- Department of Neuroscience, King Abdulaziz Medical City, National Guard Health Affairs, Jeddah, Saudi Arabia
- King Saud bin Abdulaziz University for Health Sciences, College of Medicine, Jeddah, Saudi Arabia
- College of Medicine, Jazan University, Jazan, Saudi Arabia
- College of Medicine, Qassim University, Qassim, Saudi Arabia,
- Department of Neurosurgery, University of Buckingham, Buckingham, United Kingdom,
- Department of Spine, King Fahad Medical City, National Neuroscience Institute, Riyadh, Saudi Arabia
- Department of Surgery, College of Medicine, King Saud University, Riyadh, Saudi Arabia.
Correspondence Address:
Abdulhadi Yahya Algahtani, Department of Neuroscience, King Abdulaziz Medical City, National Guard Health Affairs, Jeddah, Saudi Arabia.
DOI:10.25259/SNI_302_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abdulhadi Yahya Algahtani1, Alaa Adel Ashqar2, Fadi Abdu Munhish3, Ghaida Abdullah Albattah4, Wafa Mohammad Imran5, Mohammad M. Alshardan6, Fawaz S. Almotairi7. Awareness level of idiopathic normal pressure hydrocephalus among health-care providers. 05-Jul-2024;15:234
How to cite this URL: Abdulhadi Yahya Algahtani1, Alaa Adel Ashqar2, Fadi Abdu Munhish3, Ghaida Abdullah Albattah4, Wafa Mohammad Imran5, Mohammad M. Alshardan6, Fawaz S. Almotairi7. Awareness level of idiopathic normal pressure hydrocephalus among health-care providers. 05-Jul-2024;15:234. Available from: https://surgicalneurologyint.com/surgicalint-articles/12975/
Abstract
Background: Idiopathic normal pressure hydrocephalus (iNPH) is a disease that primarily affects the geriatric population. It was first introduced by Adams et al. in 1965. A gradual decline in cognitive function, urinary incontinence, and gait disturbances characterizes the disease. This condition is believed to be underdiagnosed, and awareness of such pathology is vital, as the treatment is very effective and can reverse the symptoms.
Methods: This questionnaire-based cross-sectional study aimed to assess awareness levels regarding iNPH among non-neuroscience healthcare providers in Saudi Arabia.
Results: A total of 269 healthcare providers participated in this study, with data collected through an online questionnaire. About 80.6% of the participants had heard of the disease, while 56.5% were aware of the disease symptomology. About 50% of physicians did not encounter iNPH patients in clinical practice. Previous clinical exposure to iNPH patients correlates significantly with an awareness of disease symptoms, investigation, treatment modalities, and outcome. Clinical experience positively impacts physicians’ awareness as it correlates with a better understanding of diagnostic methods and disease outcomes.
Conclusion: The study highlights the need for targeted educational interventions, especially among family physicians and general practitioners with no previous experience with iNPH patients, as well as interdisciplinary collaboration to address gaps in awareness and enhance early diagnosis of iNPH patients.
Keywords: Awareness, Idiopathic normal pressure hydrocephalus, Knowledge normal pressure hydrocephalus (NPH), Survey
INTRODUCTION
Idiopathic normal pressure hydrocephalus (iNPH) is a disease that affects the geriatric population.[
MATERIALS AND METHODS
Ethical approval
This study was approved by King Abdullah International Medical Research Center Institutional Review Board Study number: NRJ23J/040/02.
Design and setting
This is an observational cross-sectional online questionnaire-based study targeting physicians working in all specialties in Saudi Arabia. However, physicians specialized in neuroscience, dentists, pharmacists, nurses, physiotherapists, and medical students were excluded from the study. The selection of participants was done using the quota sampling technique. The questionnaire links were sent to each healthcare provider (WhatsApp) group. The composition of the questionnaire provided was identical across all links. Following the distribution of the questionnaire through links provided in WhatsApp groups, participants had the option to participate or decline voluntarily.
Moreover, participants could view the link’s content before clicking and participating as a brief introduction of the aims and objectives of the study is displayed alongside the link provided in the WhatsApp groups. After clicking on the link, participants can review the aims and objectives of the study again, as well as the authors involved. Following that, they will need to confirm their participation in the study and choose either “agree” to continue with the study or “disagree,” in either case, the participants’ identity will remain anonymous. The data were collected from September 2023 to December 2023. The desirable sample size was calculated to be 384 through the Sample Size Calculator by Raosoft, Inc. A confidence interval of 95% was implanted for the calculation, with a margin of error of 5%, a population proportion of 50%, and an estimated total population of 228,717.
