal and iliohypogastric nerve blocks in the radical surgery of aged cervical cancer. Oncol Lett. 2017. 13: 1637-40
23. Hodel D, Singeisen H, Frey K, Schindler C, Eichenberger U, Hausmann ON. Spinal versus general anaesthesia for lumbar spine surgery: Patient characteristics and economic aspects. Eur J Anaesthesiol. 2013. 30: 129-9
24. Hussain Z, Ghaffar A, Mushtaq MJ, Qasmi SA. Can spinal anaesthesia be a routine for single level lumbar discectomy. Pak Armed Forces Med J. 2015. 65: 397-401
25. Inci K, Celik JB, Bahar OC, Apilliodullari S, Karabagli H. Comparison of spinal and general anesthesia in lumbar disc surgery. J Neurol Sci (Turkish). 2011. 28: 487-96
26. Ishikawa N, Watanabe G. Ultra-minimally invasive cardiac surgery: Robotic surgery and awake CABG. Surg Today. 2015. 45: 1-7
27. Jellish WS, Thalji Z, Stevenson K, Shea J. A prospective randomized study comparing short and intermediate-term perioperative outcome variables after spinal or general anesthesia for lumbar disk and laminectomy surgery. Anesth Analg. 1996. 83: 559-64
28. Kahveci K, Doger C, Ornek D, Gokcinar D, Aydemir S, Ozay R. Perioperative outcome and cost-effectiveness of spinal versus general anesthesia for lumbar spine surgery. Neurol Neurochir Pol. 2014. 48: 167-73
29. Kai-Hong Chan A, Choy W, Miller CA, Robinson LC, Mummaneni PV. A novel technique for awake, minimally invasive transforaminal lumbar interbody fusion: technical note. Neurosurg Focus. 2019. 46: E16
30. Karaman S. retrospective evaluation of anesthesia approaches for lumbar disc surgery. J Anesth Clin Res. 2014. 5: 402
31. Kaushal A, Haldar R. Regional anesthesia in neuroanesthesia practice. Discoveries (Craiova). 2020. 8: e111
32. Khan MB, Kumar R, Enam SA. Thoracic and lumbar spinal surgery under local anesthesia for patients with multiple comorbidities: A consecutive case series. Surg Neurol Int. 2014. 5: S62-5
33. Kolcun JP, Brusko GD, Wang MY. Endoscopic transforaminal lumbar interbody fusion without general anesthesia: Technical innovations and outcomes. Ann Transl Med. 2019. 7: S167
34. Lessing NL, Edwards CC, Dean CL, Waxter OH, Lin C, Curto RA. Spinal anesthesia for geriatric lumbar spine surgery: A comparative case series. Int J Spine Surg. 2020. 14: 713-21
35. Lin PC, Lin ML, Huang LC, Hsu HC, Lin CC. Music therapy for patients receiving spine surgery. J Clin Nurs. 2011. 20: 960-8
36. MacNeill AL, Mayich DJ. Wide-awake foot and ankle surgery: A retrospective analysis. Foot Ankle Surg. 2017. 23: 307-10
37. McLain RF, Bell GR, Kalfas I, Tetzlaff JE, Yoon HJ. Complications associated with lumbar laminectomy: A comparison of spinal versus general anesthesia. Spine (Phila Pa 1976). 2004. 29: 2542-7
38. McLain RF, Kalfas I, Bell GR, Tetzlaff JE, Yoon HJ, Rana M. Comparison of spinal and general anesthesia in lumbar laminectomy surgery: A case-controlled analysis of 400 patients. J Neurosurg Spine. 2005. 2: 17-22
39. McLain RF, Tetzlaff JE, Bell GR, Uwe-Lewandrowski K, Yoon HJ, Rana M. Microdiscectomy: Spinal anesthesia offers optimal results in general patient population. J Surg Orthop Adv. 2007. 16: 5-11
40. Meng T, Zhong Z, Meng L. Impact of spinal anaesthesia vs. general anaesthesia on peri-operative outcome in lumbar spine surgery: A systematic review and meta-analysis of randomised, controlled trials. Anaesthesia. 2017. 72: 391-401
41. Mitchell M. Patient anxiety and conscious surgery. J Perioper Pract. 2009. 19: 168-73