Questionnaire
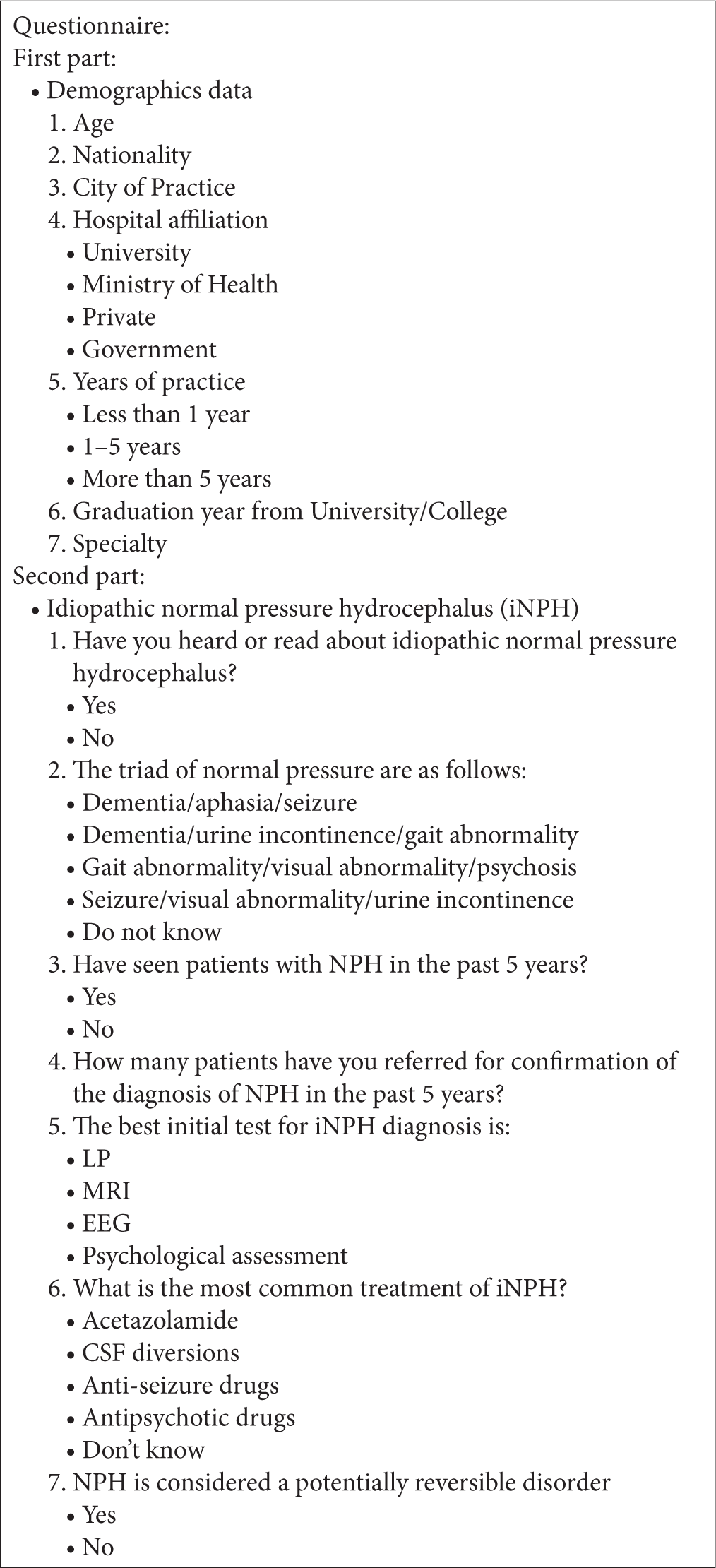
Fifteen neuroscience consultants with experience in diagnosing and treating iNPH patients were asked to review the questionnaire elements [
Data analysis
Data entry was conducted by the researchers on an Excel file. Afterward, data were transferred to the Statistical Package for the Social Sciences software version 20.0 for analysis. Mean and standard deviation were used to describe variables that are normally distributed, while median and interquartile range were used to describe variables that are skewed. Shapiro-Wilk test was used to assess the normality. To estimate the association between demographics and awareness of normal pressure hydrocephalus (NPH), the Chi-square test was used (Fisher’s exact test was used when the event rate was 5 or less). Statistical significance was considered at P < 0.05.
RESULTS
Descriptive analysis of demographics
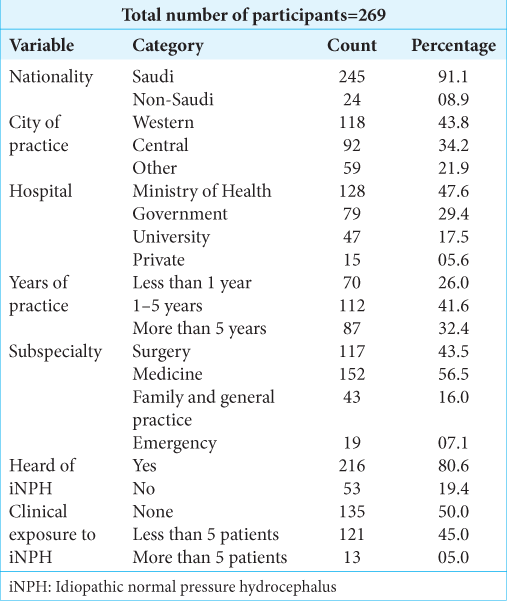
Two hundred and sixty-nine participants participated in the study, representing 70% of the calculated sample size of 384. Out of these, 245 were Saudi, and 216 had heard about iNPH. The majority of the participants, 118, were from the Western region. The healthcare providers who participated mainly worked at Ministry of Health hospitals, with 128 participants having 1–5 years of clinical experience. Medicine was the dominant specialty, with 152 participants. Notably, 135 participants did not see a patient of iNPH in their practical clinical experience. The study found that 80.4% of participants had heard about iNPH, while 56.5% of the physicians were aware of the typical clinical presentations of iNPH. About 76.2% were aware of the disease outcomes. About 52.4% of the participants were aware of diagnostic modalities, and 43.5% were aware of treatment modalities [
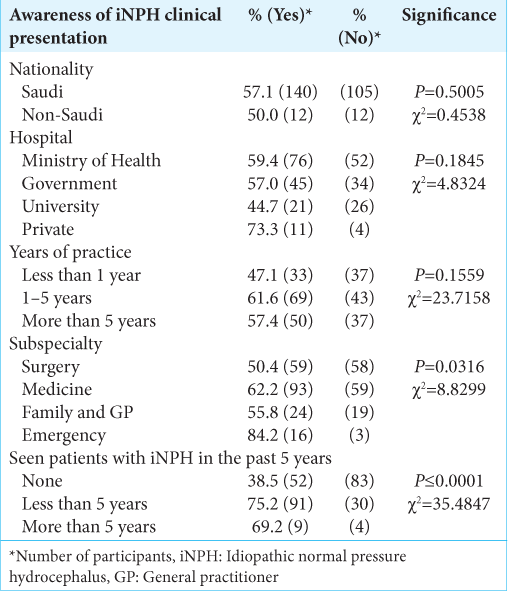
Awareness of iNPH clinical presentation
There was no significant difference in awareness between Saudi and non-Saudi participants (P = 0.5, χ2=0.4538). Similarly, there was no statistically significant difference in awareness among different types of hospitals (P = 0.1845, χ2 = 4.8324) or across different years of practice (P = 0.1559, χ2 = 23.7158). However, there was a significant difference in awareness across different subspecialties, with 54.3% of those in medicine, 50% in surgery, 55.8% in family medicine/general practice, and 84.2% in emergency medicine indicating awareness (P = 0.0316, χ2 = 8.8299). Clinical exposure to iNPH also influenced awareness; there was a significant difference among those who have seen patients with iNPH in the past 5 years (P < 0.0001, χ2 = 35.4847) [
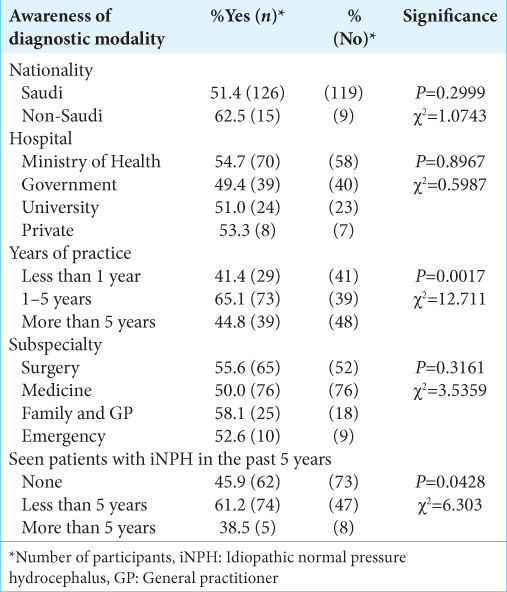
Awareness of diagnostic modality
The study found no significant difference in awareness between Saudi and non-Saudi participants (P = 0.2999, χ2 = 1.0743). Similarly, there was no significant difference in awareness across different types of hospitals (P = 0.8967, χ2 = 0.5987) and different subspecialties (P = 0.3161, χ2 = 3.5359). However, the difference in awareness across different years of practice was statistically significant (P = 0.0017, χ2 = 12.711). Finally, the study found that the difference in awareness among those who have seen patients with NPH in the past 5 years was statistically significant (P = 0.0428, χ2 = 6.303) [
Awareness of treatment modalities