42. Morris MT, Morris J, Wallace C, Cho W, Sharan A, Abouelrigal M. An analysis of the cost-effectiveness of spinal versus general anesthesia for lumbar spine surgery in various hospital settings. Glob Spine J. 2019. 9: 368-74
43. Nicassio N, Bobicchio P, Umari M, Tacconi L. Lumbar microdiscectomy under epidural anaesthesia with the patient in the sitting position: A prospective study. J Clin Neurosci. 2010. 17: 1537-40
44. Papadopoulos EC, Huang RC, Girardi FP, Synnott K, Cammisa FP. Three-level anterior cervical discectomy and fusion with plate fixation: Radiographic and clinical results. Spine (Phila Pa 1976). 2006. 31: 897-902
45. Phan K, Kim JS, Kim JH, Somani S, Di’Capua J, Dowdell JE. Anesthesia duration as an independent risk factor for early postoperative complications in adults undergoing elective ACDF. Glob Spine J. 2017. 7: 727-34
46. Pierce JT, Kositratna G, Attiah MA, Kallan MJ, Koenigsberg R, Syre P. Efficiency of spinal anesthesia versus general anesthesia for lumbar spinal surgery: A retrospective analysis of 544 patients. Local Reg Anesth. 2017. 10: 91-8
47. Rung GW, Williams D, Gelb DE, Grubb M. Isobaric spinal anesthesia for lumbar disk surgery. Anesth Analg. 1997. 84: 1165-6
48. Sadrolsadat SH, Mahdavi AR, Moharari RS, Khajavi MR, Khashayar P, Najafi A. A prospective randomized trial comparing the technique of spinal and general anesthesia for lumbar disk surgery: A study of 100 cases. Surg Neurol. 2009. 71: 60-5
49. Sairyo K, Chikawa T, Nagamachi A. State-of-the-art transforaminal percutaneous endoscopic lumbar surgery under local anesthesia: Discectomy, foraminoplasty, and ventral facetectomy. J Orthop Sci. 2018. 23: 229-36
50. Schroeder KM, Zahed C, Andrei AC, Han S, Ford MP, Zdeblick TA. Epidural anesthesia as a novel anesthetic technique for anterior lumbar interbody fusion. J Clin Anesth. 2011. 23: 521-6
51. Singeisen H, Hodel D, Schindler C, Frey K, Eichenberger U, Hausmann ON. Significantly shorter anesthesia time for surgery of the lumbar spine: Process analytical comparison of spinal anesthesia and intubation narcosis. Anaesthesist. 2013. 62: 632-8
52. Tetzlaff JE, Dilger JA, Kodsy M, al-Bataineh J, Yoon HJ, Bell GR. Spinal anesthesia for elective lumbar spine surgery. J Clin Anesth. 1998. 10: 666-9
53. Ulutas M, Secer M, Taskapilioglu O, Karadas S, Akyilmaz AA, Baydilek Y. General versus epidural anesthesia for lumbar microdiscectomy. J Clin Neurosci. 2015. 22: 1309-13
54. Vural C, Yorukoglu D. Comparison of patient satisfaction and cost in spinal and general anesthesia for lumbar disc surgery. Turk Neurosurg. 2014. 24: 380-4
55. Walcott BP, Khanna A, Yanamadala V, Coumans JV, Peterfreund RA. Cost analysis of spinal and general anesthesia for the surgical treatment of lumbar spondylosis. J Clin Neurosci. 2015. 22: 539-43
56. Wang H, Ma L, Yang D, Wang T, Wang Q, Zhang L. Cervical plexus anesthesia versus general anesthesia for anterior cervical discectomy and fusion surgery: A randomized clinical trial. Medicine (Baltimore). 2017. 96: e6119
57. Wang MY, Grossman J. Endoscopic minimally invasive transforaminal interbody fusion without general anesthesia: Initial clinical experience with 1-year follow-up. Neurosurg Focus. 2016. 40: E13
58. Yıldırım Güçlü C, Kecik Y, Yörükoğlu D, Attar A. Neuroendocrine and hemodynamic effects of general anesthesia and spinal anesthesia for minimally invasive lumbar disc surgery: A randomized trial. J Neurol Sci. 2014. 31: 586-95