The study found no significant difference in awareness of treatment modalities of iNPH between Saudi and non-Saudi participants (P = 0.8499, χ2 = 0.0358). Regarding hospital affiliation, the difference in awareness across different types of hospitals was statistically significant (P = 0.0235, χ2 = 9.4835). Across years of practice the difference in awareness across different years of practice was not statistically significant (P = 0.0747, χ2 = 5.1894) among different subspecialties. The difference in awareness across different subspecialties was not statistically significant (P = 0.3302, χ2 = 3.4287). Finally, among those who had encountered patients with iNPH in the past 5 years, the difference in awareness among those who have seen patients with iNPH in the past 5 years was statistically significant (P < 0.0001, χ2 = 35.75) [
Awareness of iNPH prognosis
There was no significant difference in awareness between Saudi and non-Saudi participants (P = 0.517, χ2 = 0.4199). Similarly, there was no significant difference in awareness across different types of hospitals (P = 0.2381, χ2 = 4.2255). However, there was a statistically significant difference in awareness across different years of practice (P = 0.0285, χ2 = 7.1169). There was no significant difference in awareness among different subspecialties (P = 0.3076, χ2 = 3.6038). Finally, among those who had encountered patients with iNPH in the past 5 years, there was a statistically significant difference in awareness (P < 0.0001, χ2 = 20.38) [
DISCUSSION
iNPH is a diagnosis by exclusion;[
A meta-analysis showed the callosal angle’s high diagnostic performance in predicting iNPH, with a sensitivity of 91% and specificity of 93%. The same result was obtained by Evans’ index, which revealed a high sensitivity of 96% but a relatively low specificity of 83%. Both the callosal angle and Evans’ index revealed excellent interobserver agreement.[
CONCLUSION
We conclude that awareness levels regarding iNPH vary among healthcare workers in Saudi Arabia. Overall, there is moderate awareness, with notable disparities across professional groups. The study underscores the need for targeted educational interventions, especially among family physicians and general practitioners with no previous experience with iNPH patients, as well as interdisciplinary collaboration to address gaps in awareness and enhance early diagnosis of iNPH patients. The study contributes to the growing body of literature on iNPH awareness and highlights the importance of raising awareness among healthcare providers to improve diagnostic accuracy and patient outcomes.
Ethical approval
The research/study was approved by the Institutional Review Board at King Abdullah International Medical Research Center (KAIMRC), number IRB/2360/23, dated September 18, 2023.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgment
Our sincere gratitude to Prof. Abdulhakeem Jamjoom, Dr. Ahmed Lary, Khalid Alshuqaifi, and Abdulaziz Alkhoshi for their invaluable contributions and unwavering support throughout the preparation of this research.
References
1. Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH. Symptomatic occult hydrocephalus with normal cerebrospinal-fluid pressure: A treatable syndrome. N Engl J Med. 1965. 273: 117-26
2. Andersson J, Rosell M, Kockum K, Lilja-Lund O, Söderström L, Laurell K. Prevalence of idiopathic normal pressure hydrocephalus: A prospective, population-based study. PLoS One. 2019. 14: e0217705
3. Asmri MA, Almalki MJ, Fitzgerald G, Clark M. The public health care system and primary care services in Saudi Arabia: A system in transition. Eastern Mediterr Health J. 2020. 26: 468-76
4. Chen Z, Wang Y, Cao N, Chen C, Wang Y, Ru Y. A survey on normal-pressure hydrocephalus in Shanghai community health-care professionals in Yangpu Community Training Program for rehabilitation medicine. J Int Soc Phys Rehabil Med. 2019. 2: 151-8
5. Conn HO, Lobo FM. What do physicians know about normal pressure hydrocephalus and when did they know it? A survey of 284 physicians. Yale J Biol Med. 2008. 81: 19-29
6. Derya KA, Isik AT. Cerebrospinal fluid biomarkers for normal pressure hydrocephalus. Biomark Neuropsychiatry. 2023. 9: 100071
7. Forsberg L, editors. Outcomes of hydrocephalus ventriculoperitoneal shunt surgery at a rural hospital. 2022. p.
8. Giordan E, Palandri G, Lanzino G, Murad MH, Elder BD. Outcomes and complications of different surgical treatments for idiopathic normal pressure hydrocephalus: A systematic review and meta-analysis. J Neurosurg. 2018. 131: 1024-36
9. Ishida T, Murayama T, Kobayashi S. Current research of idiopathic normal pressure hydrocephalus: Pathogenesis, diagnosis and treatment. World J Clin Cases. 2023. 11: 3706
10. Molde K, Söderström L, Laurell K. Parkinsonian symptoms in normal pressure hydrocephalus: A population-based study. J Neurol. 2017. 264: 2141-8
11. Mori E, Ishikawa M, Kato T, Kazui H, Miyake H, Miyajima M. Guidelines for management of idiopathic normal pressure hydrocephalus. Neurol Med Chir (Tokyo). 2012. 52: 775-809
12. Park H. Y, Kim M, Suh C. H, Lee D. H, Shim W. H, Kim S. J. Diagnostic performance and interobserver agreement of the callosal angle and Evans’ index in idiopathic normal pressure hydrocephalus: a systematic review and meta-analysis. European radiology. 2021. 31: 5300-5311
13. Petrella G, Ciarlo S, Elia S, Piaz RD, Nucera P, Pompucci A. Idiopathic normal pressure hydrocephalus: The real social and economic burden of a possibly enormous underdiagnosis problem. Tomography. 2023. 9: 2006-15
14. Rigamonti D, Yasar S, Vivas-Buitrago T, Rigamonti K. Letter to our colleagues family practitioners, geriatricians, and radiologists to increase awareness regarding idiopathic normal pressure hydrocephalus. World Neurosurg. 2024. 181: e291-3
15. Thavarajasingam SG, El-Khatib M, Vemulapalli K, Iradukunda HA, Sajeenth Vishnu K, Borchert R. Radiological predictors of shunt response in the diagnosis and treatment of idiopathic normal pressure hydrocephalus: A systematic review and meta-analysis. Acta Neurochir. 2023. 165: 369-419
16. Toma AK, Papadopoulos MC, Stapleton S, Kitchen ND, Watkins LD. Systematic review of the outcome of shunt surgery in idiopathic normal-pressure hydrocephalus. Acta Neurochir. 2013. 155: 1977-80
17. Torsnes L, Blåfjelldal V, Poulsen FR. Treatment and clinical outcome in patients with idiopathic normal pressure hydrocephalus-a systematic review. Dan Med J. 2014. 61: A4911
18. Tullberg M, Persson J, Petersen J, Hellström P, Wikkelsø C, Lundgren-Nilsson Å. Shunt surgery in idiopathic normal pressure hydrocephalus is cost-effective-a cost utility analysis. Acta Neurochir. 2018. 160: 509-18
19. Wang Z, Zhang Y, Hu F, Ding J, Wang X. Pathogenesis and pathophysiology of idiopathic normal pressure hydrocephalus. CNS Neurosci Ther. 2020. 26: 1230-40
20. Williams MA, Malm J. Diagnosis and treatment of idiopathic normal pressure hydrocephalus. Continuum (Minneap Minn). 2016. 22: 579-99